Diabetes Medication Side Effect Risk Calculator
Your Health Profile
Your Side Effect Risk Assessment
Recommended medications:
-
Metformin (extended-release)
- Reduced GI issues (25-40% lower)
- Vitamin B12 monitoring recommended
-
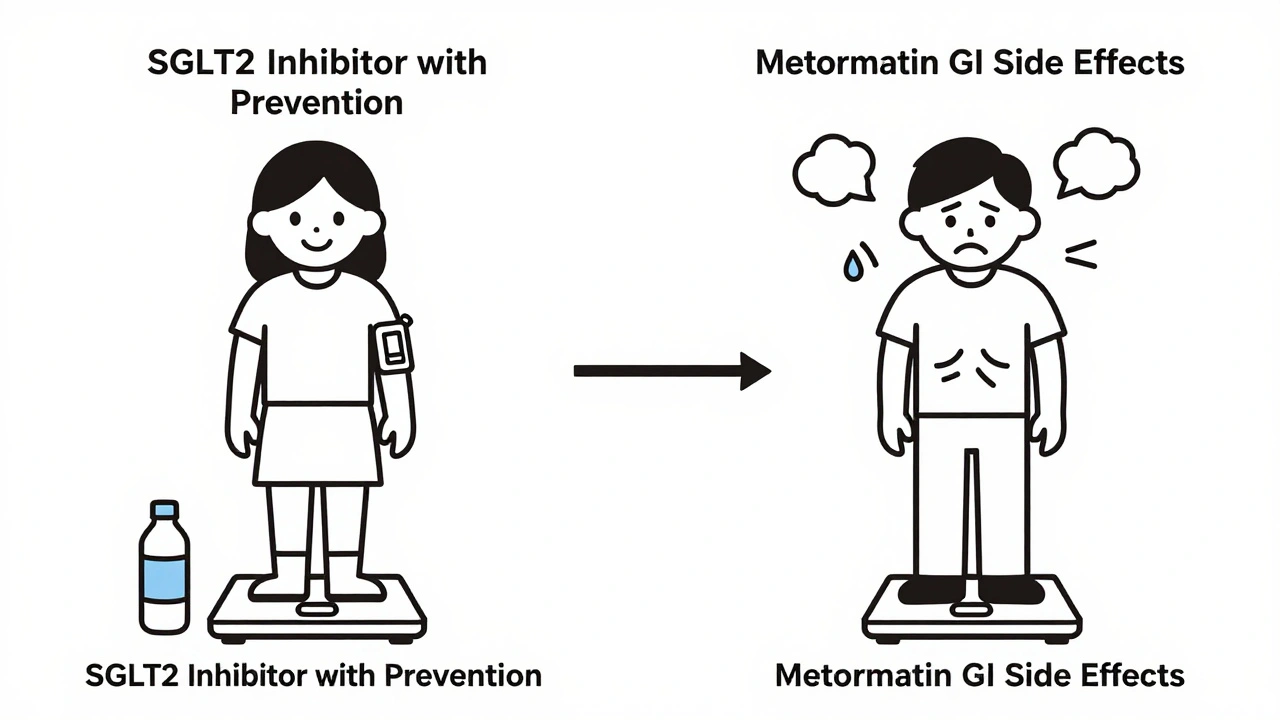
SGLT2 Inhibitors
- Weight loss benefit
- Watch for UTIs
Managing diabetes isn’t just about checking blood sugar levels and taking pills. For many people, the real challenge comes from the side effects of the very medications meant to help. These side effects don’t just cause discomfort-they can derail glucose control, reduce quality of life, and even lead to stopping treatment altogether. About half of people with Type 2 diabetes stop taking their meds within the first year, not because their blood sugar isn’t improving, but because the side effects feel worse than the disease.
Metformin: The First-Line Drug With Common Gut Issues
Metformin is the most prescribed diabetes medication in the world. It’s affordable, effective, and doesn’t cause low blood sugar. But for 20-30% of users, it brings stomach trouble: nausea, bloating, diarrhea, and loss of appetite. These symptoms aren’t mild-they can make people skip doses or quit entirely. The good news? Switching to the extended-release version (like Glucophage XR or Fortamet) cuts these side effects by up to 40%. Starting with a low dose-500 mg once a day with food-and slowly increasing it helps the body adjust. Most people find relief within a few weeks.
There’s another hidden risk with long-term metformin use: vitamin B12 deficiency. After four or more years on the drug, 5-10% of users develop low B12 levels. Symptoms like fatigue, dizziness, and tingling in hands and feet are often mistaken for aging or stress. But without treatment, this can lead to nerve damage. The fix? Get your B12 checked yearly if you’ve been on metformin for more than two years. Many doctors now recommend a daily 1,500 mcg supplement for long-term users.
Sulfonylureas: The Hidden Danger of Low Blood Sugar
Sulfonylureas like glipizide and glyburide work by forcing the pancreas to release more insulin. They’re cheap and effective at lowering blood sugar-but they come with a dangerous flip side: hypoglycemia. About 15-20% of users experience low blood sugar episodes, sometimes without warning. Symptoms include shaking, sweating, confusion, and rapid heartbeat. In older adults or those with kidney problems, these episodes can be life-threatening.
One patient on Reddit shared: “I passed out at work after taking my morning glipizide. My coworkers thought I was drunk.” That’s not rare. Continuous glucose monitors (CGMs) reduce severe hypoglycemia by 40%, but many patients still aren’t using them. The 15-15 rule helps in a pinch: eat 15 grams of fast-acting sugar (like juice or glucose tabs), wait 15 minutes, check again. But prevention is better than reaction. If you’re on sulfonylureas and keep having lows, talk to your doctor about switching to a safer option.
SGLT2 Inhibitors: Weight Loss With Serious Risks
Drugs like Jardiance, Farxiga, and Invokana work by making your kidneys flush out extra sugar through urine. The result? Weight loss (2-3 kg on average), lower blood pressure, and fewer heart-related hospitalizations. For people with heart disease or kidney issues, these drugs can be life-saving. But they also bring unexpected problems.
Genital yeast infections affect 4-6% of women and 1-2% of men. Urinary tract infections (UTIs) happen in 5-10% of users. One patient wrote: “I got a UTI every other month on Jardiance. I had to switch to Victoza.” Good hygiene and drinking plenty of water help, but some people need preventive cranberry supplements or low-dose antibiotics. More alarming are rare but deadly risks: Fournier’s gangrene (a rare flesh-eating infection near the genitals) and diabetic ketoacidosis-even when blood sugar isn’t high. The FDA added black-box warnings for these in 2018 after 55 cases were reported.
Another risk? Lower limb amputations. Canagliflozin (Invokana) showed a 0.3-0.5% higher risk compared to placebo in the CANVAS trial. That’s small, but real. If you have a history of foot ulcers or poor circulation, your doctor should think twice before prescribing this drug.
TZDs: Fluid Retention and Heart Risks
Thiazolidinediones like Actos and Avandia make cells more sensitive to insulin. They’re great for lowering blood sugar, but they cause fluid retention. That means swelling in the ankles, sudden weight gain, and worse-heart failure. Rosiglitazone (Avandia) was pulled from the market in Europe in 2011 after studies showed a 43% higher risk of heart failure. Even pioglitazone (Actos), which is still available, increases heart failure risk in people with NYHA Class III-IV heart failure. That’s why doctors avoid these drugs in patients with existing heart problems.
Weight gain is another issue. On average, users gain 2-5 kg in six months. For someone already struggling with obesity, that’s a dealbreaker. These drugs are rarely used today unless other options have failed-and even then, only with close monitoring.
Alpha-Glucosidase Inhibitors: Gas, Bloating, and Social Embarrassment
Acarbose (Precose) and miglitol (Glyset) slow down how fast your body breaks down carbs. That helps prevent blood sugar spikes after meals. But the trade-off? Undigested carbs hit your colon, where bacteria feast and produce gas. Up to 30% of users experience bloating, flatulence, and diarrhea. These aren’t just annoying-they can be socially isolating. One patient said: “I stopped going out to lunch with friends because I was too embarrassed.”
These drugs are rarely prescribed now. They’re not as effective as newer options, and the side effects are hard to tolerate. They’re mostly used in places where newer drugs are too expensive or unavailable.
Choosing the Right Drug: It’s Not One-Size-Fits-All
There’s no perfect diabetes drug. The best one is the one you can take consistently without dangerous or unbearable side effects. Metformin remains the go-to for most people because of its safety profile and heart benefits. But if you can’t tolerate the stomach issues, extended-release versions or combination pills like Xigduo XR (which pairs dapagliflozin with metformin) can cut GI side effects by 25%.
SGLT2 inhibitors shine for people with heart disease, kidney disease, or obesity. But if you’re prone to infections or have mobility issues, they might not be worth the risk. Sulfonylureas are fading out because of hypoglycemia danger-especially in older adults. TZDs? Almost always avoided unless there’s no other option.
What’s new? Genetic testing is starting to help. Some people carry a gene variant (ADL-1) that makes them 3.2 times more likely to get stomach problems from metformin. Others have a CYP2C9*3 variant that makes them super sensitive to sulfonylureas, increasing hypoglycemia risk by nearly threefold. In 2024, the American Diabetes Association will start recommending these tests for patients with repeated side effects.
What Patients Say: The Real Cost of Side Effects
On Drugs.com, metformin has a 6.3 out of 10 rating. Nearly half of reviewers say their side effects were moderate to severe. On Reddit’s r/diabetes community, SGLT2 inhibitors spark heated debates: “Jardiance dropped my A1c from 8.2 to 6.8-but I got three UTIs in six months. Worth it? Not for me.”
Mayo Clinic surveys show 68% of patients felt their doctors didn’t warn them about side effects before starting treatment. That’s a failure in communication. You shouldn’t have to learn about yeast infections or fainting spells from a forum post.
How to Manage Side Effects Before They Manage You
- Start low, go slow with metformin-500 mg daily with food, then increase every 2 weeks.
- Take B12 supplements if you’ve been on metformin for more than 2 years.
- Use a CGM if you’re on sulfonylureas or insulin-it catches lows before you feel them.
- Drink 2-3 liters of water daily if you’re on an SGLT2 inhibitor.
- Wear cotton underwear and avoid tight clothing to reduce yeast infection risk.
- Ask your doctor about fixed-dose combinations like Xigduo XR or Synjardy-they reduce pill burden and side effects.
Side effects aren’t a sign you’re doing something wrong. They’re a signal that your treatment needs tweaking. Don’t suffer in silence. Talk to your doctor. Ask: “What’s the most common side effect of this drug? How do I know if it’s serious? Is there a better option for me?”
What’s Next? The Future of Diabetes Meds
Researchers are working on next-gen drugs that avoid today’s pitfalls. New TZDs like INT131 show 60% less fluid retention in early trials. Glucose-responsive insulin-still in development-could replace daily shots and pills entirely by releasing insulin only when blood sugar rises. Closed-loop systems (artificial pancreases) are already helping some patients maintain near-perfect glucose control with fewer meds.
By 2030, the Diabetes Technology Society predicts traditional oral medications may be used less often. But for now, the drugs we have are still the main tool. The key isn’t finding the perfect pill-it’s finding the right one for your body, your life, and your risks.
Can diabetes medication side effects cause long-term damage?
Yes, some can. Long-term metformin use can lead to vitamin B12 deficiency, which may cause nerve damage if untreated. SGLT2 inhibitors carry rare but serious risks like Fournier’s gangrene and ketoacidosis, which can be life-threatening if not caught early. Sulfonylureas increase the risk of severe hypoglycemia, which can lead to falls, seizures, or brain injury in older adults. Regular monitoring and open communication with your doctor can prevent most of these outcomes.
Why do some people tolerate metformin better than others?
Genetics play a big role. People with the ADL-1 gene variant are over three times more likely to experience severe stomach side effects from metformin. Others may have slower digestion or a sensitive gut. Starting with a low dose, using extended-release forms, and taking the pill with food can help almost everyone adjust. If side effects persist after 3 months, switching to another class of drugs is often better than enduring discomfort.
Are newer diabetes drugs always better than older ones?
Not always. Newer drugs like SGLT2 inhibitors and GLP-1 agonists have proven benefits for heart and kidney health, but they’re also more expensive and carry unique risks. Metformin remains the safest, most studied option for most people without heart or kidney disease. The best choice depends on your health history, not just how new the drug is. A 70-year-old with no heart issues might do better on metformin than on a $600-a-month SGLT2 inhibitor.
Can I stop my diabetes medication if side effects are too bad?
Never stop on your own. Stopping suddenly can cause blood sugar to spike dangerously high, leading to complications like diabetic ketoacidosis or long-term organ damage. Instead, talk to your doctor. There’s almost always another option. You might switch from a sulfonylurea to a GLP-1 agonist, or from metformin to an SGLT2 inhibitor with better tolerability. Your doctor can adjust your plan safely.
How do I know if a side effect is normal or dangerous?
Mild nausea or increased urination early on is common. But if you feel dizzy, confused, have chest pain, swelling in your legs, or pain near your genitals with fever or redness, seek help immediately. These could signal ketoacidosis, heart failure, or necrotizing fasciitis. Keep a symptom journal and bring it to appointments. If a side effect lasts more than a week or gets worse, don’t wait-call your provider.


Comments
14 Comments
Deborah Andrich
Been on metformin for 6 years. B12 crash hit me hard-tingling fingers, brain fog, thought I was aging. Doctor never mentioned it. Started supplements, felt like a new person. Why isn’t this standard advice?
Rawlson King
People complain about side effects like they’re entitled to a perfect drug. Diabetes is a chronic disease. You take the medicine or you die early. Stop whining and manage it.
Alvin Montanez
Let me tell you something. I’ve been a diabetic for 23 years. I’ve seen every drug come and go. Metformin is the baseline. Everything else is just a fancy upgrade with more risks. People don’t realize that the side effects they’re complaining about? They’re the price of survival. You want to avoid hypoglycemia? Don’t take sulfonylureas. You want to avoid yeast infections? Drink water and wear cotton. It’s not rocket science. And yes, I’ve been on SGLT2 inhibitors. Got a UTI. Treated it. Didn’t quit. That’s called responsibility. You don’t get to cherry-pick your health outcomes. The disease doesn’t care how you feel. Your body is the battlefield, not a customer service hotline.
Tommy Watson
so i got on jardiance and like... 3 UTIs in 4 months?? like bro i was peeing blood and my boyfriend was like "are you sure it's not a yeast infection??" and i was like "I DON'T KNOW I'M JUST TRYING TO LIVE" and then i had to go to urgent care and they were like "oh yeah this is from the med" and i was like "WHY DID NO ONE TELL ME??" now i'm on metformin again and my stomach is screaming but at least i'm not crying in the bathroom again 🤮
Karen Mccullouch
Why is the FDA letting these pharma giants push these death pills? They know what they’re doing. They’re making billions while we’re getting infections and amputations. It’s not coincidence-it’s corporate greed. And don’t even get me started on how they silence patients who speak up. Wake up, people. This isn’t medicine. It’s a money scheme.
Cole Newman
metformin gave me diarrhea so bad i started carrying wipes in my purse like a toddler. switched to XR and it’s like night and day. also started taking b12 because my doc said "maybe" and i was like "maybe? i’m tired all the time and my tongue is burning" now i’m not a zombie. why do docs act like it’s a surprise?
Casey Mellish
As an Australian who’s been on metformin since 2018, I can confirm: the extended-release version is a game-changer. Also, B12 deficiency is grossly underdiagnosed. My GP didn’t mention it until I brought up the numbness in my toes. Now I take 1500 mcg daily. No more brain fog. Australia’s Medicare covers the test-why doesn’t the US? It’s not just about meds-it’s about systemic oversight.
Tyrone Marshall
There’s a deeper truth here that’s rarely discussed: diabetes medication isn’t just about biology-it’s about dignity. The shame of bloating in public, the fear of fainting at work, the isolation from yeast infections-these aren’t side effects. They’re social punishments. We treat diabetes like a math problem, but it’s a human experience. The best drug is the one that lets you live without hiding. That’s not just medical advice-it’s moral.
Emily Haworth
ALERT 🚨 THE GOVERNMENT IS HIDING THE TRUTH ABOUT SGLT2 INHIBITORS 🚨 I KNOW A GUY WHO KNEW A DOCTOR WHO SAID THEY’RE DESIGNED TO MAKE PEOPLE NEED MORE DRUGS LATER 😈 THEY’RE SELLING INFECTIONS SO WE’LL BUY ANTIBIOTICS AND THEN INSULIN AND THEN HOSPITALS 💉☠️ I SAW A VIDEO ON TIKTOK ABOUT A WOMAN WHO LOST HER FOOT AND THEY ERASED THE POST 🤫 #PharmaCoverup #DiabetesConspiracy
Tom Zerkoff
It is imperative to underscore that the pharmacological management of type 2 diabetes must be individualized with a rigorous assessment of risk-benefit profiles. The literature consistently demonstrates that metformin remains the first-line agent due to its established safety, efficacy, and cardiovascular benefits. However, the emergence of SGLT2 inhibitors and GLP-1 receptor agonists represents a paradigm shift in outcomes-based therapy. The challenge lies not in the medications themselves, but in the absence of standardized patient education protocols prior to initiation. Without informed consent regarding potential adverse effects, non-adherence becomes not a failure of discipline, but a failure of the system.
Yatendra S
you know what? maybe diabetes isn’t about pills at all. maybe it’s about karma. i took sugar for 20 years. now my body is like "you wanted sweetness? here’s your price." 🙏 maybe we need to stop blaming drugs and start blaming our choices. also, i heard if you chant "om" while eating, your blood sugar stays calm. just saying 🌿
Himmat Singh
The assertion that metformin is the gold standard is statistically misleading. Comparative effectiveness research from the UKPDS trial indicates that sulfonylureas demonstrate superior glycemic control in the first 12 months. The preference for metformin is rooted in cost-effectiveness models, not superior clinical outcomes. Furthermore, the claim regarding B12 deficiency as a widespread concern is overstated; the prevalence of clinically significant deficiency remains below 5% in longitudinal cohorts. The narrative of pharmaceutical malfeasance is emotionally compelling but empirically unsupported.
kevin moranga
Hey, I was right where you are. Metformin wrecked my gut. I thought I was done. Then I tried the XR version with food and slowly bumped up the dose. Took 3 months, but now I’m stable. And yeah, I take B12. No regrets. You’re not broken-you’re just on the wrong version. Keep going. You got this. And if you’re scared to talk to your doc? Write it down first. I did. Took me 17 drafts. But I sent it. And they listened. You can too.
Lara Tobin
i just wanted to say thank you for writing this. i’ve been silent for years because i felt guilty for hating my meds. but this? this made me feel seen. i cried. not because i’m weak, but because someone finally said it’s okay to not be okay with this. 💛
Write a comment