Heartburn Medication Selector
Personalized Heartburn Relief Guide
Answer a few questions to find the most appropriate heartburn medication for your situation.
When the acid in your stomach decides to climb up the food pipe, the burning feeling can ruin a dinner or a night out. Heartburn medication is a type of drug that neutralises or reduces that acid, giving you quick relief and protecting your esophagus in the long run.
What exactly is heartburn?
Heartburn is the painful, sour sensation that occurs when stomach acid backs up into the lower esophagus. It’s often a symptom of gastroesophageal reflux disease (GERD), but occasional episodes happen to most people after a big meal, spicy food, or late‑night snacking.
How do medications tame the burn?
Most antacids work by directly neutralising stomach acid for fast relief. Others, like proton pump inhibitors (PPIs) block the stomach’s acid‑producing pumps, lowering overall acid levels. A third group, H2 receptor antagonists reduce the amount of acid the stomach releases, sits between antacids and PPIs in speed and duration.
Over‑the‑counter (OTC) options you can pick up today
OTC products are perfect for occasional flare‑ups or for people who want to avoid a doctor’s visit. Here’s a quick rundown of the most common classes:
- Calcium carbonate (e.g., Tums, Rolaids) - a fast‑acting antacid that also supplies calcium. Works within minutes and lasts 30‑60 minutes.
- Magnesium hydroxide (e.g., Milk of Magnesia) - neutralises acid and can double as a mild laxative, useful if constipation accompanies reflux.
- Alginate‑based formulas (e.g., Gaviscon) - create a foam barrier that floats on stomach contents, preventing acid from reaching the esophagus.
- Low‑dose H2 blockers such as famotidine (Pepcid AC) - start working within an hour, offering relief that lasts up to 12 hours.
These meds are generally safe for adults, but it’s worth checking the label if you’re pregnant, nursing, or have kidney problems.
Prescription‑strength solutions for frequent or severe symptoms
If heartburn knocks you out a few times a week, or if you’ve been diagnosed with GERD, a doctor may prescribe stronger drugs. The main categories are:
- Proton pump inhibitors (PPIs) such as omeprazole, esomeprazole, and lansoprazole - they shut down acid production at its source, providing 24‑hour relief after a few days of consistent use.
- Higher‑dose H2 blockers like famotidine 20 mg taken twice daily - useful for night‑time symptoms when a longer‑acting antacid isn’t enough.
- Prokinetics such as metoclopramide, which help the stomach empty faster, reducing pressure that pushes acid upward - reserved for specific cases because of possible side effects.
Doctors might combine a PPI with an alginate for extra protection during severe flare‑ups.
OTC vs. prescription: a side‑by‑side look
| Feature | OTC Options | Prescription Options |
|---|---|---|
| Typical active ingredient | Calcium carbonate, Magnesium hydroxide, Alginate, Low‑dose H2 blocker | PPIs (omeprazole, esomeprazole), High‑dose H2 blocker, Prokinetic |
| Onset of relief | 5-30 minutes | 1-2 hours (PPIs need 2-3 days for full effect) |
| Duration of action | 1‑2 hours (antacids) / up to 12 hours (H2 blocker) | 12‑24 hours (PPIs) |
| Need for doctor’s note | No | Yes |
| Common side effects | Gas, constipation, mild taste alteration | Headache, nutrient malabsorption, risk of bone fracture with long‑term use |
How to pick the right medication for you
Think of the decision as a checklist:
- Frequency: Occasional (once or twice a month) → start with an antacid or alginate.
Frequent (several times a week) → consider an H2 blocker. - Severity: If the burn lasts longer than 30 minutes or wakes you at night, you likely need a prescription‑strength PPI.
- Other health conditions: Kidney disease, heart failure, or pregnancy can limit which ingredients are safe.
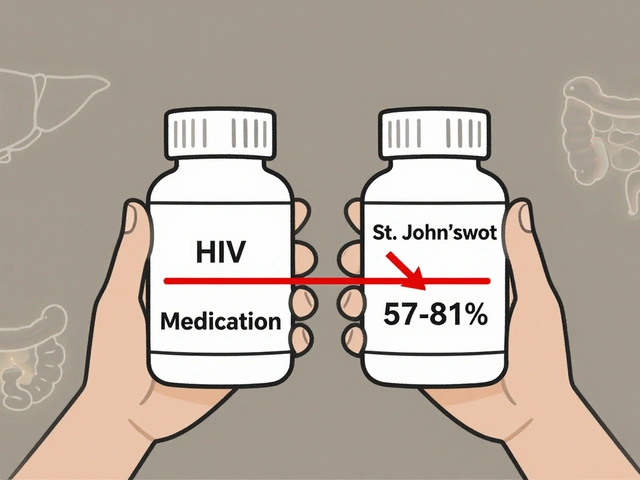
- Drug interactions: PPIs can affect the absorption of certain antibiotics and blood thinners; always cross‑check with your pharmacist.
- Long‑term plan: Use the lowest effective dose for the shortest time. If you need a PPI for more than 8 weeks, ask your doctor about stepping down to an H2 blocker.
Recording when symptoms occur, what you ate, and which medication you tried can help your doctor tailor a plan that balances relief with safety.
Safety tips and pitfalls to avoid
Even “easy” meds can cause trouble if misused. Here are the most common warnings:
- Over‑use of antacids: Taking more than the label recommends can lead to high calcium levels or kidney stones.
- Long‑term PPI use: Studies link it to higher risk of C. diff infection, vitamin B12 deficiency, and osteoporosis. Schedule a review after 3‑6 months.
- Mixing meds: Avoid taking antacids within two hours of certain antibiotics (e.g., tetracycline) as they bind and reduce absorption.
- Self‑diagnosis: Persistent pain, difficulty swallowing, or weight loss could signal an ulcer or esophageal cancer-see a doctor promptly.
Quick reference cheat‑sheet
- Burn lasts < 5 minutes? Try a calcium carbonate antacid.
- Burn lasts 30‑60 minutes? Add an alginate or low‑dose H2 blocker.
- Burn keeps coming back >2 times/week? Book a GP appointment for a possible PPI prescription.
- Need nightly relief? Discuss a low‑dose PPI or bedtime H2 blocker with your doctor.
- Any red‑flag symptoms (bleeding, severe pain, vomiting)? Seek urgent care.
Frequently Asked Questions
Can I combine an antacid with a prescription PPI?
Yes. An antacid or alginate can be taken between PPI doses to cover breakthrough symptoms, but avoid taking them within an hour of the PPI to ensure the PPI can work properly.
Are there any OTC heartburn meds safe for pregnancy?
Calcium carbonate (e.g., Tums) is generally considered safe during pregnancy, but always check with your midwife before starting any regular use.
How long can I stay on a PPI?
Short‑term (4‑8 weeks) is typical for most reflux cases. If you need longer, your doctor should monitor bone density, vitamin B12, and kidney function.
What’s the difference between a PPI and an H2 blocker?
PPIs block the final step of acid production, giving stronger and longer relief, while H2 blockers reduce the amount of acid released and work faster but for a shorter period.
Can lifestyle changes replace medication?
Often yes. Losing weight, avoiding late meals, limiting caffeine and alcohol, and elevating the head of the bed can cut down the need for meds, but medication may still be needed during flare‑ups.



Comments
4 Comments
Tiffany Davis
I appreciate the clear breakdown of OTC versus prescription options; it's helpful to see the onset and duration side by side.
Don Goodman-Wilson
Oh great, another fluffy summary. If you actually wanted relief you'd just grab the strongest PPI and stop reading these fluff pieces.
Bret Toadabush
They don't tell you that the big pharma lords push PPIs so they can keep us hooked on pricey meds. The real fix is simple diet changes, but they hide it.
Iris Joy
When you’re dealing with that burning feeling, start by tracking what you eat and when the symptoms hit. A simple food diary can reveal triggers like spicy meals, caffeine, or late‑night snacks. If occasional, an antacid or alginate does the trick in minutes. For more frequent flare‑ups, an H2 blocker taken before meals can smooth things out without jumping straight to a prescription. Remember to stay upright after eating and avoid tight clothing that presses on the stomach. Hydration helps, but sip water rather than gulp large amounts that can distend the stomach. Also, consider modest weight loss if you’re carrying extra pounds; even a few kilos can lower abdominal pressure. Finally, keep a low‑dose PPI handy for nights when the burn keeps you awake, but aim to step down after a few weeks.
Write a comment