Steroid Insulin Adjustment Calculator
Enter Your Current Information
Key Guidelines
- 20mg+ prednisone 30-50% increase
- 100mg+ prednisone Double dose
- Mealtime insulin 50-100% increase
- Tapering rule 10-20% reduction per 10mg steroid drop
Recommended Insulin Adjustment
Enter your current steroid dose and insulin regimen to see adjustments.
Important Tapering Guidance
Reduce insulin by 10-20% for every 10mg reduction in prednisone equivalent. Monitor closely for hypoglycemia.
Example: If reducing from 40mg to 20mg prednisone, reduce total insulin by 20-30%.
When you're on steroids-whether for asthma, arthritis, or after a transplant-your blood sugar can spike unexpectedly. Even if you've never had diabetes before, high-dose steroids can push your glucose levels into dangerous territory. This isn't just a side effect. It's a real, well-documented condition called steroid hyperglycemia. And if you're already living with diabetes, it can turn your usual routine upside down.
Why Steroids Raise Blood Sugar
Steroids like prednisone, hydrocortisone, and dexamethasone don’t just calm inflammation. They mess with how your body handles sugar. They block insulin from doing its job, make your liver pump out more glucose, and even reduce the amount of insulin your pancreas can produce. The result? Blood sugar climbs, especially after meals.This isn’t a slow, gradual rise. It’s often sharp and timed to when the steroid hits its peak. If you take prednisone in the morning, your blood sugar will likely spike between 4 and 8 hours later-that’s breakfast and lunch, not dinner. That’s why checking your glucose only in the morning misses half the problem. Fasting numbers can look fine while your post-meal numbers are soaring.
Who’s at Risk?
Not everyone on steroids gets high blood sugar, but some people are far more likely to. If you already have type 2 diabetes, your risk jumps significantly. But even people without diabetes aren’t safe. Studies show that over 50% of hospitalized patients on high-dose steroids develop hyperglycemia. For those on doses over 100 mg of prednisone equivalent per day, the odds of needing insulin go up more than tenfold.Other red flags:
- Age 65 or older
- BMI over 30
- History of prediabetes or high fasting glucose
- Family history of diabetes
- Taking other immunosuppressants like tacrolimus (common after transplants)
- Low magnesium levels
- Chronic hepatitis C
If you check any of these boxes, your doctor should be monitoring your glucose from day one-not waiting for symptoms to show up.
How Much Insulin Do You Need?
If you're on insulin, you’re probably going to need more. A typical increase is 30-50% when starting moderate steroid doses (20 mg prednisone or higher). For someone on high doses-say, 100 mg prednisone daily-it’s not unusual to need double your usual insulin.But here’s the catch: you don’t just need more insulin. You need it at the right times. Steroids hit hardest after breakfast and lunch, so that’s when your mealtime insulin should be highest. Your long-acting insulin might only need a 10-20% bump, but your rapid-acting insulin (like lispro or aspart) could need a 50-100% increase.
For example:
- Before: 10 units of rapid-acting insulin at breakfast
- On steroids: 15-20 units at breakfast
- Before: 8 units at lunch
- On steroids: 12-16 units at lunch
Many people find their dinner insulin doesn’t need to change at all-because the steroid’s effect has worn off by then. That’s why blanket increases across the board can lead to nighttime lows later on.
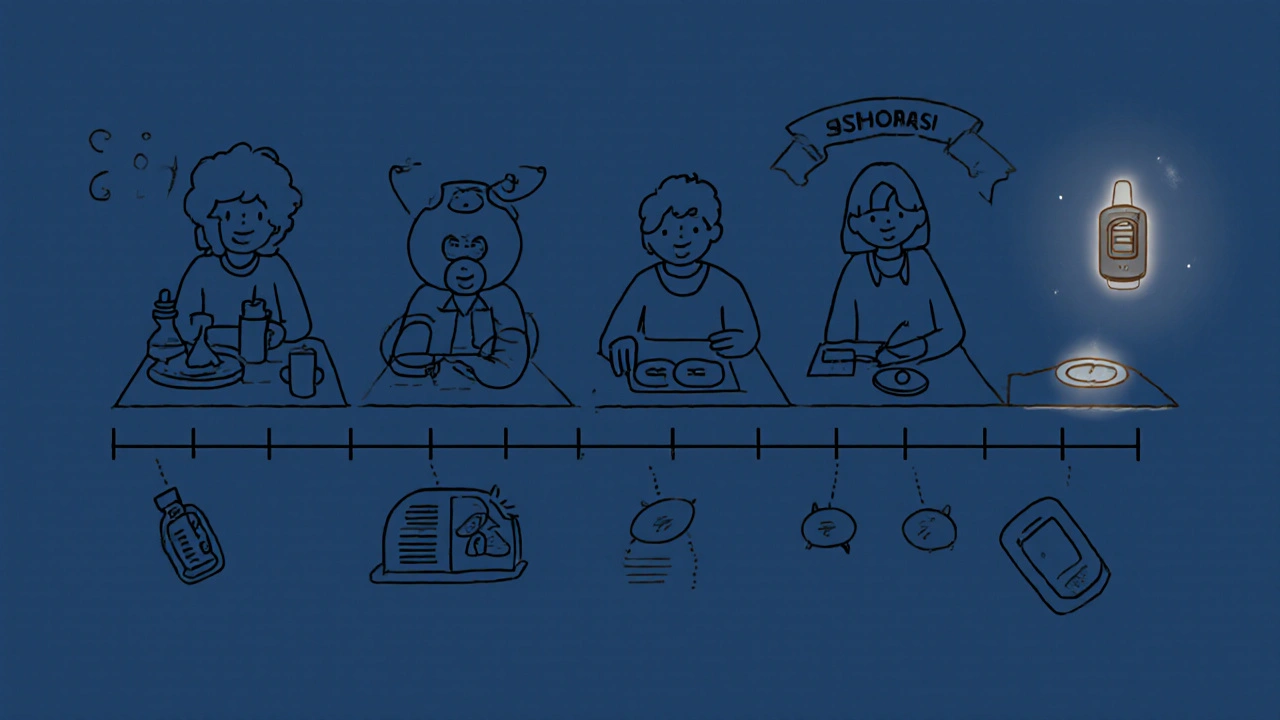
Monitoring Is Everything
Checking your blood sugar once a day is useless here. You need to check it before and two hours after every meal. That’s at least four times a day. If your glucose is over 180 mg/dL after meals, you’re not managing this well enough.Continuous glucose monitors (CGMs) are game-changers. A 2021 study showed CGM users adjusted their insulin doses 37% more accurately than those using fingersticks. Why? Because you see the spikes as they happen. You don’t wait for a number to be high before acting-you see the trend and adjust in real time.
And don’t skip checking at bedtime. Even if your daytime numbers are under control, nighttime lows can sneak up when your steroid dose starts to drop.
The Tapering Trap
This is where most people get hurt. When the steroid dose goes down, your insulin needs don’t automatically follow. If you keep your high doses, you’re setting yourself up for dangerous lows.Studies show that 18% of hospital readmissions within 30 days of stopping steroids are due to hypoglycemia-because insulin wasn’t reduced. In one study, 22% of patients who didn’t adjust their insulin during tapering had at least one severe low blood sugar episode.
Here’s the rule: reduce your insulin by 10-20% for every 10 mg reduction in prednisone equivalent. So if you were on 60 mg prednisone and drop to 50 mg, cut your total daily insulin by 10-20%. If you drop from 40 mg to 20 mg, cut insulin by 20-30%.
Don’t guess. Track your steroid dose and insulin dose side by side. Write it down. Use a notes app. Share it with your care team.
What About Oral Diabetes Medications?
Most oral meds aren’t enough. Metformin might help a little, but it won’t cut it when steroids are running high. Sulfonylureas? They can cause dangerous lows, especially when the steroid tapers. DPP-4 inhibitors and SGLT2 inhibitors? They’re often ineffective in this setting.Insulin is the gold standard for steroid hyperglycemia. That’s what endocrinologists use in hospitals. It’s flexible, fast-acting, and you can adjust it daily based on your glucose readings. If you’re not on insulin yet and your glucose is consistently above 180 mg/dL after meals, insulin is likely your best-and safest-option.
What’s New in Management?
Hospitals are starting to use smart systems that automatically adjust insulin based on steroid dose, weight, and glucose trends. Tools like the EndoTool System and Glytec’s eGlucose Management System have cut hyperglycemia rates by 27% and hypoglycemia by 33% in trials.Even more promising? Machine learning. A 2023 trial showed an algorithm using steroid dose, BMI, and baseline HbA1c could predict insulin needs with 85% accuracy. That’s not science fiction-it’s already being tested in clinics.
By 2027, most U.S. hospitals will have formal protocols for steroid hyperglycemia. But if you’re managing this at home, you’re still on your own. That’s why knowing the numbers, timing, and patterns matters more than ever.
What You Can Do Right Now
If you’re starting steroids:- Ask your doctor for a baseline HbA1c and fasting glucose before you begin.
- Start checking your glucose before and after meals-four times a day minimum.
- If you’re on insulin, expect to increase your mealtime doses by 50-100%.
- Use a CGM if you can. It’s worth the cost.
- Track your steroid dose and insulin dose together in a log.
- When tapering, reduce insulin by 10-20% for every 10 mg drop in prednisone.
- Don’t wait for symptoms. A glucose of 200 mg/dL after lunch isn’t normal-it’s a signal.
Steroid hyperglycemia isn’t your fault. It’s a biological response to powerful drugs. But with the right monitoring and adjustments, you can avoid complications and stay in control. You don’t have to choose between treating your illness and managing your blood sugar. You can do both-just not the same way you did before.
Can steroids cause diabetes in people who never had it before?
Yes. Steroid-induced diabetes (SIDM) is a well-documented condition. Up to 40% of patients on high-dose steroids develop high blood sugar, even if they’ve never been diagnosed with diabetes. It’s often temporary, but it can become permanent if not managed properly, especially in people with risk factors like obesity or prediabetes.
How long does steroid-induced high blood sugar last?
It usually lasts as long as the steroid is being taken and for a few days to weeks after stopping. Blood sugar tends to drop quickly once the steroid dose is reduced. But in some cases-especially with long-term use or in people with pre-existing insulin resistance-it can become permanent. That’s why monitoring and adjusting insulin during and after treatment is critical.
Should I stop my steroids if my blood sugar goes high?
No. Steroids are often essential for treating life-threatening conditions like autoimmune diseases, organ rejection, or severe inflammation. Stopping them can be dangerous. The goal isn’t to stop the steroid-it’s to adjust your diabetes treatment to match it. Work with your doctor to manage your blood sugar while continuing the steroid therapy.
Is metformin enough to control steroid-induced high blood sugar?
Usually not. Metformin helps with insulin resistance, but it doesn’t overcome the massive glucose surge caused by steroids. Studies show insulin is far more effective in this setting. Oral medications like sulfonylureas can cause dangerous lows during steroid tapering. Insulin remains the most reliable and safest option for managing steroid hyperglycemia.
Why does my blood sugar spike after lunch but not dinner when I take steroids in the morning?
Steroids like prednisone peak in your bloodstream 4-8 hours after you take them. If you take your dose at 8 a.m., the peak hits around noon to 4 p.m.-right when you’re digesting lunch. By dinner time, the steroid effect has worn off, so your blood sugar doesn’t rise as much. That’s why you need higher insulin at breakfast and lunch, not dinner.
Can I use a CGM to help adjust my insulin during steroid therapy?
Yes, and it’s highly recommended. CGMs show you real-time trends, not just snapshots. You’ll see exactly when your glucose rises after meals and how long it stays high. This lets you adjust insulin doses more precisely. One study found CGM users adjusted insulin 37% more accurately than those using fingersticks alone.
What should I do if I feel shaky or dizzy while on steroids and insulin?
Check your blood sugar immediately. If it’s below 70 mg/dL, treat it with 15 grams of fast-acting sugar (glucose tabs, juice, or candy). Then recheck in 15 minutes. If you’re having frequent lows, especially during steroid tapering, your insulin dose is likely too high. Contact your doctor to reduce your insulin. Never ignore hypoglycemia-it can be dangerous.
Do I need to see an endocrinologist if I’m on steroids and have diabetes?
It’s strongly advised, especially if you’re on high doses or have trouble controlling your glucose. Endocrinologists specialize in these complex cases. They know how to adjust insulin based on steroid type, dose, and timing. Many hospitals now have steroid-specific protocols run by endocrine teams. If your doctor isn’t familiar with these guidelines, ask for a referral.




Comments
8 Comments
Rachel Harrison
Just started prednisone for my rheumatoid flare and my BG spiked to 280 after lunch 😱 I had no idea steroids did this. This post saved my life. Started checking before/after meals and bumped my lispro by 75%-now I’m under 180. CGM is worth every penny. 💪
Tiffanie Doyle
OMG YES SAME 😭 I thought I was just eating too much carbs but nooo it was the steroids. I’m on 40mg prednisone and my insulin needs doubled. I literally cried when I saw the pattern-breakfast and lunch only. Dinner? Barely changed. Also, don’t skip bedtime checks, I had a scary low at 3am when they tapered me too fast. 🙏
james landon
So basically if you’re on steroids you gotta be a full-time diabetic now? Cool. I’ll just stop the steroids then. 😅
Jenn Clark
Thank you for sharing this. I’m a nurse and see this all the time in the hospital-patients unaware, insulin not adjusted, and then readmissions. The tapering trap is real. I always tell my patients: write it down. Track dose and insulin side by side. Even a simple notes app helps. Small steps, big difference.
L Walker
My father was on 100mg prednisone post-transplant-he went from metformin to 80 units of insulin daily. The hospital used a protocol, but at home? We were flying blind. We ended up in A&E twice because we didn’t reduce insulin fast enough during taper. This article nails it. CGM was the only thing that kept him alive. If you’re on steroids and diabetic-get one. Now.
giri pranata
Bro this is gold. I’m from India and we don’t talk about this stuff enough. My cousin got steroids for lupus and ended up in ICU because they didn’t adjust insulin. He’s fine now but it was scary. I shared this with my whole family. Even my uncle who’s diabetic and on steroids now-he’s checking his sugar four times a day. Thank you for writing this. 🙏
Stuart Rolland
I’ve been managing steroid-induced hyperglycemia for over a year now after my kidney transplant. It’s not just about insulin dosing-it’s about timing, stress, sleep, even weather. I use a CGM and log everything in a spreadsheet-steroid dose, meal content, activity level, sleep hours, even my mood. The algorithm I built from this data? It’s 80% accurate at predicting my next spike. I’m not a tech guy, but this stuff works. The future is here, and it’s not magic-it’s data. If you’re doing this alone, you’re doing it wrong. Find your team. Track. Adjust. Repeat. You’re not alone in this.
Kent Anhari
Just want to add: if you’re on tacrolimus too, double down on monitoring. That combo is brutal. My numbers went haywire even more than with steroids alone. Endocrinologist saved me-she adjusted my basal insulin based on steroid peaks and tacrolimus trough levels. It’s complicated, but doable. Don’t be afraid to ask for help.
Write a comment