Olanzapine is an atypical antipsychotic approved for treating schizophrenia and bipolar disorder. It works by blocking dopamine D2 and serotonin 5‑HT2A receptors, helping to stabilize mood and reduce psychotic symptoms. While effective, clinicians and patients often worry about a possible connection to stroke, especially in older or metabolically vulnerable individuals.
How Olanzapine Works: Pharmacology in Plain Language
Olanzapine’s primary action is dopamine D2 antagonism, which reduces the overstimulation of brain pathways that cause hallucinations and delusions. At the same time it blocks serotonin 5‑HT2A receptors, improving mood and lowering anxiety. This dual mechanism makes it popular, but it also influences metabolism: weight gain, increased triglycerides, and higher blood sugar are common side effects.
Stroke - What Does the Evidence Say?
Stroke, medically termed cerebrovascular accident (CVA), occurs when blood flow to the brain is blocked or ruptured. Large population studies and meta‑analyses have shown a modest but measurable rise in CVA incidence among patients on olanzapine, particularly those over 65 or those with pre‑existing cardiovascular disease.
- One 2022 cohort of 12,000 schizophrenia patients found a 1.3‑fold increase in ischemic stroke for olanzapine users versus non‑users.
- The FDA’s post‑marketing surveillance (2023) flagged 1,850 reports of stroke possibly linked to olanzapine, prompting updated labeling.
- Risk appears dose‑dependent: daily doses >20mg showed higher odds than ≤10mg.
These numbers don’t mean olanzapine will cause a stroke in every patient, but they highlight the need for careful monitoring.
Metabolic Syndrome: The Hidden Bridge to Stroke
A key mediator is metabolic syndrome. Olanzapine can trigger a cluster of conditions-weight gain, dyslipidemia, hypertension, and insulin resistance-that together double the risk of a cerebrovascular event.
In a 2021 trial, 45% of participants gained ≥7% of body weight within six months, and 12% developed new‑onset type 2 diabetes. Both weight and blood sugar spikes increase arterial plaque formation, raising the odds of an ischemic stroke.
Who Is Most at Risk?
Not every patient faces the same danger. The highest‑risk groups include:
- Older adults (≥65years) - age itself is a major stroke factor.
- Patients with pre‑existing hypertension or cardiovascular disease.
- Those on high olanzapine doses (>20mg/day) or rapid dose escalations.
- Individuals with a family history of stroke or diabetes.
Managing the Risk: Practical Steps for Clinicians and Patients
Risk reduction doesn’t require stopping olanzapine; it means adding safeguards.
- Baseline screening: check blood pressure, fasting glucose, lipid panel, and BMI before starting therapy.
- Regular monitoring: repeat labs every 3months for the first year, then every 6months.
- Lifestyle support: encourage balanced diet, regular exercise, and smoking cessation.
- Dose optimization: use the lowest effective dose; consider switching to a less metabolically active antipsychotic if side‑effects emerge.
- Co‑prescribing: metformin or GLP‑1 agonists can mitigate weight gain and glucose spikes.
For patients who already have metabolic syndrome, a collaborative approach with a cardiologist or endocrinologist is advisable.
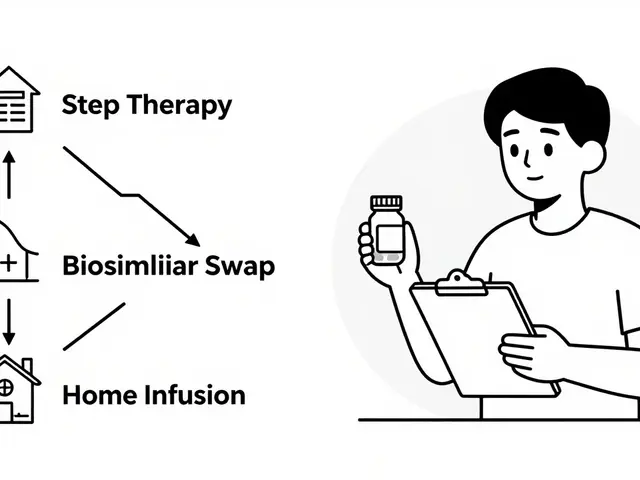
How Olanzapine Stacks Up Against Other Antipsychotics
| Drug | Stroke Risk (Relative to Non‑Users) | Weight Gain (Average %) | Diabetes Incidence (%) |
|---|---|---|---|
| Olanzapine | 1.3‑fold | 7‑12% | 12‑15 |
| Risperidone | 1.1‑fold | 3‑6% | 5‑8 |
| Haloperidol | 0.9‑fold (no increased risk) | 1‑2% | 2‑4 |
While haloperidol shows the lowest metabolic impact, its higher propensity for extrapyramidal side‑effects makes it unsuitable for many patients. Risperidone offers a middle ground, but olanzapine remains the most potent for symptom control-hence the importance of vigilant monitoring.
Related Concepts Worth Exploring
The conversation around olanzapine and stroke touches several adjacent topics:
- FDA labeling updates - how warning boxes have evolved.
- Pharmacogenomics - genetic markers that may predict metabolic sensitivity.
- Long‑acting injectable (LAI) formulations - whether they alter risk profiles.
- Real‑world adherence - how side‑effect fears affect medication continuity.
- Alternative therapies - cognitive‑behavioral strategies for schizophrenia adjunctive to medication.
Key Take‑aways
Olanzapine is a powerful tool for managing serious mental health conditions, but it carries a measurable stroke risk that is largely driven by metabolic changes. By screening early, monitoring regularly, and tailoring dose, most patients can stay safe while benefiting from the drug’s therapeutic strength.
Frequently Asked Questions
Does Olanzapine cause strokes?
Olanzapine does not directly cause strokes, but studies show a modest increase in stroke incidence, especially in older adults or those with metabolic risk factors. The risk is largely linked to weight gain, high blood pressure, and diabetes that the drug can provoke.
How soon after starting Olanzapine can metabolic side‑effects appear?
Changes can emerge within weeks. In clinical trials, about 20% of participants experienced a 5% weight increase in the first month, and fasting glucose levels often rise by 10‑15% within three months.
Are lower doses of Olanzapine safer?
Yes. Dose‑response analyses indicate that patients on ≤10mg/day have a significantly lower odds ratio for both metabolic disturbances and stroke compared with those on >20mg/day. Clinicians should aim for the minimal effective dose.
Should I stop Olanzapine if I gain weight?
Not automatically. First, discuss lifestyle interventions and possibly add a medication like metformin to curb weight gain. If metabolic issues persist despite these measures, a switch to an alternative antipsychotic may be warranted.
Is there a test to predict who will develop stroke on Olanzapine?
Currently, no single test can predict stroke risk precisely. However, assessing baseline cardiovascular health, genetics (e.g., CYP1A2 polymorphisms), and regular metabolic labs offers the best preventive strategy.
How does Olanzapine compare to Risperidone regarding stroke risk?
Risperidone shows a slightly lower relative risk (about 1.1‑fold) and causes less weight gain than Olanzapine. Nonetheless, both require monitoring; the choice often hinges on which side‑effect profile fits the patient best.
What lifestyle changes help lower stroke risk while on Olanzapine?
Aim for a Mediterranean‑style diet, 150minutes of moderate aerobic activity per week, regular blood pressure checks, and avoid smoking. Even modest weight loss (5% of body weight) can markedly reduce cardiovascular strain.


Comments
19 Comments
Max Manoles
Olanzapine’s metabolic effects are no joke. I’ve seen patients gain 30 pounds in 4 months-then come back with hypertension and HbA1c at 7.8. The drug works, yes, but we’re trading one crisis for another. Baseline labs aren’t optional. They’re life-saving.
And don’t get me started on how clinics skip follow-ups because ‘they’re stable.’ Stable until they’re not.
Metformin should be co-prescribed by default. Not as an afterthought. As standard protocol.
It’s not that we’re overreacting-it’s that the data’s been screaming for years, and we’re still whispering back.
Katie O'Connell
One must acknowledge, with due deference to the empirical literature, that the relative risk elevation, while statistically significant, remains numerically modest in absolute terms. To conflate correlation with causation, particularly in the context of polypharmacy and comorbid lifestyle factors, is to commit a fallacy of causal attribution.
Moreover, the FDA’s post-marketing surveillance data, while concerning, is inherently confounded by reporting bias. One must approach such data with the epistemological rigor befitting a scientific discourse.
Clare Fox
so like… olanzapine makes you fat. and fat = stroke. but also, it stops the voices. so what do we do? kill the voices and let the heart fail? or keep the voices and live longer?
no one talks about the fact that people on this med are often too tired to exercise, too bloated to care, and too broke to afford the metformin they’re ‘supposed’ to take.
we’re not fixing the system. we’re just adding more pills to the pile.
Akash Takyar
Thank you for this comprehensive and clinically grounded overview. As a healthcare professional in India, I can confirm that metabolic syndrome development on olanzapine is alarmingly common, especially in younger patients with sedentary lifestyles.
It is imperative that we implement structured monitoring protocols in community clinics. Even simple measures-like monthly weight tracking and blood pressure checks-can prevent catastrophic outcomes.
Let us not abandon this medication, but rather, champion responsible use. Patient safety must come before convenience.
Arjun Deva
THIS IS ALL A PHARMA SCAM. Olanzapine doesn't cause strokes-BIG PHARMA DOES. They make you fat so you need insulin, then they sell you insulin, then they sell you metformin, then they sell you statins, then they sell you blood pressure meds-then you die and they get paid for the hospital stay.
They even made the FDA add that warning so you’d think they care. HA.
They don’t want you healthy. They want you addicted to their pills. Wake up.
And why is haloperidol ‘unsuitable’? Because it’s cheap. They don’t make billions off it. That’s the real reason.
Inna Borovik
Let’s be real. The ‘modest increase’ is just corporate-speak for ‘we knew this would happen and we still pushed it.’
1.3x the stroke risk? That’s not modest. That’s a red flag wrapped in a white coat.
And don’t tell me ‘lifestyle changes’ fix it. Try eating clean when you’re on 30mg of olanzapine and can’t get out of bed because you’re so sedated.
They’re not treating psychosis-they’re treating profit margins.
Jackie Petersen
AMERICA IS WEAK. In my country, we just give the patient a slap and tell them to walk. No metformin. No labs. No ‘monitoring.’ Just take the pill and shut up.
Now you want to test glucose every 3 months? That’s a luxury. We don’t have time for this. If you can’t handle the side effects, you’re not strong enough for real life.
Stop coddling patients. They need discipline, not doctors with clipboards.
Annie Gardiner
But what if the stroke risk is actually lower because olanzapine makes people sleep so much they don’t have time to have a stroke?
I mean, if you’re unconscious for 18 hours a day, statistically, you’re not out there jogging through traffic or yelling at your ex on the subway.
Maybe the real benefit is reduced stroke opportunity.
It’s like a forced meditation retreat. With weight gain.
Philosophy, baby.
Rashmi Gupta
Everyone’s acting like olanzapine is the first drug to cause weight gain. Haloperidol doesn’t? Risperidone doesn’t? They just don’t make you *feel* like a balloon.
And the FDA? Please. They approved lithium. Lithium. People die from lithium toxicity every year.
It’s not about the drug. It’s about how we treat people who need it.
We don’t give them tools. We give them guilt.
Andrew Frazier
Look, I get it. You wanna play doctor. But most of these people are just lazy. They eat McDonald’s, sit on the couch, smoke, and then wonder why they got diabetes.
It’s not olanzapine’s fault. It’s their fault. And now you wanna give them metformin so they can keep being lazy?
Give them a kick in the ass. That’s what they need. Not more pills.
Also, why are we letting foreigners write medical guidelines? This is America.
Kumar Shubhranshu
Weight gain is real. But so is psychosis.
Choose.
One kills slowly. One kills fast.
Metformin helps. So does walking.
Do both.
Or don't.
But don't pretend the choice doesn't exist.
Mayur Panchamia
Let me be blunt-olanzapine is a chemical sledgehammer. It doesn’t just calm the mind-it obliterates it. And yeah, it turns people into walking doughnuts.
But here’s the thing: when your brother is screaming at ghosts and trying to jump out the window, you don’t care if he gains 40 pounds.
You care if he’s alive.
So yes, monitor. Yes, mitigate. But don’t you dare tell someone they can’t have this drug because it makes them ‘unattractive.’
Some battles are worth the belly.
Karen Mitchell
It is unconscionable that clinicians continue to prescribe olanzapine as a first-line agent without mandatory metabolic screening. This is not medical practice; it is negligence dressed in white coats.
Furthermore, the normalization of weight gain as an ‘acceptable trade-off’ reflects a profound moral failure within psychiatric care.
Patients are not expendable. Their bodies are not collateral damage.
Until we enforce accountability, this will continue.
Geraldine Trainer-Cooper
i just think about how we treat people like machines. you got side effects? here's another pill. you got diabetes? here's another pill. you got a stroke? well, we tried.
what if we just… listened? what if we asked them what they wanted?
not what the algorithm says.
what they actually feel.
maybe the real cure isn't in the pill.
maybe it's in the quiet.
Nava Jothy
OMG I’m crying 😭 this is so true. I’ve been on olanzapine for 5 years. I gained 70lbs. My mom cried when she saw me. My husband left. I’m on 4 meds now. But I don’t hear the voices anymore. So… I guess it’s worth it? 🤷♀️
But why can’t we have a drug that helps without turning us into monsters? 😔
Big Pharma doesn’t care. They just want our insurance info. 💔
Kenny Pakade
Why are we even talking about this? It’s obvious. Olanzapine is a tool. Use it right. Don’t blame the tool because you’re too lazy to use it properly.
And stop blaming America. India’s got the same problem. China’s got it. Every country.
It’s not a nationality issue. It’s a human issue.
Stop making it political.
Just fix it.
brenda olvera
in mexico, we say ‘el cuerpo habla’-the body speaks. but no one listens.
olanzapine doesn’t lie. it tells you: ‘i’m changing you.’
and if you listen? you can change with it.
walk. eat beans. drink water. sleep. talk to someone.
it’s not magic. it’s medicine.
and it’s free.
you just have to choose to hear it.
Myles White
Let’s take a step back and consider the broader context of antipsychotic pharmacology and its intersection with public health infrastructure. The data presented, while compelling, is inherently limited by selection bias in clinical trials, inconsistent monitoring protocols across institutions, and the confounding influence of socioeconomic determinants of health-such as access to nutritious food, safe housing, and consistent psychiatric follow-up.
Furthermore, the framing of metabolic side effects as ‘risk factors’ for stroke may inadvertently pathologize normal physiological responses to pharmacological intervention, particularly when the alternative-uncontrolled psychosis-carries its own set of catastrophic outcomes, including increased mortality from suicide, accidents, and neglect.
What we’re really discussing is not merely drug safety, but the adequacy of our healthcare systems to support patients long-term. A patient on olanzapine in a rural clinic without access to a dietitian or gym is not failing-they’re being failed by the system.
Therefore, the solution is not to vilify olanzapine, but to invest in holistic, community-based care models that integrate metabolic monitoring, nutritional support, and psychosocial rehabilitation as standard components of treatment-not as afterthoughts.
And yes, metformin should be considered prophylactically, but only if it’s paired with actual human support. Because pills don’t change lives. People do.
Max Manoles
That’s exactly it. The system’s broken. We’re treating symptoms, not people.
I had a patient last month who lost her job because she couldn’t get to the clinic for labs. She stopped her meds. Then she had a stroke.
We didn’t fail her because of olanzapine.
We failed her because we didn’t show up.
Write a comment