Combined Oral Contraceptive Risk: Quick Guide
Combined oral contraceptives (COCs) are the pill most people think of when they talk about birth control. They mix estrogen and progestin to stop ovulation, and for many they work great. But like any medicine, they bring a set of risks you should know before you pop a pill every day.
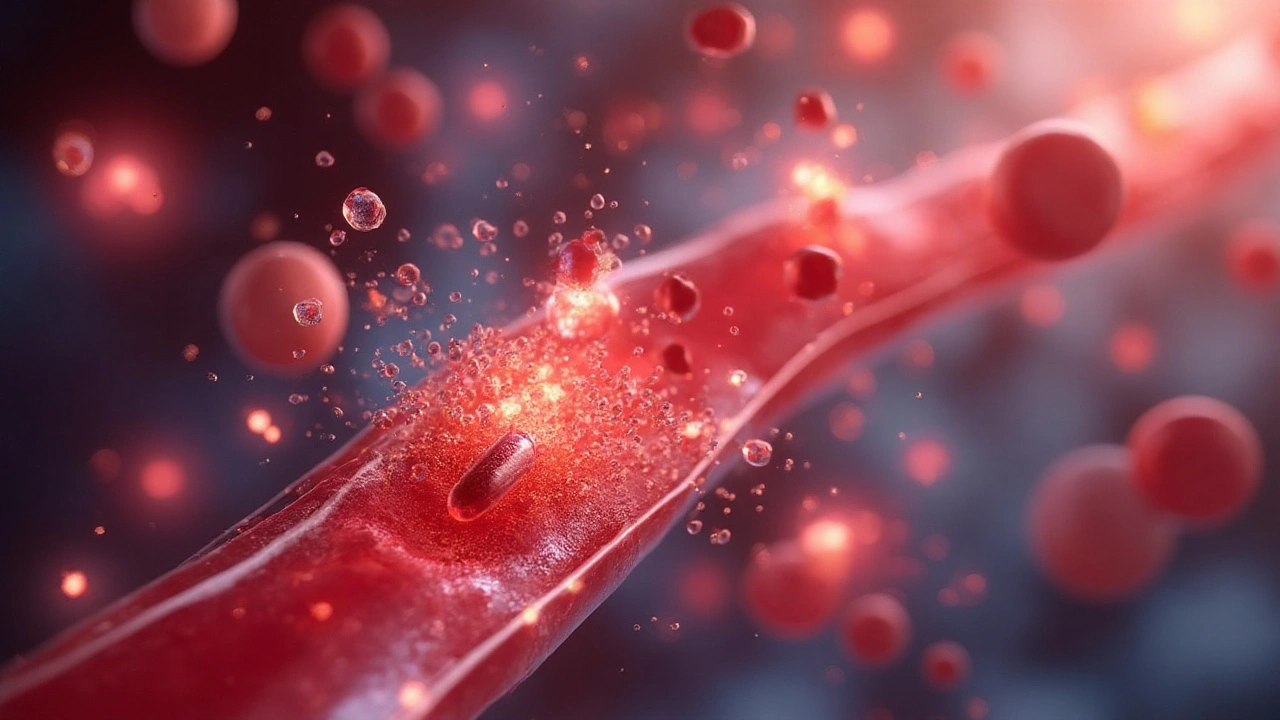
First off, the biggest red‑flag is blood clots. The estrogen in COCs can make blood a little stickier, which raises the chance of a clot forming in the leg (deep‑vein thrombosis) or even traveling to the lungs (pulmonary embolism). While the overall chance is low, it’s higher for smokers, people over 35, and those with a personal or family history of clotting disorders.
Next up are heart‑related issues. COCs can nudge blood pressure up and, in rare cases, trigger a stroke or heart attack. This is why doctors screen for hypertension, high cholesterol, or a history of heart disease before prescribing the pill.
Who Should Be Cautious?
If you’re over 35 and smoke, the combination of age and nicotine is a perfect storm for clots and heart events. Women with migraine headaches that come with visual aura should also steer clear, as estrogen can worsen those migraines and increase stroke risk.
Other red‑lights include a past diagnosis of breast or liver cancer, uncontrolled diabetes, and certain genetic clotting disorders like Factor V Leiden. Even if you don’t fall into these categories, it’s wise to check your personal and family medical history with a doctor.
How to Lower Your Risk
The easiest step is to quit smoking. If you can’t quit cold turkey, talk to your doctor about nicotine‑replacement options. Staying active, maintaining a healthy weight, and keeping an eye on blood pressure also cut risk.
Regular check‑ups are key. Ask your doctor to check your blood pressure at every visit and discuss any new symptoms—like calf pain, unexplained swelling, or sudden headaches. If you notice anything odd, don’t wait; get evaluated right away.
Consider lower‑dose estrogen pills or progestin‑only options if you have risk factors. Newer formulations use less estrogen, which can reduce clot risk while still preventing pregnancy effectively. Your doctor can help match the right pill to your health profile.
Lastly, keep a symptom diary. Jot down any mood swings, headaches, or breast changes. Hormones can affect mood, and tracking what you feel helps your provider adjust the prescription before problems grow.
Bottom line: COCs are safe for most people, but they’re not one‑size‑fits‑all. Knowing the risks, staying honest with your doctor, and making lifestyle tweaks can keep you protected while you enjoy reliable birth control.