Post-Surgery Eye Inflammation Symptom Checker
Check Your Symptoms
Select any symptoms you're experiencing after your eye surgery. This tool helps determine if you need urgent medical attention.
When you come out of eye surgery, the risk of postoperative eye inflammation can be unsettling. Knowing why it happens and what to look for helps you act fast and protect your vision.
Postoperative eye inflammation is an immune‑mediated reaction that occurs after intraocular or ocular surface procedures, leading to redness, pain, and visual changes. It typically involves the conjunctiva, cornea, or uveal tract and can range from mild irritation to sight‑threatening swelling.
What triggers the inflammation?
Several mechanisms can set off the inflammatory cascade after surgery. Understanding each trigger lets patients and clinicians target the right treatment.
- Surgical trauma - Even the most delicate incision disrupts tiny blood vessels and cells, releasing cytokines that attract white blood cells.
- Infection - Bacterial or viral contaminants can enter the eye during or after the procedure, prompting a classic inflammatory response.
- Inflammatory response - The body’s natural healing process involves prostaglandins and leukotrienes, which cause redness, swelling, and pain.
- Medication side‑effects - Some postoperative drops, especially steroids, can provoke a “steroid response” that mimics inflammation.
- Dry eye syndrome - Reduced tear film after surgery makes the ocular surface more irritable, amplifying any inflammatory signals.
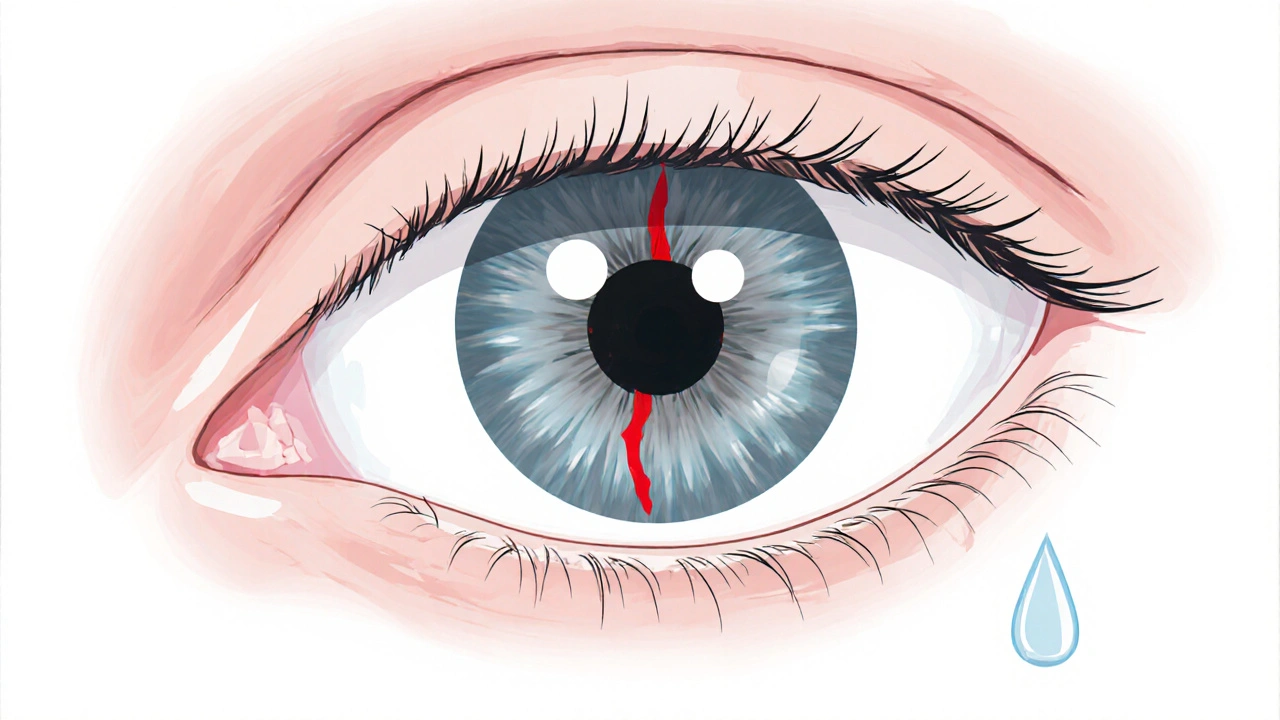
Typical symptoms and timeline
Symptoms usually appear within the first 24‑48 hours, but some can surface weeks later if complications develop. Common signs include:
- Redness that starts at the incision site and may spread across the white of the eye.
- Throbbing or aching pain, especially when moving the eye.
- Sensitivity to light (photophobia) that makes bright environments uncomfortable.
- Blurred or fluctuating vision, sometimes accompanied by floaters.
- Watery or mucous discharge that feels gritty.
If symptoms worsen after the first few days, or if you notice sudden vision loss, treat it as an emergency.
How doctors diagnose postoperative eye inflammation
Ophthalmologists combine patient history with a thorough eye exam. Key tools include:
- Slit‑lamp biomicroscopy - provides magnified view of the cornea, conjunctiva, and anterior chamber.
- Fluorescein staining - highlights epithelial defects and corneal abrasions.
- Intraocular pressure measurement - elevated pressure may signal a steroid response or secondary glaucoma.
- Optical coherence tomography (OCT) - detects subtle retinal swelling such as cystoid macular edema.
Based on findings, the clinician categorises the inflammation into specific sub‑types.

Common sub‑types after eye surgery
| Inflammation type | Typical cause | Main symptoms | First‑line treatment |
|---|---|---|---|
| Uveitis | Surgical trauma or immune reaction | Redness, pain, photophobia, floaters | Topical corticosteroid drops |
| Conjunctivitis | Surface irritation or infection | Diffuse redness, watery discharge | Antibiotic or antihistamine drops |
| Keratitis | Corneal epithelial damage | Pain, hazy vision, foreign‑body sensation | Lubricating drops + possible antibiotics |
| Cystoid macular edema | Inflammatory fluid accumulation in the macula | Gradual central vision blur | NSAID eye drops or peri‑ocular steroids |
Treatment options and what to expect
The goal is to curb inflammation while preserving the surgical outcome. Common therapies include:
- Topical steroids - Reduce cytokine activity; dosing is tapered over weeks.
- Non‑steroidal anti‑inflammatory drugs (NSAIDs) - Useful for mild cases or as steroid-sparing agents.
- Antibiotic eye drops - Prescribed when bacterial infection is suspected.
- Oral anti‑inflammatories - reserved for severe uveitis or when ocular drops alone are insufficient.
- Management of Intraocular pressure spikes - may require pressure‑lowering drops or temporary discontinuation of steroids.
Patients typically notice symptom relief within 48‑72 hours of starting medication. Regular follow‑up visits are essential to adjust dosages and monitor for side‑effects like cataract formation or steroid‑induced glaucoma.
Prevention tips for a smoother recovery
- Follow pre‑operative instructions precisely - include eye‑cleansing protocols and any pre‑surgery antibiotics.
- Choose an experienced surgeon - meticulous incision technique reduces tissue trauma.
- Adhere to the prescribed postoperative drop schedule - skipping doses can let inflammation flare.
- Protect your eyes from wind, dust, and bright sunlight using sunglasses and a shield.
- Stay hydrated and maintain a balanced diet rich in omega‑3 fatty acids; they support natural anti‑inflammatory pathways.
- Report any unusual symptoms promptly - early intervention prevents complications.
When to seek urgent care
If you notice any of the following, call your ophthalmologist or go to the emergency department right away:
- Sudden loss of vision or a large dark spot in the visual field.
- Severe, worsening pain despite medication.
- Rapidly increasing redness that spreads beyond the incision.
- Persistent fever or systemic signs of infection.
- Noticeable swelling of the eyelid that limits eye opening.
Quick checklist for the first week after surgery
- Apply all prescribed drops at the exact times.
- Log any new or worsening symptoms.
- Keep follow‑up appointments - usually at day 1, week 1, and month 1.
- Avoid rubbing the eye.
- Use protective eyewear when outdoors.
How long does postoperative eye inflammation usually last?
Mild inflammation often resolves within a week, while moderate cases may need 2-4 weeks of tapering drops. Persistent inflammation beyond six weeks should be re‑evaluated.
Can I use over‑the‑counter eye drops for postoperative inflammation?
Only if your ophthalmologist explicitly approves them. Some OTC drops contain preservatives that may aggravate inflammation.
Are steroids safe after eye surgery?
When used as prescribed, topical steroids are the most effective way to control inflammation. However, they must be monitored for side‑effects like raised intraocular pressure.
What lifestyle changes help reduce postoperative inflammation?
Stay hydrated, avoid smoking, wear sunglasses, and limit screen time for the first few days to give the eye a break.
Is it normal to have blurry vision after cataract surgery?
Mild blurriness is common as the eye heals and the cornea stabilises. If vision does not improve after a couple of weeks, contact your surgeon.



Comments
9 Comments
James Gray
Great rundown, super helpful for anyone post‑op!
Scott Ring
I totally agree-following the post‑surgery checklist can really cut down on complications. Keeping those drops on schedule and protecting the eye from wind are simple steps that make a big difference.
Shubhi Sahni
Post‑operative eye inflammation is a complex cascade that begins the moment the incision is made, and cytokines released from damaged cells immediately call white blood cells to the site, which in turn produce prostaglandins and leukotrienes that cause the classic redness and pain, while the breach in the corneal epithelium can also let microbes slip in, prompting an infection‑driven response, and even the preservatives in some postoperative drops may act as irritants, especially in eyes already compromised by dry‑eye syndrome, leading to a feedback loop of further tearing and discomfort, patients typically notice the first signs within 24 to 48 hours, but delayed reactions can surface weeks later as cystoid macular edema, which is why a thorough slit‑lamp examination is indispensable, fluorescent staining reveals micro‑abrasions that are otherwise invisible, and optical coherence tomography can catch subtle retinal swelling before vision is noticeably affected, management usually starts with topical corticosteroids, tapered slowly to avoid rebound inflammation, and non‑steroidal anti‑inflammatory drops are added for steroid‑sparing benefits, finally, regular follow‑up appointments allow the surgeon to adjust therapy and watch for pressure spikes that could indicate a steroid response.
Danielle St. Marie
Honestly, if you’re not already on a brand‑name steroid regimen, you’re doing it wrong 🙄. Only the best ophthalmic protocols will keep your vision pristine. 💎
keerthi yeligay
Pls check dosage, some drops can cause pressure rise.
Peter Richmond
Indeed, monitoring intra‑ocular pressure is essential when tapering steroids; schedule a follow‑up within the first week.
Bonnie Lin
Good point. Keep a log of drop times and any discomfort.
sara fanisha
Will do, thanks for the tip!
Tristram Torres
Remember to avoid rubbing the eye; it can worsen inflammation.
Write a comment