Every month, pharmacists face the same frustrating pattern: a patient walks in two weeks early for a 30-day supply of oxycodone, claiming their doctor said it was okay. Another comes in with a new script for gabapentin-same dose, same pharmacy, just a different prescriber. These aren’t just inconveniences. They’re red flags for early refills and duplicate therapy, two of the most dangerous medication errors in community and clinical pharmacy today.
It’s not just about breaking rules. It’s about preventing overdose, stopping drug diversion, and making sure patients get the right treatment without harmful overlaps. The CDC says medication non-adherence contributes to 125,000 deaths a year in the U.S. alone-and early refills are often the first sign someone’s slipping out of safe care. In the UK and elsewhere, similar risks exist, even if the systems look different.
Why Early Refills Are a Red Flag
Early refills don’t always mean misuse. Maybe the patient lost their pills. Maybe they traveled. Maybe they’re in pain and their insurance won’t cover a new prescription until day 28. But when early refills happen month after month-especially for controlled substances-it’s rarely coincidence.
According to DEA guidelines, Schedule II drugs like oxycodone, fentanyl, and Adderall cannot be refilled under any circumstances. Yet many patients still show up asking for them. Some say their doctor wrote it. Others claim their insurance allows a 5-day early refill. And yes, some will offer to pay cash, thinking that removes the problem.
The truth? Most insurance plans allow a 5-day early refill on 30-day prescriptions-but only once, and only if the prescription is still active. That doesn’t mean it’s okay to come in early every month. Pharmacists who ignore this pattern are enabling risky behavior.
One Bristol pharmacy reported a patient who filled a 30-day supply of tramadol every 18 days for six months. When they checked the NHS Prescription Service, they found the same patient had gotten another tramadol script from a different GP clinic two weeks earlier. That’s duplicate therapy. And it’s exactly how overdoses start.
Duplicate Therapy: When Two Prescriptions Do the Same Thing
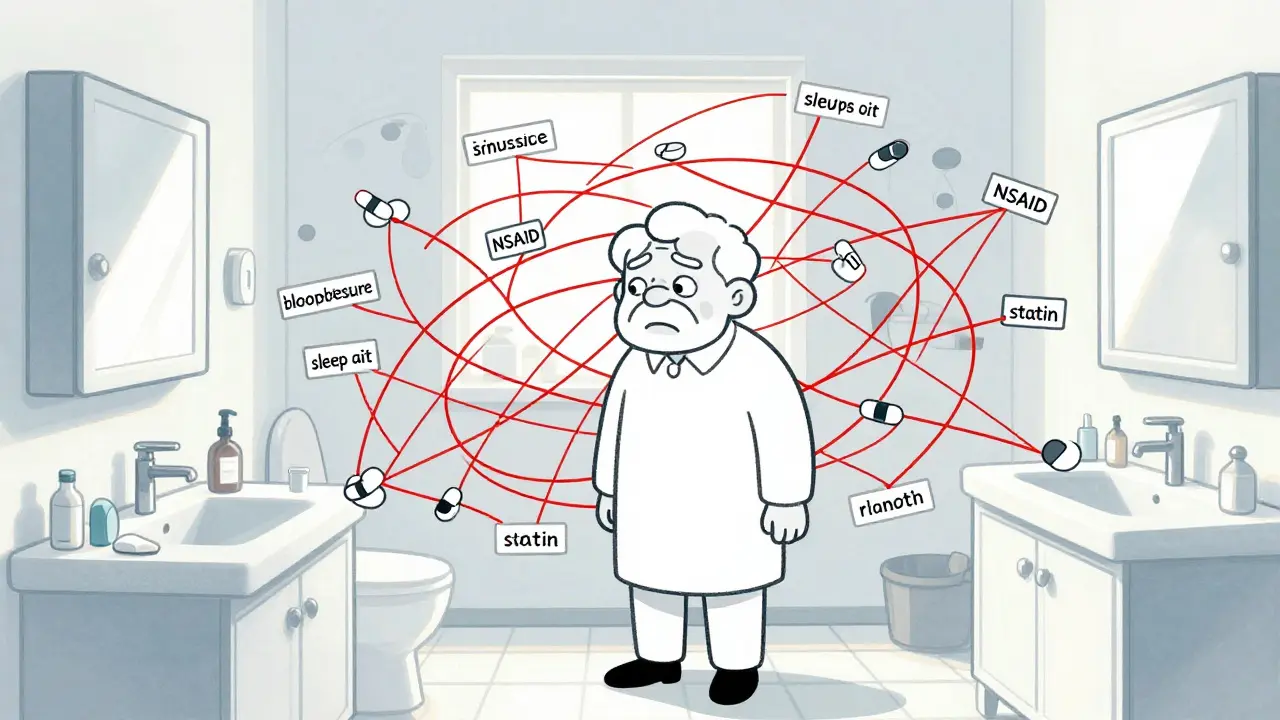
Duplicate therapy happens when a patient gets two or more drugs that do the same thing-like two different SSRIs, two different NSAIDs, or two different gabapentin formulations. Sometimes it’s accidental. Sometimes it’s intentional.
Patients might visit multiple doctors to get around refill limits. They might not remember what they’re already taking. Or they might think, “If one pill helps, two will help more.” That’s dangerous. Combining two benzodiazepines, for example, can cause respiratory depression. Taking two different blood pressure meds without coordination can crash your systolic pressure into the 80s.
Pharmacists are often the last line of defense. A 2023 study in the Journal of Pharmacy Practice found that 37% of duplicate therapy cases were caught by pharmacists during dispensing-not by prescribers. But you can’t catch what you can’t see.
That’s why access to clinical viewers matters. In the UK, the NHS Spine gives pharmacists real-time access to prescriptions filled across the country. If a patient gets a prescription in London and then comes to your Bristol pharmacy two weeks later for the same drug, the system flags it. If they’re using private clinics or out-of-area GPs, those records might not show up. That’s why you need to ask.
How to Build a Refill Protocol That Works
Waiting for patients to call or show up is reactive. It’s chaotic. And it’s how mistakes happen. The best pharmacies don’t wait-they plan.
Start by categorizing medications into three tiers:
- Low-risk: Nasal steroids, thyroid meds, some antidepressants. These can often be refilled automatically every 90 days if the patient has had a check-up in the last 6 months.
- Medium-risk: Antihypertensives, diabetes meds, statins. These need a 3-month refill window, but only if the patient has had labs or a visit in the last 90 days.
- High-risk: Opioids, benzodiazepines, stimulants. No automatic refills. No early fills. Every request requires direct provider approval.
Then build your workflow around it. When a refill request comes in:
- Check the date of the last fill. Is it within the allowed window?
- Check the NHS Spine or other clinical viewer for duplicates.
- Check if the patient has had a recent visit or lab test (e.g., HbA1c for diabetes, liver enzymes for statins).
- If it’s high-risk, call the prescriber. Don’t assume they know what the patient is taking elsewhere.
- If it’s outside the window and there’s no valid reason, say no-and document why.
One practice in Bristol cut early refill requests by 68% in six months after implementing this system. Staff didn’t have to scramble. Patients knew the rules. And no one got a dangerous combo of painkillers.
Technology Is Your Ally, Not Your Enemy
Electronic Health Records (EHRs) and pharmacy management systems can do the heavy lifting-if they’re set up right.
Make sure your system:
- Flags early refill attempts with a red alert
- Automatically checks for duplicate prescriptions across all providers
- Shows recent lab results tied to the medication (e.g., creatinine for ACE inhibitors)
- Has a note field where pharmacists can write: “Patient received same med from Dr. Smith on 1/10/2026-confirmed duplicate”
Don’t rely on memory. Don’t assume the patient told you the truth. Use the tools you have. The NHS has invested in digital infrastructure for a reason. Use it.
And if your system doesn’t do this? Push for it. Talk to your manager. Show them the data. A 2022 study in PMC found that health systems using automated refill protocols reduced provider workload by 40% and cut medication errors by 52%.
What to Do When a Patient Gets Angry
Some patients will get upset. “I’ve been taking this for years!” “My doctor said I could get it early!” “I’m in pain!”
Stay calm. Stay professional. Say this:
“I understand you’re in pain, and I want to help. But I need to make sure you’re not getting too much of this medication. Let me check with your doctor to see if we can adjust your plan safely.”
Never argue. Never say, “You’re trying to get drugs.” That shuts down communication. Instead, make it about safety. About care. About doing the right thing together.
Some patients will walk out. That’s okay. Better they walk out than overdose next week.

Training Your Team Is Non-Negotiable
One pharmacist can’t catch everything. But a trained team can.
Every staff member-pharmacists, technicians, receptionists-needs to know:
- What counts as an early refill
- Which drugs are high-risk
- How to use the clinical viewer
- When to escalate to a pharmacist
- How to document every interaction
Run monthly 15-minute huddles. Review one case. Ask: “What did we miss? What could we have done better?”
Make it part of your culture. Not a checklist. Not a rule. A habit.
What’s Next? The Bigger Picture
Preventing early refills and duplicate therapy isn’t just about stopping bad behavior. It’s about building trust.
When patients know you’re looking out for them-not just filling scripts-they’re more likely to be honest. They’re more likely to say, “I’ve been taking extra because the pain came back.” That’s the moment you can help.
Work with GPs. Share concerns. Suggest follow-ups. Offer to send a note: “Patient presented for early refill of oxycodone. No recent visit. No lab results. Recommended follow-up.”
That’s not overstepping. That’s being a pharmacist.
The opioid crisis didn’t happen because of one bad actor. It happened because systems failed. People slipped through cracks. Prescriptions were filled without context.
You don’t have to fix everything. But you can stop one error. One early refill. One duplicate script. That’s enough to save a life.




Comments
8 Comments
Timothy Davis
Let’s be real-most of these ‘early refill’ cases are just patients with chronic pain who’ve been abandoned by the system. You want to stop abuse? Start by fixing the 12-month waiting period for pain specialists. Until then, you’re just punishing people who can’t get care. And no, ‘documenting’ doesn’t fix structural failure.
fiona vaz
I’ve used the NHS Spine for years-it’s lifesaving. But in rural clinics? No access. No training. Just a stressed pharmacist and a panicked patient. The tech exists. The will doesn’t. Push for funding. Don’t just wait for it to magically appear.
Sue Latham
OMG I can’t believe some of you are actually defending these people. Like, no-just no. If someone’s coming in every 18 days for oxycodone, they’re not in pain, they’re addicted. And you’re enabling them. Stop being so soft. Say no. Period.
John Rose
Great breakdown. I’ve seen this exact scenario in my clinic-patient gets gabapentin from two docs, one for ‘nerve pain,’ the other for ‘anxiety.’ Both were legit prescriptions, but neither knew the other existed. We built a simple checklist: 1) Check script date 2) Cross-reference with EHR 3) Call prescriber if duplicate suspected. Cut our error rate by 70% in four months. It’s not magic-it’s discipline.
Lexi Karuzis
Wait… so you’re saying the government’s digital system is reliable? LOL. The NHS Spine? That’s the same system that lost 17 million records in 2021. And you trust it to stop overdoses? What about the black-market scripts from Mexico? The fake online prescribers? The DEA doesn’t even track those! You’re all just playing pretend with spreadsheets while people die. Wake up!
Brittany Fiddes
Oh, please. You Americans think your ‘protocols’ are some grand innovation. In the UK, we’ve had real-time prescription monitoring since 2014. We don’t need ‘tiered systems’-we have a national database that flags duplicates before the patient even walks in. Your ‘Bristol pharmacy’ story? Cute. We’ve been doing this since before you had smartphones. Honestly, it’s embarrassing you still treat this like a novel concept.
Phil Davis
Ironically, the most effective tool here isn’t the software-it’s the silence. When you say ‘I need to check with your doctor,’ you’re not denying care-you’re creating space for honesty. I’ve had patients break down and admit they were hoarding pills after losing their job. That conversation? That’s the real intervention. Not the red flag. Not the system. The human moment.
Anna Lou Chen
What you’re describing is merely a symptom of late-stage biomedical capitalism’s failure to decouple care from commodification. The pharmacy, as an institution, has been co-opted into a logistical node of pharmaceutical extraction-replacing therapeutic presence with algorithmic gatekeeping. Your ‘tiered system’ is just a neoliberal veneer over structural violence. True harm reduction requires dismantling the prescriptive hierarchy-replacing it with community-based, non-hierarchical, trauma-informed care models. Until then, you’re just optimizing the machine that’s killing people.
Write a comment