VTE and Birth Control: Quick Facts You Shouldn't Miss
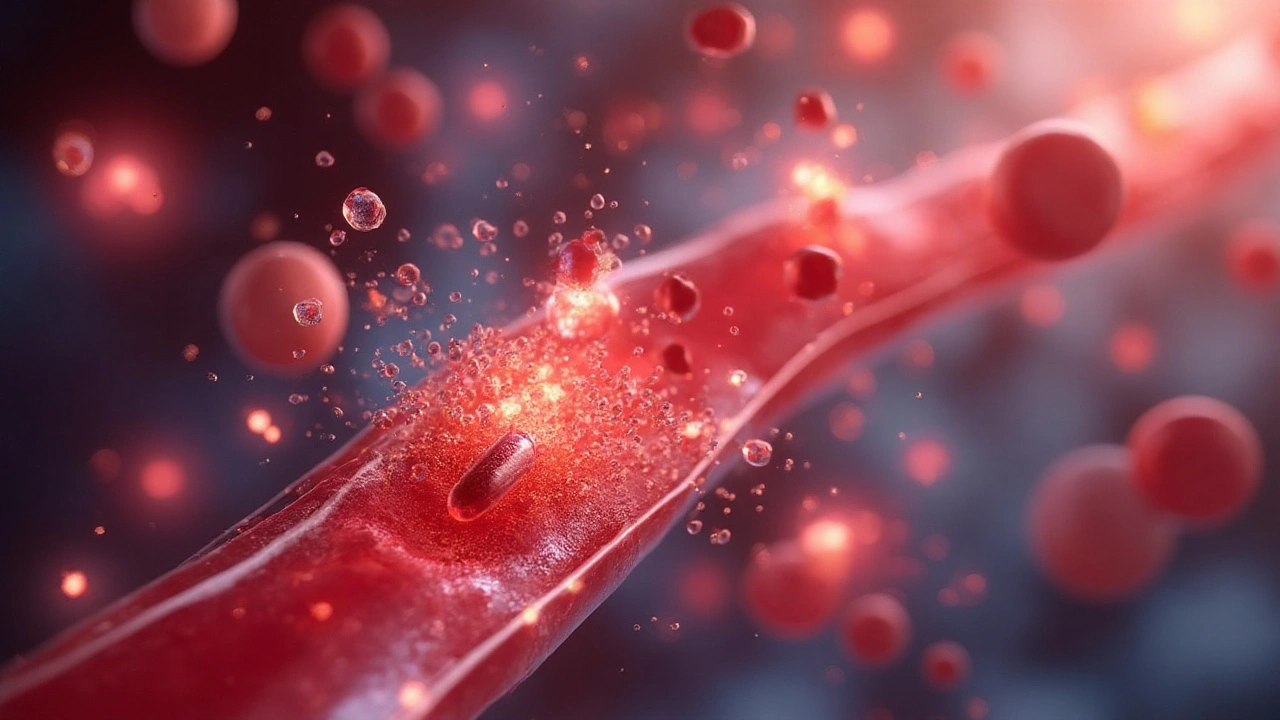
If you’re on the pill or another hormonal method, you’ve probably heard "blood clots" mentioned in the fine print. It’s not a myth – combined oral contraceptives (COCs) can raise the chance of venous thromboembolism (VTE). The key is knowing who’s at higher risk, what signs to look for, and how to protect yourself without giving up reliable birth control.
Why Birth Control Can Raise VTE Risk
COCs contain estrogen and progestin. Estrogen makes the blood a bit stickier, which helps prevent bleeding during a period but also nudges clot‑forming proteins up. Most women see a small increase – about a two‑to‑four‑fold rise compared to not using hormones. For a healthy 25‑year‑old, that still means a very low absolute risk, but the numbers jump for smokers, people over 35, or those with a family history of clots.
Progestin type matters, too. Newer generations (like drospirenone) have been linked to slightly higher clot rates than older forms (like levonorgestrel). If you’re worried, ask your doctor about a pill with a lower‑risk progestin or consider a non‑estrogen method.
How to Lower Your Clot Risk While Using Hormonal Contraceptives
First, be honest with your doctor about any past VTE events, clot‑related surgeries, or known genetic factors (such as Factor V Leiden). Even a mild thrombophilia can turn a modest pill‑related risk into something serious.
Second, ditch smoking. A smoker on COCs faces a dramatically higher chance of clotting. If you can’t quit cold turkey, look into nicotine patches or gum first, then switch to a birth control method without estrogen, like a copper IUD or a progestin‑only pill.
Third, stay active. Long flights, car rides, or desk jobs can slow blood flow in the legs. Stretch your legs every hour, wear loose clothing, and keep hydrated. Simple leg‑raising exercises during TV time can make a difference.
If you notice any warning signs – sudden leg pain, swelling, warmth on one side, or unexpected shortness of breath – treat them as emergencies. Those symptoms could signal a deep‑vein thrombosis (DVT) or a pulmonary embolism (PE). Call 911 or head straight to the ER.
Lastly, consider alternatives if your risk profile is high. Progestin‑only options, hormonal IUDs, or even non‑hormonal barriers avoid estrogen entirely. They’re just as effective for preventing pregnancy while keeping clot risk low.
Bottom line: birth control doesn’t automatically mean you’ll get a clot, but certain factors raise the odds. By sharing your medical history, staying smoke‑free, moving regularly, and watching for symptoms, you can use hormonal contraception safely. Talk to your healthcare provider about the best fit for your lifestyle and health – a quick chat now can save you a lot of worry later.