Skipping a pill here and there might seem harmless-maybe you forgot, or the cost was too high, or you felt fine and thought you didn’t need it anymore. But when you don’t take your medication exactly as your doctor ordered, the risks aren’t just theoretical. They’re real, measurable, and often deadly.
Every Missed Dose Adds Up
Doctors don’t prescribe medications randomly. The dosage, timing, and duration are based on years of clinical research. For chronic conditions like high blood pressure, diabetes, or depression, even small lapses can undo the progress you’ve made. Studies show that medication nonadherence is responsible for up to 50% of treatment failures across all major diseases. That means if you’re not taking your pills as directed, your treatment isn’t working-not because the drug is ineffective, but because you’re not giving it a chance.
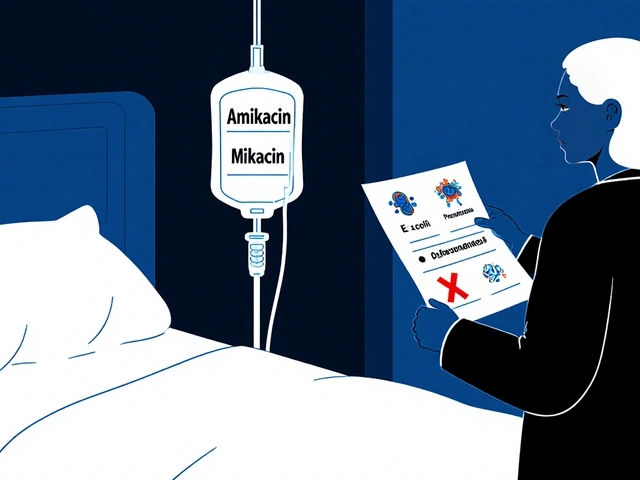
Take blood pressure medication. If you skip doses, your pressure spikes unpredictably. That puts stress on your heart, kidneys, and brain. Over time, this increases your risk of stroke, heart attack, or kidney failure. The same goes for statins: missing doses lets cholesterol build back up, silently damaging your arteries. And for antibiotics? Stopping early doesn’t just make your infection worse-it creates superbugs that resist treatment.
The Human Cost: Lives Lost
It’s not just about feeling unwell. Nonadherence kills. In the United States alone, an estimated 125,000 deaths each year are directly linked to people not taking their medications as prescribed. For people over 50, that risk jumps to 30 times higher than the risk of being murdered. In the UK and across Europe, similar patterns emerge. The World Health Organization says medication adherence has a bigger impact on survival than the actual drug itself.
Older adults are especially vulnerable. One in five hospital readmissions within 30 days is tied to missed medications. That’s not just bad luck-it’s preventable. ChenMed estimates 100,000 elderly deaths annually in the U.S. could be avoided if people took their drugs consistently. And it’s not just the elderly. People with mental health conditions like schizophrenia or bipolar disorder are 59% more likely to skip their meds, leading to relapses, emergency room visits, and tragically, suicide.
The Financial Toll on You and the System
Skipping pills doesn’t just hurt your body-it hurts your wallet. In 2016, the total cost of nonadherence in the U.S. hit $529 billion. That includes hospital stays, emergency care, lost wages, and long-term disability. On average, each patient who doesn’t take their meds adds between $5,271 and $52,341 in extra healthcare costs over time.
And it’s not just the system paying. Out-of-pocket drug costs rose 4.8% in 2021 to $63 billion. That’s why 8.2% of working-age adults in the U.S. admitted they didn’t take their medication because they couldn’t afford it. In the UK, while the NHS covers most prescriptions, people on low incomes still struggle with co-pays, travel to pharmacies, or buying over-the-counter aids to manage side effects. The result? A vicious cycle: high cost → skipped doses → hospitalization → even higher bills.
Why Do People Skip Their Meds?
It’s never just one reason. People miss doses for complex, layered reasons:
- Cost-The biggest barrier. Even with insurance, co-pays for chronic meds can hit £50+ a month.
- Side effects-Nausea, dizziness, weight gain-people stop because they feel worse, not better.
- Complex regimens-Taking five different pills at three different times a day? It’s easy to get confused.
- Feeling fine-If you don’t feel symptoms, you think you’re cured. But hypertension doesn’t scream. Diabetes doesn’t shout.
- Poor communication-Many patients don’t understand why the drug matters or what happens if they stop.
- Stigma-Especially with mental health meds, people hide them, avoid refills, or quit to avoid judgment.
And it gets worse over time. Adherence drops steadily after the first few weeks. A pill you took religiously in January? By June, it’s an afterthought.
Who’s Most at Risk?
Nonadherence doesn’t affect everyone equally. People in low-income communities, minority groups, and rural areas face higher barriers. Pharmacy deserts-areas without a nearby pharmacy-are common in parts of the UK and the U.S. Older adults juggle multiple prescriptions. People with mental illness often lack consistent care. And those with low health literacy don’t know how to read labels, understand dosing, or ask questions.
These aren’t personal failures. They’re systemic failures. The healthcare system expects patients to navigate complexity without support, then blames them when things go wrong.

What Actually Works to Fix This?
There are solutions-and they’re proven.
- Pharmacist-led counseling-Patients who meet with a pharmacist to review their meds see 15-20% improvement in adherence.
- Text message reminders-Simple, free, and effective. Studies show 12-18% better adherence with daily texts.
- Pill organizers-Blister packs or weekly boxes reduce confusion. Many pharmacies now offer them for free.
- Medication therapy management (MTM)-A structured review of all your drugs by a pharmacist. It saves money: for every £1 spent, £3-£10 is saved in avoided hospital care.
- Reducing pill burden-Doctors can often switch to combination pills or once-daily options.
The biggest barrier? Most of these services aren’t covered by insurance. Pharmacist time, home delivery, adherence packaging-they’re not reimbursed. So even though they work, they’re rarely offered.
What You Can Do Right Now
You don’t need a perfect system. Start small:
- Set a daily phone alarm for each medication. Name it clearly: “Blood Pressure AM,” “Diabetes Lunch.”
- Use a pill box. Buy one for £5 at any pharmacy. Fill it weekly.
- Ask your doctor: “Can I switch to a once-a-day version?” or “Is there a cheaper alternative?”
- Ask your pharmacist: “Can you pack my meds in a blister pack?” Most will do it free.
- If you’re skipping meds because of side effects-don’t quit. Call your doctor. There’s often a fix.
- Keep a log. Write down when you take your meds. It helps you spot patterns and gives your doctor real data.
And if cost is the issue: ask about patient assistance programs. Many drug makers offer free or low-cost meds to those who qualify. NHS in the UK offers prepayment certificates for people on multiple prescriptions. Don’t assume you can’t afford it-ask.
The Bigger Picture
This isn’t just about you taking your pills. It’s about a broken system that treats adherence like a personal responsibility instead of a public health priority. But your choices matter. Every pill you take is a step away from hospitalization, disability, or death. And every time you speak up-about cost, side effects, confusion-you help change the system for others too.
Medications are powerful tools. But they only work if you use them. Your doctor gave you a prescription. Now it’s your turn to honor it-not because you have to, but because you deserve to stay healthy.
What happens if I miss one dose of my medication?
It depends on the drug. For some, like blood pressure or cholesterol meds, skipping one dose won’t cause immediate harm, but it lowers your overall protection. For others, like antibiotics or insulin, missing even one dose can lead to serious complications. Always check the patient leaflet or call your pharmacist. Never double up unless instructed.
Why do I feel worse when I start a new medication?
Many medications cause temporary side effects as your body adjusts-nausea, dizziness, fatigue. These often fade after a week or two. But if symptoms are severe or persistent, don’t stop the drug. Contact your doctor. They may adjust the dose, switch the medication, or add a helper drug to ease the side effects.
Can I stop my medication if I feel better?
For chronic conditions like hypertension, diabetes, or depression, feeling better means the medication is working-not that you’re cured. Stopping can cause your condition to return, often worse than before. Always talk to your doctor before stopping. Some drugs, like steroids or antidepressants, need to be tapered slowly to avoid withdrawal.
How do I know if I’m adherent enough?
Experts say you need to take at least 80% of your prescribed doses to get full benefit. That means missing no more than 2-3 doses a month on a daily regimen. If you’re missing more than that, it’s time to find a solution-whether it’s a pill box, reminders, or talking to your doctor about cost or side effects.
Are there free tools to help me remember my meds?
Yes. Many free apps like Medisafe, MyTherapy, or even Google Calendar alarms can send reminders. Pharmacies often give out free pill organizers. NHS pharmacies in the UK offer free blister packs for people on multiple medications. Ask your pharmacist-they’re trained to help with this.
What if I can’t afford my prescription?
Don’t skip doses because of cost. Ask your doctor if there’s a generic version. Many brand-name drugs have cheaper generics with the same active ingredient. In the UK, ask about a Prescription Prepayment Certificate (PPC) if you need multiple prescriptions. In the U.S., check RxAssist or patient assistance programs from drug manufacturers. Pharmacies sometimes offer discount cards. Never go without because you think you can’t pay-there’s always a way.


Comments
13 Comments
Deepika D
Look, I get it-life gets crazy. I’m a nurse in Mumbai, and I’ve seen patients skip insulin because they can’t afford the co-pay, or forget their blood pressure pills because they’re juggling three jobs. But here’s the thing: adherence isn’t about willpower, it’s about design. If your regimen is a maze, the system failed you, not you. Try a pill organizer from the pharmacy-they’re free. Set a phone alarm named ‘Heart Alive AM.’ Tell your doc: ‘I need simpler.’ You’re not lazy. You’re just not supported. And you deserve better.
Stewart Smith
So let me get this straight-we’re blaming people for not taking pills while the same system charges $500 for a 30-day supply of metformin? Cool. Real cool. 😒
Chandreson Chandreas
Man, I used to skip my antidepressants when I felt ‘better.’ Thought I was cured. Then I crashed harder than a phone in a toilet. 🤕 Now I take ‘em every day, even if I’m vibing. The meds ain’t magic-they’re scaffolding. And sometimes, scaffolding feels like a cage. But hey, better a cage than a fall, right? 🙏
Aaron Bales
80% adherence is the threshold. Miss more than 2-3 doses/month on daily meds? You’re not optimizing. Use free apps like Medisafe. Pharmacies give out blister packs. Ask for generics. Done.
Lawver Stanton
Oh, so now it’s MY fault my blood pressure meds cost $200 a month? Let me guess-you’ve never had to choose between insulin and groceries? You know what’s worse than skipping a pill? Being told you’re ‘noncompliant’ while your insurance company makes $12 billion in profit. This isn’t about discipline-it’s about capitalism eating your health alive. And now you want me to feel guilty? Nah. I’ll keep living. You keep preaching.
Harriet Hollingsworth
People who skip meds are just selfish. They don’t think about the ER nurses, the paramedics, the families who lose them. It’s not just about them-it’s about all of us paying for their negligence. If you can’t be responsible for your own body, you don’t deserve to be part of a society that cares.
Darren Pearson
It is, of course, axiomatic that pharmacological adherence constitutes a fundamental pillar of therapeutic efficacy. The WHO’s meta-analyses on nonadherence are not merely suggestive-they are statistically definitive. One might posit that the moral imperative to adhere is not merely clinical, but sociopolitical, given the aggregate fiscal burden on public health infrastructure.
Bennett Ryynanen
Bro, I was on 7 pills a day. Felt like a pharmacy. Then I asked my doc if I could combo them. Got switched to 3 once-a-day. Life changed. No magic. Just ask. Your doc wants you to get better. They’re not here to judge. Talk to them. Or your pharmacist. They’re the real MVPs.
Sara Stinnett
Oh, so now we’re glorifying compliance as virtue? What’s next-blaming people for getting sick because they didn’t meditate enough? This post reads like a pharmaceutical ad disguised as public service. The real villain isn’t the patient who skips a pill-it’s the system that turns medicine into a luxury good and then calls them lazy. Wake up.
Martin Viau
Canada’s got free prescriptions for seniors. Why doesn’t the U.S.? Because we’re a nation that’d rather let people die than tax the rich. You want adherence? Make meds affordable. Stop blaming the sick. This isn’t a moral failure-it’s a policy failure. And if you’re still blaming patients, you’re part of the problem.
Jenny Salmingo
I’m from the Philippines and my mom takes 5 meds. She uses a plastic box with morning/afternoon/evening slots. I fill it every Sunday. We set a WhatsApp alarm. Simple. Free. Works. You don’t need tech. You need someone who cares. And you deserve that.
Retha Dungga
we are all just trying to survive and sometimes the pills are just another thing that reminds you you're not free 🌿💔
Robb Rice
As someone who’s been on long-term statins and metformin for over a decade, I can say this: consistency isn’t about discipline-it’s about routine. I take mine with my morning coffee. No thought. No guilt. No drama. If you’re struggling, start there. Pair it with something you already do. And if cost is the issue? Talk to your pharmacist. They’ve got resources. And if you’re still unsure? Call your doctor. They’re not here to shame you. They’re here to help. I’ve been there. You’re not alone.
Write a comment