INR Risk Assessment Tool
Enter Your INR Value
Results
Enter your INR value to see risk assessment
When you're on a blood thinner like warfarin, your life depends on a single number: your INR. It's not just a lab result-it's the difference between a clot that could cause a stroke and a bleed that could send you to the ER. Many people think taking a daily pill is enough. But without regular INR checks, that pill could be doing more harm than good.
What Is INR, and Why Does It Matter?
INR stands for International Normalized Ratio. It's a standardized way to measure how long it takes your blood to clot. This number tells your doctor whether your warfarin dose is too high, too low, or just right. Before INR was developed in 1983, every lab used different methods to measure clotting time. One hospital’s "normal" could be another’s danger zone. That inconsistency led to dangerous dosing errors. INR fixed that. Now, whether you're tested in a hospital in Chicago or a clinic in rural Alabama, a result of 2.5 means the same thing everywhere.
For someone not on blood thinners, the normal INR is 1.0. That’s your baseline. But if you have atrial fibrillation, a mechanical heart valve, or a history of blood clots, your target range is higher. Most people aim for 2.0 to 3.0. That’s the sweet spot-low enough to avoid clots, high enough to prevent dangerous bleeding. Some conditions need tighter control. For example, people with mechanical mitral valves often need an INR between 2.5 and 3.5. Miss that target by even 0.5, and your risk of complications jumps.
How Often Should You Test Your INR?
When you first start warfarin, you might need testing every few days. Your body reacts differently to the drug than anyone else’s. Doctors adjust your dose based on each result until they find the right balance. Once you're stable, most people switch to testing once a month. But "stable" doesn’t mean "set and forget." Many patients get tested too often. A 2021 study found that 38% of people on warfarin had weekly tests even though their INR hadn’t changed in months. That’s unnecessary stress, extra costs, and more needle pokes for no reason.
On the flip side, going too long between tests is just as risky. If you skip a check for six weeks, your INR could drift out of range without you knowing. A rise above 4.9 increases your chance of major bleeding by 27% for every 0.5-point increase. A drop below 1.5 means your blood is clotting too fast. That’s when clots form-leading to strokes, heart attacks, or pulmonary embolisms. The American Heart Association says hospitals with over 65% time in therapeutic range (TTR) have 42% fewer strokes. That’s not luck-it’s consistency.
Home Testing: Convenience or Risk?
Home INR testing has changed the game. Devices like the Abbott Acelis and Roche CoaguChek let you prick your finger, drop a tiny drop of blood on a strip, and get a result in under a minute. No more waiting 24 to 48 hours for lab results. No more missing work or driving across town in bad weather. Studies show patients who test at home stay in their target range 72% of the time-compared to just 58% for clinic-based testing. That means 34% fewer clots and 21% fewer major bleeds.
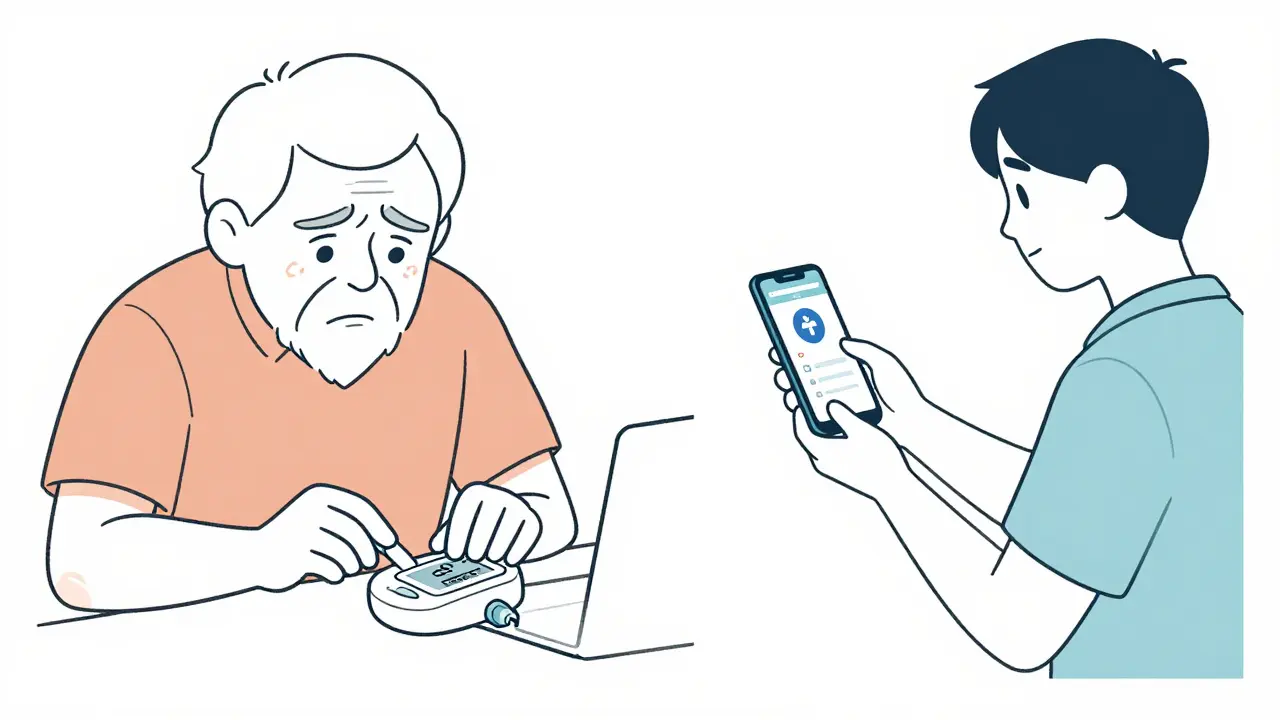
But it’s not for everyone. The FDA says 25-30% of patients can’t use home devices because of shaky hands, poor eyesight, or trouble following steps. Elderly patients under 65 rate home testing at 4.3 out of 5. Those over 65? Only 3.1. One user on Reddit said, "After three years, I still miss the capillary tube one in five tests. I waste $6 each time." That’s not just money-it’s frustration. If you’re not confident in your technique, stick with clinic visits.
Cost is another factor. Medicare covers 100% of home INR testing for eligible patients. But private insurers? They often require 20% coinsurance. With strips costing $5.99 each and testing twice a week, that’s over $600 a year out of pocket. Some patients pay more for testing than they do for the warfarin itself.
What Your INR Numbers Really Mean
Let’s break down what each number means in real terms:
- INR below 1.5: Your blood is clotting too fast. You’re at risk for stroke, heart attack, or deep vein thrombosis. Call your doctor immediately.
- INR 2.0-3.0: The standard target for most conditions like atrial fibrillation or DVT. This is where you want to stay.
- INR 3.0-4.0: Higher than ideal. You’re at increased bleeding risk. Your doctor may lower your dose.
- INR above 4.9: Dangerous. Major bleeding risk spikes. You may need to skip your next dose and get emergency care.
- INR above 5.0: Medical emergency. Hold your warfarin. Contact your provider within 24 hours.
There’s no wiggle room here. Every 0.5-point increase above 3.0 adds 27% more bleeding risk. That’s why timing matters. Test in the morning, after fasting for 4-6 hours. Vitamin K in your food, alcohol, or even a change in your daily routine can swing your result. Consistency is your best defense.
Warfarin vs. Newer Blood Thinners
When warfarin was the only option, INR monitoring was non-negotiable. Today, newer drugs like apixaban, rivaroxaban, and dabigatran don’t require regular blood tests. They’re easier. But they’re not better for everyone.
Warfarin still has a critical role. If you have a mechanical heart valve-especially a mitral valve-DOACs won’t work. You must take warfarin. That’s about 200,000 Americans right there. Warfarin also stays the go-to for patients with severe kidney disease. And cost? Warfarin runs about $4 a month. DOACs? $550-$650. That’s a huge difference if you’re paying out of pocket.
But here’s the trade-off: DOACs have a much wider safety window. You can miss a dose, eat a big salad, or drink a glass of wine without a major risk. With warfarin, even small changes can throw your INR off. That’s why the American College of Chest Physicians now recommends home testing as first-line for all eligible patients. It’s not about preference-it’s about safety.

What to Do If Your INR Is Off
When your INR is too high or too low, don’t panic. But don’t ignore it either.
If your INR is below 1.5: Contact your provider right away. You may need a higher dose or a temporary change in diet.
If your INR is above 5.0: Skip your next warfarin dose. Call your doctor. They may give you vitamin K to reverse the effect. Don’t wait until morning. Bleeding can happen suddenly.
If your INR is stuck in the 3.0-4.0 range for two tests in a row: Your dose likely needs adjustment. Your provider may reduce it by 10-25%. Don’t try to adjust it yourself.
Keep a log. Write down your INR results, your dose, what you ate, and how you felt. Patterns matter. A sudden rise after eating a lot of spinach? That’s vitamin K. A drop after switching to a new antibiotic? That’s a drug interaction. Your doctor can’t help if you don’t give them the full picture.
Future of INR Monitoring
The future is connected. In January 2023, the FDA approved the first smartphone-linked INR monitor. Results now auto-send to your doctor. No more forgotten calls or lost paperwork. A 2022 Mayo Clinic trial showed AI tools predicting the right warfarin dose with 83% accuracy. That’s huge. But it’s not replacing human care-it’s supporting it.
Still, challenges remain. Only 35% of rural clinics offer full anticoagulation services. That’s compared to 82% in cities. People in remote areas are falling through the cracks. And while DOACs are growing fast-projected to make up 85% of new prescriptions by 2028-warfarin isn’t going away. For some, it’s still the only safe choice.
The bottom line? INR monitoring isn’t optional. It’s life-saving. Whether you test at home or in a clinic, staying in your target range is the single most important thing you can do to stay healthy on warfarin. Don’t treat it like a chore. Treat it like your lifeline.