Why Thyroid Medication Matters in Pregnancy
When you’re pregnant, your body doesn’t just need more food or rest-it needs more thyroid hormone. That’s because your baby relies entirely on your thyroid hormones during the first 10 to 12 weeks of development, before its own thyroid even starts working. If your thyroid isn’t producing enough, or if your medication dose isn’t adjusted, your baby’s brain development could be affected. Studies show that untreated or poorly managed hypothyroidism during pregnancy can lower a child’s IQ by 7 to 10 points and increase the risk of miscarriage by up to 69%. The good news? With the right medication and monitoring, these risks drop dramatically. Levothyroxine, the standard treatment, is safe, well-studied, and classified as Pregnancy Category A by the FDA-meaning no proven risk to the fetus.
How Much More Medication Do You Need?
If you’re already taking levothyroxine before pregnancy, you’re likely going to need more. On average, women increase their dose by 20% to 30% as soon as they find out they’re pregnant. Some guidelines, like those from the American College of Obstetricians and Gynecologists (ACOG), suggest an immediate 50 mcg increase upon confirmation. Others, like the American Thyroid Association (ATA), recommend a 20-30% increase, which many patients achieve by taking two extra doses per week. For example, if you were taking 75 mcg daily before pregnancy, you’d move to about 90-95 mcg daily once pregnant.
But it’s not just about doubling up. If you’re newly diagnosed during pregnancy, dosing depends on your TSH level. If your TSH is above 10 mIU/L, start with 1.6 mcg per kilogram of body weight per day. If it’s between 5 and 10, start with 1.0 mcg/kg/day. A 2021 NIH study tracking 280 pregnant women found that their average levothyroxine dose jumped from 85.7 mcg before pregnancy to 100 mcg by the first trimester-that’s a 16.7% increase in just weeks.
When to Adjust Your Dose
Don’t wait for your first prenatal visit. Thyroid hormone demand spikes almost immediately after conception, often before you even know you’re pregnant. Experts agree: the best time to increase your dose is the day you get a positive pregnancy test. Delaying adjustment-even by a few weeks-can put your baby at risk. One patient on Reddit shared that her OB told her to "wait and see," and her TSH stayed at 4.2 at 8 weeks. She ended up needing another 25 mcg increase. That delay caused her months of anxiety. On the flip side, another woman increased her dose right away, kept her TSH in range, and her daughter scored in the 90th percentile for development at 18 months.
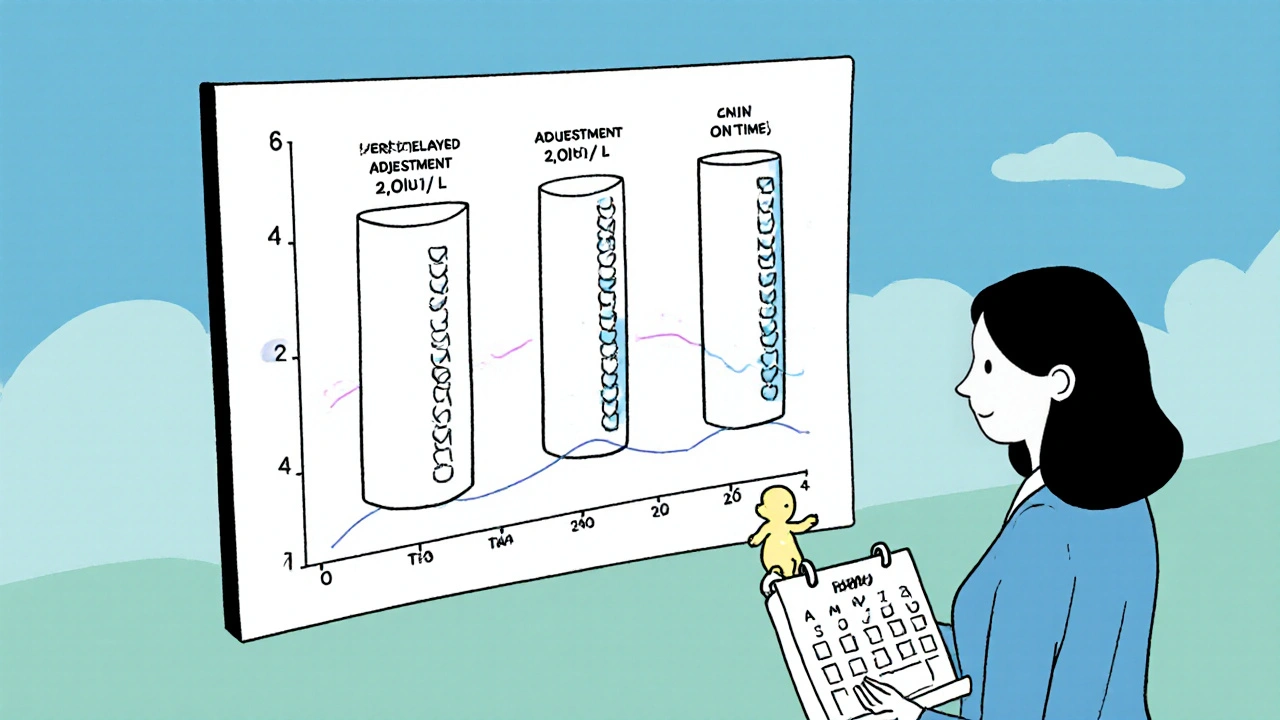
How Often Should You Get Tested?
Testing isn’t a one-time thing. You need to check your TSH every 4 weeks until your dose stabilizes, then at least once per trimester. The ATA recommends testing at 4-6 weeks, then every 4-6 weeks until 20 weeks, and again at 24-28 weeks and 32-34 weeks. Why so often? Because your body’s need for thyroid hormone keeps rising. By week 16, most women are already on their highest dose. A 2013 study found that 75% of women with pre-existing hypothyroidism needed a dose increase in the first trimester alone.
Target TSH levels vary slightly between guidelines. The ATA says keep TSH ≤ 2.5 mIU/L throughout pregnancy. The Endocrine Society says ≤ 2.5 in the first trimester, and up to 3.0 in the second and third. But here’s the key: if your TSH is above 2.5 in the first trimester, your risk of miscarriage goes up by nearly 70%. That’s why many endocrinologists aim for the stricter target, especially if you have thyroid antibodies.
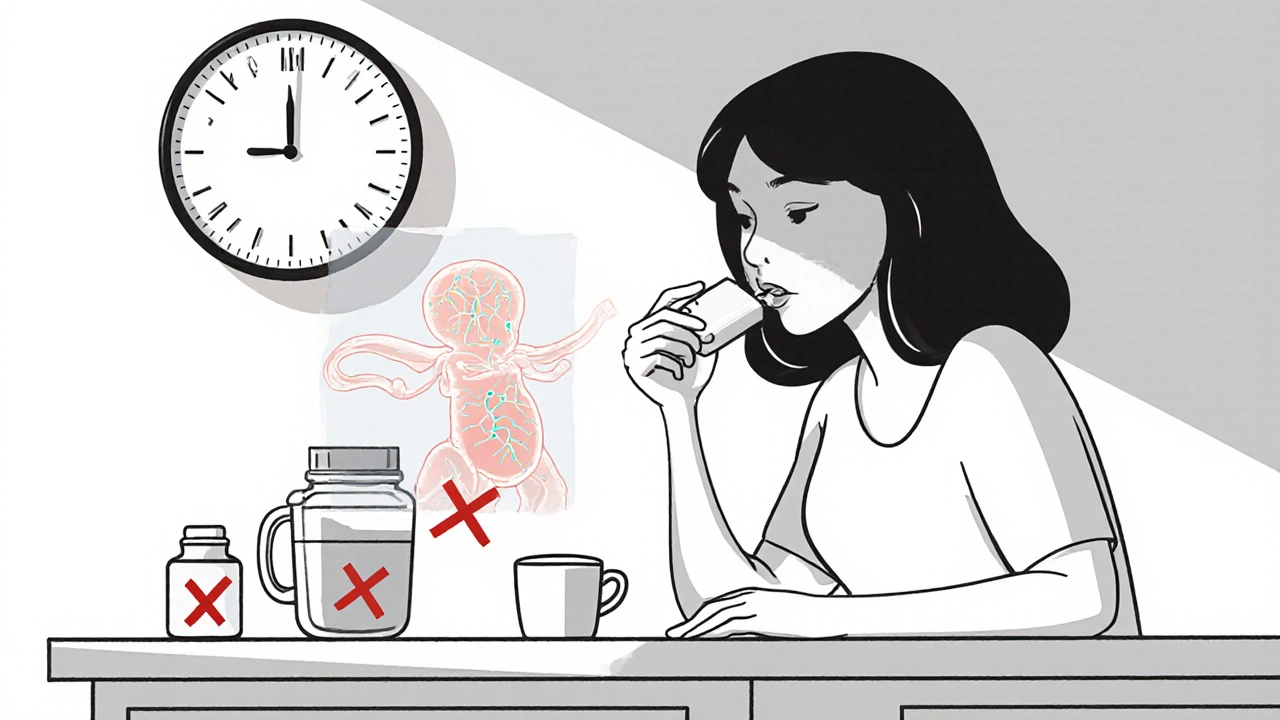
How to Take Your Medication Right
It’s not just about the dose-it’s about how you take it. Levothyroxine works best when taken on an empty stomach, at least 30 to 60 minutes before eating. If you take it with coffee, calcium, iron, or prenatal vitamins containing those minerals, your body absorbs 35% to 50% less. That means your TSH could creep up even if you’re taking the "right" dose.
Some patients try to make up for missed doses by taking extra pills on weekends. But that can backfire. Taking two extra doses on Saturday and Sunday might cause a spike in hormone levels Monday morning, then a drop by Tuesday. Instead, spread the extra doses across the week-add 3.5 mcg extra per day, every day, rather than 25 mcg on two days. This keeps your levels steady.
What Happens If You Don’t Adjust?
Ignoring dose changes isn’t just risky-it’s common. A survey of 150 OB/GYNs found that 68% don’t routinely check TSH at the first prenatal visit for women with known hypothyroidism. That’s a major gap. Without timely adjustments, you’re more likely to face preterm birth, low birth weight, or even preeclampsia. A 2021 study showed women whose doses were adjusted within four weeks of pregnancy confirmation had 23% fewer preterm births than those who waited.
And it’s not just about the baby. Untreated hypothyroidism can lead to fatigue, depression, muscle cramps, and high cholesterol in the mother. It can also interfere with labor and postpartum recovery. The stakes are high, but the solution is simple: test early, adjust early, and test again.
What’s New in 2025?
Thyroid care in pregnancy is getting smarter. In 2023, the ATA reversed its long-standing stance and now recommends universal TSH screening for all pregnant women in the first trimester-not just those with symptoms or risk factors. That’s a big shift. Meanwhile, AI tools are starting to predict your ideal dose based on your pre-pregnancy TSH, weight, and thyroid antibody status. The 2022 ENDO trial showed these tools improved TSH control by 28% compared to standard dosing.
There’s also growing global recognition. The WHO added levothyroxine to its Essential Medicines List for maternal health in 2023. But access remains unequal: in low-income countries, only 22% have consistent access to the medication, contributing to 15% of preventable developmental delays in those regions.
What You Can Do Today
- If you’re planning pregnancy or just found out you’re pregnant and take levothyroxine, contact your doctor immediately. Don’t wait.
- Ask for a TSH test right away-even if you feel fine.
- Take your medication on an empty stomach, 30-60 minutes before food.
- Avoid calcium, iron, and prenatal vitamins within 4 hours of taking your pill.
- Track your doses and test dates using a free app like MyThyroid, used by over 12,500 pregnant women.
- Insist on follow-up tests every 4 weeks until your dose is stable.
Thyroid health in pregnancy isn’t optional. It’s essential. With the right care, you can protect your baby’s brain development and have a healthy pregnancy. You don’t need to guess. You don’t need to wait. You just need to act-and make sure your care team does too.
Can I keep taking levothyroxine while pregnant?
Yes, absolutely. Levothyroxine is safe during pregnancy and is the standard treatment for hypothyroidism. It’s classified as Pregnancy Category A by the FDA, meaning no proven risk to the fetus. In fact, stopping your medication can be dangerous for your baby’s brain development. Most women need a higher dose during pregnancy, but the medication itself remains safe.
What happens if I miss a dose?
If you miss one dose, take it as soon as you remember, unless it’s close to your next scheduled dose. Don’t double up. Missing one dose occasionally won’t cause harm, but consistently skipping doses or delaying dose increases can raise your TSH and put your baby at risk. If you’re having trouble remembering, use a pill organizer or set a daily phone reminder.
Do I need to take iodine supplements too?
Most prenatal vitamins contain 150 mcg of iodine, which is the recommended daily amount during pregnancy. You don’t need extra iodine unless your doctor recommends it. Too much iodine can actually worsen thyroid function in some cases, especially if you have autoimmune thyroid disease. Stick to your prenatal vitamin and avoid iodine supplements unless advised.
Will my dose go back down after I have the baby?
Yes, most women return to their pre-pregnancy dose within a few weeks after delivery. Your body’s demand for thyroid hormone drops sharply after birth. Your doctor will likely check your TSH 6 to 8 weeks postpartum and adjust your dose accordingly. Don’t assume your pregnancy dose is your new normal-overdosing can cause symptoms like anxiety, weight loss, and heart palpitations.
What if I’m breastfeeding?
Levothyroxine is safe while breastfeeding. Only tiny amounts pass into breast milk, and studies show no effect on the baby’s thyroid function or development. You can continue your postpartum dose without concern. In fact, maintaining stable thyroid levels helps with energy, mood, and milk production.
Can I switch brands of levothyroxine during pregnancy?
It’s best to stick with the same brand throughout pregnancy. While generic levothyroxine is bioequivalent, small differences in absorption between brands can cause TSH fluctuations. If you must switch, your doctor should recheck your TSH 6 to 8 weeks after the switch to make sure your dose still works. Consistency matters more than cost during pregnancy.
How do I know if my dose is too high or too low?
Symptoms alone aren’t reliable. Feeling tired doesn’t always mean your dose is too low-pregnancy itself causes fatigue. The only way to know is through blood tests. TSH is the best marker. If your TSH is above the trimester target, your dose is likely too low. If it’s below 0.1 mIU/L, you may be overdosed. Always rely on lab results, not how you feel.
Is it safe to get pregnant if I have thyroid disease?
Yes, absolutely. With proper management, women with hypothyroidism have healthy pregnancies and babies at the same rate as those without thyroid disease. The key is getting your TSH in range before conception and continuing close monitoring. Many women with thyroid conditions go on to have multiple healthy pregnancies. Don’t let fear stop you-work with your endocrinologist and OB/GYN to plan ahead.




Comments
13 Comments
Ross Ruprecht
lol why is this even a thing? my cousin took levothyroxine while pregnant and her kid is now a pro gamer. no big deal.
Ragini Sharma
so if i take my pill with coffee and then eat idli for breakfast... is my baby gonna be dumber? 😅 i mean i already drink chai at 7am and its basically liquid caffeine with milk and sugar... help.
Bryson Carroll
this article is so basic its painful. anyone who needs a 30% dose increase probably shouldn't have gotten pregnant in the first place. you're not a lab rat. stop treating your body like a spreadsheet. also who even uses TSH anymore? real doctors measure free T3 and reverse T3
Lisa Lee
why are we letting the WHO dictate maternal health? in Canada we don't need some international panel telling us to screen everyone. we have standards. real ones. not this woke thyroid nonsense.
Manjistha Roy
If you are pregnant, or planning to be, and you are on levothyroxine, please do not wait. Do not hope. Do not assume you feel fine so it must be fine. Your baby’s brain is developing every single day, and thyroid hormone is the building block. Please, get tested. Please, adjust. Please, be the advocate for your own body. This is not optional. It is non-negotiable. And if your provider doesn’t get it, find someone who does.
Javier Rain
I was diagnosed with hypothyroidism at 6 weeks and my doc said "just wait till your next appointment." I didn't. I called the endo myself, got tested the next day, and doubled my dose. My daughter is 2 now and reads books at 18 months. This isn't magic. It's science. Do the work.
Laurie Sala
I took my pill with my prenatal vitamin because I was tired of remembering... and then my TSH went to 8.2... I cried for three days... I felt like a bad mom... I didn't know it was that serious... please... just... don't make my mistake...
Lisa Detanna
I'm from India and we don't always have access to levothyroxine. My sister had to travel 200km every month to get her pills. Her TSH was 12 at 10 weeks. She didn't know. No one told her. Her son is now 5 and has speech delays. This isn't just a US problem. This is a global human rights issue.
Demi-Louise Brown
Consistency in dosing and timing is critical. Deviations in absorption can lead to suboptimal fetal neurodevelopment. Monitoring TSH every four weeks during the first half of pregnancy is the standard of care. Failure to adhere to this protocol increases perinatal risk. Please consult your provider.
Matthew Mahar
so like... what if you dont know you're preggo for 8 weeks and you been taking your pill with coffee and calcium since day one... is it too late? like... do we just give up? or is there still hope??
John Mackaill
I've been managing Hashimoto's for 12 years. I had two kids. Both were born healthy. I adjusted my dose on day one of a positive test. I tested weekly. I didn't trust my OB. I trusted my endo. And I didn't let anyone tell me it was "just a little high." Thyroid isn't a suggestion. It's a lifeline.
Adrian Rios
I think people need to understand that this isn't just about numbers on a lab report. It's about the silent, invisible work your body does to build a human being. Your thyroid isn't just a gland-it's a conductor. And if the conductor is off, the whole orchestra collapses. The fact that we still have doctors telling patients to "wait and see" is a failure of medical education. We know better. We have to do better. Every day matters. Every microgram matters. Every woman deserves a care team that takes this seriously.
Casper van Hoof
The epistemological framework underpinning thyroid management in pregnancy reveals a paradox: while the biological imperative is quantifiable, the social infrastructure remains fragmented. The reduction of maternal neurodevelopmental risk to a TSH threshold reflects a technocratic bias that obscures the lived experience of care inequity. One may ask: is the algorithm truly serving the patient-or merely optimizing institutional compliance?
Write a comment