Most people with asthma or COPD rely on inhalers to breathe easier. But here’s the hard truth: if you’re not using your inhaler correctly, you’re getting less than half the medicine you’re paying for. Studies show 70 to 90% of patients mess up their technique. That means your inhaler isn’t working like it should-no matter how expensive or advanced it is.
Why Technique Matters More Than the Device
You might think the brand or type of inhaler makes the biggest difference. It doesn’t. What matters most is how you use it. A 2023 review by the Agency for Healthcare Research and Quality found that proper technique can improve lung delivery by 30-40% compared to poor technique-even if you’re using the same inhaler. Two people with the same prescription, same diagnosis, same inhaler: one gets 60% of the medicine into their lungs, the other gets 15%. The difference? Technique.
The World Health Organization estimates 262 million people have asthma and 210 million have COPD. That’s nearly half a billion people worldwide. If even half of them are using their inhalers wrong, we’re talking about millions of unnecessary flare-ups, hospital visits, and lost days of work or life. The solution isn’t a new device. It’s learning how to use the one you already have.
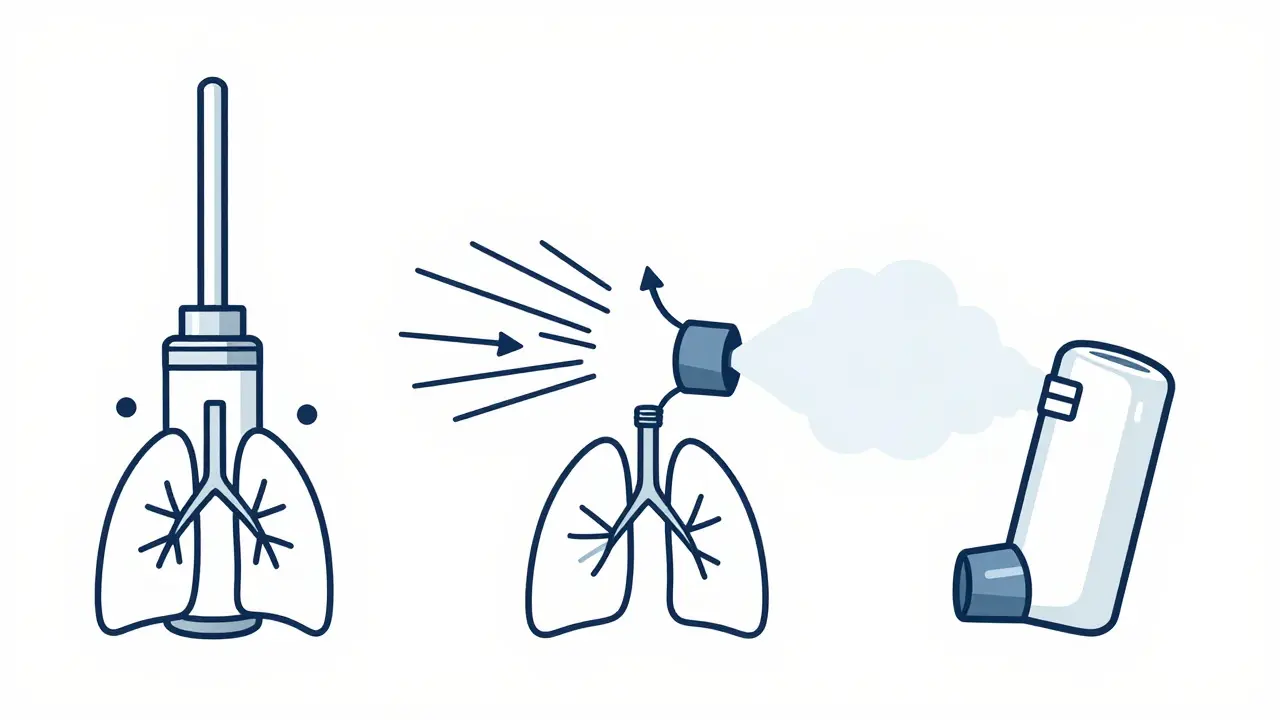
The Three Main Types of Inhalers (and How They Work)
There are three main kinds of inhalers, and each works differently. Using the wrong method for your device means the medicine won’t reach your lungs.
- Metered-Dose Inhalers (MDIs) - These are the classic aerosol cans you shake and spray. Examples include ProAir HFA and Ventolin HFA. They use a propellant to push out a puff of medicine. But here’s the catch: you have to press the canister and breathe in at the exact same time. If you’re too early or too late, most of the medicine hits your throat instead of your lungs.
- Dry Powder Inhalers (DPIs) - These include Diskus, Ellipta, and Turbuhaler. No propellant. No button to press. You just breathe in hard and fast. The force of your breath pulls the powder into your lungs. But if you’re too weak, too slow, or breathe out into the device first, the powder won’t aerosolize. That’s why many older adults or people with severe COPD struggle with these.
- Soft Mist Inhalers - The Respimat is the main one. It releases a slow, gentle mist over 1.5 seconds. You don’t need to time your breath perfectly. But you still need to inhale deeply and hold your breath. It’s easier for people who can’t coordinate MDIs or can’t generate enough force for DPIs.
Here’s the thing: no single device is best for everyone. Your doctor should match the inhaler to your ability-not just your diagnosis. A 65-year-old with weak lungs might do better with a soft mist inhaler than a DPI. A teenager who can breathe hard and fast might do great with a DPI. But if you’re using the wrong technique for your device, you’re wasting medicine.
How to Use an MDI the Right Way (Step by Step)
If you’re using a metered-dose inhaler, here’s the correct method, based on the NHLBI and American Lung Association guidelines:
- Remove the cap and shake the inhaler well for 5 seconds.
- Breathe out fully-away from the inhaler. Don’t blow into it.
- Place the mouthpiece between your lips and seal your lips around it.
- Start breathing in slowly through your mouth, and at the same time, press down on the canister.
- Keep breathing in slowly for 3 to 5 seconds until your lungs feel full.
- Hold your breath for 10 seconds. This lets the medicine settle into your airways.
- Breathe out slowly through your nose.
And here’s the most overlooked part: wait 60 seconds between puffs. If you take two puffs back-to-back, the second puff won’t reach your lungs properly. The first puff leaves a cloud of medicine in your mouth and throat. Waiting lets that clear out so the next puff can go deep.
How to Use a Dry Powder Inhaler (DPI) the Right Way
DPIs don’t need shaking or timing. But they need power. Here’s how to get it right:
- Load the dose as instructed (some need you to slide a lever, others twist a cap).
- Breathe out fully-away from the inhaler. Never exhale into it.
- Put the mouthpiece in your mouth and seal your lips tightly.
- Breathe in quickly and deeply-like you’re trying to suck a thick milkshake through a straw.
- Hold your breath for 10 seconds.
- Breathe out slowly.
Don’t try to use a DPI if you’re having a flare-up. If you’re gasping for air, you won’t be able to inhale hard enough. That’s when you need an MDI with a spacer. DPIs also don’t work with spacers. If you try to attach one, you’ll block the powder and get almost nothing into your lungs.
And never open the capsule or try to pour the powder out. That’s a common mistake. The powder is designed to be inhaled only through the device. If you spill it, you’re wasting your dose.
Why Spacers Are a Game-Changer (But Only for MDIs)
If you’re using an MDI, a spacer is your best friend. It’s a plastic tube you attach to the inhaler. You spray the medicine into the spacer, then breathe in slowly from the other end. It eliminates the need to time your breath perfectly. Studies show spacers increase lung delivery by 70-100% compared to MDIs alone.
And here’s why this matters: a 2022 Asthma UK survey found that 78% of users who added a spacer reported better symptom control. That’s not a small improvement. That’s life-changing.
Spacers are especially helpful for kids, older adults, and anyone who struggles with coordination. The National Asthma Council Australia recommends them for everyone using an MDI. And yes, you can clean them. Wash them once a week with warm water and dish soap. Don’t dry them with a towel-let them air dry. A damp spacer works better than a dusty one.

Common Mistakes (And How to Fix Them)
Here are the mistakes most people make-and how to stop them:
- Not shaking the MDI - 45% of users skip this. Shake it for 5 seconds. Always.
- Exhaling into the inhaler - 27% do this. Breathe out away from the device first.
- Not holding your breath - 63% of patients don’t hold for 10 seconds. That’s the most important step. It’s what lets the medicine stick to your airways.
- Using DPIs with spacers - This cuts effectiveness by 50-70%. Never do it.
- Storing inhalers in hot places - Above 30°C, the medicine loses 15-20% of its potency. Keep it at room temperature.
And one more: rinsing your mouth after using steroid inhalers. If you don’t, you risk oral thrush-a fungal infection that causes white patches and soreness. Rinsing reduces that risk by 75%. Just swish water or mouthwash and spit it out. Don’t swallow it.
What to Do If You’re Still Struggling
If you’re still having trouble, you’re not alone. On Reddit’s asthma community, 68% of users said they didn’t get it right until they had multiple doctor visits. A Drugs.com survey found 37% of users didn’t even know if they were using their inhaler correctly.
Here’s what to do:
- Ask your doctor or nurse to watch you use your inhaler during your next visit. Don’t just say “I know how to use it.” Show them.
- Watch a video from a trusted source-American Lung Association, Asthma UK, or the NHS. Don’t rely on random YouTube videos.
- Ask for a spacer if you’re using an MDI. They’re cheap, often free with prescriptions, and work better than any fancy new inhaler.
- If you’re over 65 or have severe COPD and can’t breathe hard enough for a DPI, ask about switching to a soft mist inhaler or MDI with spacer.
Some people are now using smart inhalers-devices with sensors that track when you use them and whether your technique was right. The FDA approved the first one in 2021. By 2025, 40% of inhalers are expected to have this tech. But even if you don’t have one, you can still get it right. You don’t need tech. You just need to learn.
What’s Next? Don’t Just Get a Prescription-Get Trained
Doctors are supposed to check your inhaler technique at every visit. The National Asthma Education and Prevention Program says so. And it works: a 2023 JAMA study found patients who had their technique checked had 22% fewer emergency room visits.
But too often, it’s skipped. So if your provider doesn’t ask you to demonstrate your technique, ask them. Say: “Can you watch me use my inhaler? I want to make sure I’m getting the full benefit.”
This isn’t about being perfect. It’s about getting enough medicine into your lungs so you don’t have to suffer. So you can walk up stairs without gasping. So you can sleep through the night. So you don’t end up in the hospital because a $50 inhaler didn’t work-not because it was broken, but because you didn’t know how to use it.
You’ve got the medicine. Now make sure it does its job.
Can I use my inhaler without shaking it?
No. Shaking your metered-dose inhaler (MDI) for 5 seconds before each puff ensures the medicine and propellant are properly mixed. If you skip this, you might get too much propellant and not enough medicine-or vice versa. Studies show 45% of users forget to shake, which leads to inconsistent dosing and poor symptom control.
Is it okay to use a spacer with a dry powder inhaler?
No. Spacers are designed only for metered-dose inhalers (MDIs). Using a spacer with a dry powder inhaler (DPI) blocks the airflow needed to lift the powder into your lungs. Research shows this cuts medication delivery by 50-70%. DPIs rely on your strong, fast inhalation to work. A spacer prevents that.
Why does my inhaler not seem to work anymore?
It’s rarely because the inhaler is empty. More often, it’s because your technique has slipped. Many people stop holding their breath for 10 seconds, forget to shake the inhaler, or breathe in too fast or too slow. If your symptoms are worse, check your technique first. Then check the counter on your inhaler. Most have a dose counter-use it.
Should I rinse my mouth after using my inhaler?
Yes-if it contains a corticosteroid (like fluticasone, budesonide, or beclomethasone). Rinsing reduces the risk of oral thrush by 75%. Swish water or mouthwash for 10 seconds and spit it out. Don’t swallow it. This is especially important for people who use steroid inhalers daily.
Can I use my inhaler if I’m having a severe attack?
Yes-but only if it’s an MDI, preferably with a spacer. Dry powder inhalers (DPIs) require a strong, fast breath to work. During a severe attack, you may not be able to generate enough airflow. An MDI with a spacer lets you breathe in slowly and still get the medicine. If your rescue inhaler isn’t helping, call for emergency help immediately.
How do I know if my inhaler is empty?
Most modern inhalers have a dose counter that shows how many puffs are left. If yours doesn’t, check the expiration date and count your puffs. A standard MDI has 120 or 200 puffs. If you use two puffs twice a day, it’ll last about 30 days. Never rely on how it feels when you spray it-empty inhalers can still make a sound.



Comments
9 Comments
Kuldipsinh Rathod
I used to mess up my MDI all the time-shook it, but never held my breath. Then my nurse made me demo it during a checkup. I felt so dumb. But after learning to wait 60 seconds between puffs? My inhaler finally worked. No more midnight wheezing. Just… breathing. Thanks for the reminder.
SHAKTI BHARDWAJ
OMG I HATE THESE INHALERS SO MUCH!! WHY DO I HAVE TO BREATHE IN LIKE I’M TRYING TO SUCK A MOUNTAIN THROUGH A STRAW?? MY GRANDMA CAN’T EVEN DO IT AND SHE’S GOT COPD!! AND WHY DO I HAVE TO RINSE MY MOUTH?? I JUST WANT TO FEEL BETTER NOT BE A LAB RAT!!
Jody Kennedy
Y’ALL. THIS. IS. LIFE-CHANGING. I used to think my inhaler was broken because I still felt like I was drowning. Then I watched the American Lung Association video. Used a spacer. Held my breath. And-holy heck-I actually felt it working. I’m not exaggerating: I walked to my mailbox today without stopping. I cried. If you’re still struggling, just try the spacer. It’s free. It’s easy. It’s magic.
christian ebongue
shaking the inhaler = non-negotiable. forgot to do it for 3 months. thought my meds were expired. turned out i was just lazy. also, spacers are the unsung heroes of respiratory care. no cap.
jesse chen
I’ve been using my DPI for years, and I just realized I was breathing out INTO it. I’m so embarrassed. I thought I was ‘clearing my lungs’ before inhaling. Turns out, I was just wasting medicine. I’m going to rewatch the video tonight. Thanks for pointing this out-this is the kind of info no one tells you.
Prasanthi Kontemukkala
For anyone struggling with DPIs-especially if you’re older or have weak lungs-don’t feel bad. It’s not you, it’s the device. My mom switched to a Respimat last year and now she’s gardening again. Talk to your doctor about alternatives. You deserve to breathe easy. And yes, rinse your mouth. It’s simple, and it saves you from thrush. Tiny habit, huge difference.
Alex Ragen
It’s fascinating, really-the profound epistemological dissonance between medical prescription and patient execution. We are told to ‘inhale deeply,’ yet the physiological capacity to do so is systematically eroded by disease, age, and environmental degradation. The inhaler, then, becomes a symbol of neoliberal healthcare: a tool that demands perfect compliance from those least equipped to comply. And yet, we blame the patient.
Lori Anne Franklin
my inhaler counter says 23 left but it still sounds like it has stuff in it so i keep using it… is that bad? 😅
Bryan Woods
Thank you for the comprehensive breakdown. The data on spacer efficacy and the 60-second interval between puffs are critical points often omitted in clinical settings. I recommend printing this guide and sharing it with patients. Proper inhaler technique is not an ancillary detail-it is the cornerstone of effective respiratory management.
Write a comment