Antibiotic Selection Assistant
Antibiotic Selection Tool
This tool helps healthcare professionals determine the best antibiotic choice for serious bacterial infections based on key factors like infection type, patient condition, and resistance patterns.
Recommended Antibiotic
Key considerations:
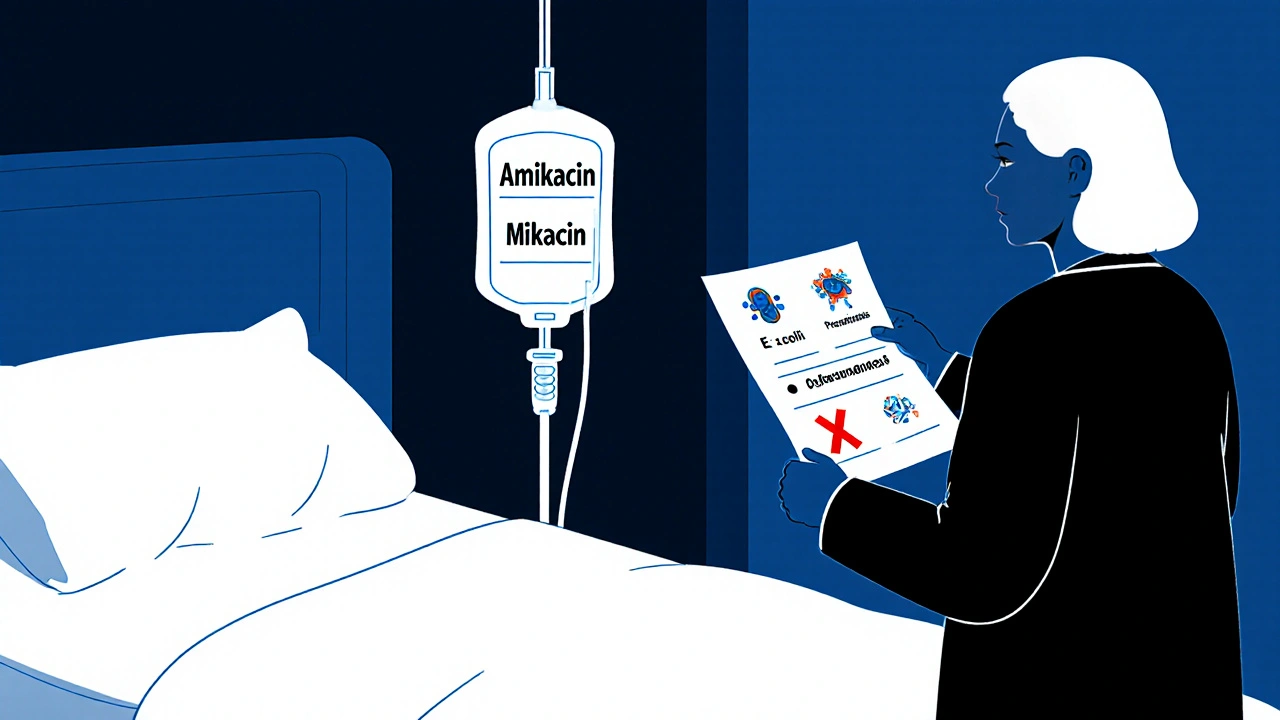
- Amikacin (Mikacin) - Best for resistant Gram-negative infections
- Piperacillin-Tazobactam - Safer alternative for many infections
- Meropenem - For severe carbapenem-resistant infections
When a serious bacterial infection hits hard - like sepsis, pneumonia in ICU patients, or a resistant urinary tract infection - doctors don’t waste time. They reach for powerful antibiotics. One of them is Mikacin Injection, which contains amikacin. It’s a last-line defense, often used when other antibiotics have failed. But it’s not the only option. And not always the best one. So how does it stack up against other antibiotics? And when should a doctor pick something else?
What is Mikacin Injection (Amikacin)?
Mikacin Injection is a brand name for amikacin, an aminoglycoside antibiotic. It works by breaking down the protein-making machinery inside bacteria. Without functional proteins, the bacteria can’t survive or multiply. It’s especially effective against Gram-negative bugs like E. coli, Klebsiella, and Pseudomonas aeruginosa. These are the kinds of bacteria that often cause hospital-acquired infections.
Amikacin is given by injection - either into a muscle or through an IV. It doesn’t work as a pill because the body can’t absorb it well through the gut. It’s usually used in hospitals, not at home. The typical dose is 15 mg per kg of body weight, given every 8 to 12 hours. Treatment lasts 7 to 14 days, depending on the infection.
But here’s the catch: amikacin is tough on the body. It can damage your kidneys and hearing. That’s why doctors monitor blood levels and kidney function closely during treatment. It’s not something you take lightly - or for long.
Why Look for Alternatives?
Amikacin has a narrow window between helping and harming. A little too much, and you risk permanent hearing loss or kidney failure. A little too little, and the infection doesn’t budge. That’s why doctors often try alternatives - especially if the patient is older, has existing kidney problems, or is on other drugs that stress the kidneys.
Also, resistance is growing. Some strains of bacteria have evolved enzymes that break down amikacin before it can work. In those cases, even a high dose won’t help. That’s when switching to another antibiotic becomes necessary.
Alternative 1: Gentamicin
Gentamicin is the most common alternative to amikacin. Like amikacin, it’s an aminoglycoside. But there are key differences.
Gentamicin is cheaper and more widely available. It’s often the first choice in many hospitals for Gram-negative infections. It’s also effective against the same bugs - E. coli, Klebsiella, and Pseudomonas.
But gentamicin has a higher risk of kidney damage than amikacin in some studies. It’s also more likely to be neutralized by bacterial enzymes. That means if a strain is resistant to gentamicin, it’s probably resistant to amikacin too - but not always the other way around.
Amikacin wins in one area: resistance. Because it’s used less often than gentamicin, fewer bacteria have learned how to fight it. So if gentamicin fails, amikacin often still works.
Alternative 2: Ceftriaxone
Ceftriaxone is a third-generation cephalosporin. It’s given as an IV or IM injection, just like amikacin. But it’s not an aminoglycoside - it’s a beta-lactam antibiotic.
This matters because ceftriaxone is much gentler on the kidneys. It doesn’t cause hearing loss. That makes it a safer choice for elderly patients or those with chronic kidney disease.
It’s very effective against common hospital infections like pneumonia, meningitis, and bloodstream infections caused by susceptible bacteria. But it doesn’t work against all Gram-negative bugs. For example, it’s weak against Pseudomonas aeruginosa - one of the main targets of amikacin.
Doctors often pair ceftriaxone with another drug like gentamicin or amikacin when treating severe infections. This combo hits the bacteria with two different attack methods, making it harder for them to survive.
Alternative 3: Piperacillin-Tazobactam
This combo drug - a penicillin-type antibiotic with a beta-lactamase inhibitor - is now one of the most common go-to treatments in ICUs for severe infections.
Piperacillin-tazobactam covers a wider range of bacteria than amikacin, including many Gram-positive bugs, anaerobes, and even some Pseudomonas strains. It’s also safer for the kidneys and ears.
Studies from 2023 show it’s just as effective as amikacin plus other antibiotics for treating hospital-acquired pneumonia and complicated urinary tract infections. And because it’s given as a single IV infusion, it’s easier to manage than multiple daily injections.
The downside? It’s more expensive. And in places where carbapenem-resistant bacteria are common, even piperacillin-tazobactam can fail. That’s when amikacin still has a role.

Alternative 4: Meropenem
Meropenem is a carbapenem antibiotic - one of the strongest in the class. It’s used for the most serious, multi-drug resistant infections.
It works against nearly all Gram-negative bacteria, including those that make enzymes to destroy other antibiotics. That includes many strains that resist amikacin. It’s often the drug of choice for sepsis caused by ESBL-producing bacteria.
But meropenem is reserved for the worst cases. Why? Because overuse leads to resistance. Hospitals keep it locked away for emergencies. If a patient can be treated with amikacin or piperacillin-tazobactam, they’ll get that first.
Meropenem is also safer for kidneys than amikacin. But it’s not risk-free - it can cause seizures in patients with brain injuries or kidney failure. That’s why it’s used under close supervision.
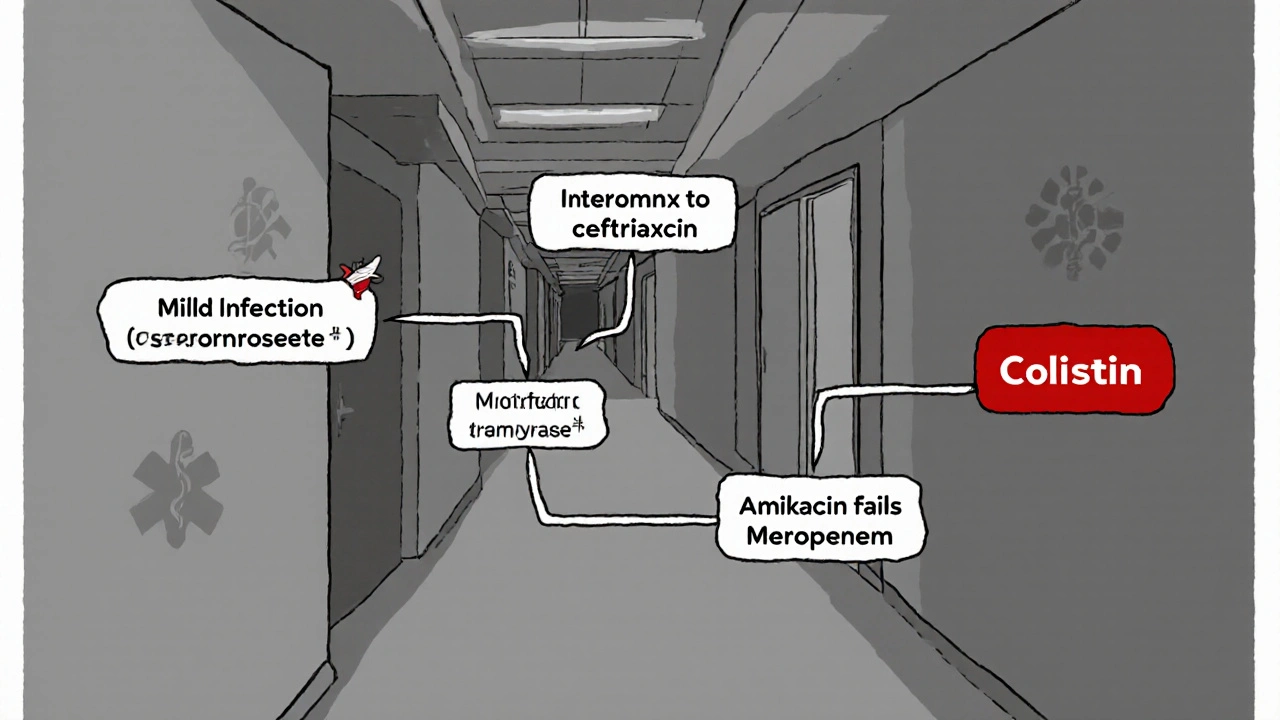
Alternative 5: Colistin
Colistin is an old antibiotic, revived because newer drugs no longer work on some superbugs. It’s used when every other option has failed - including amikacin.
It’s extremely toxic. It can cause severe kidney damage in over 50% of patients. Hearing loss is also common. But for infections caused by carbapenem-resistant Acinetobacter or Klebsiella, it might be the only thing left.
Doctors avoid colistin unless absolutely necessary. It’s usually given in combination with other drugs to reduce the dose and lower the risk. In many hospitals, it’s a last-resort option - even after amikacin has been tried.
When Is Amikacin the Best Choice?
Amikacin isn’t the first drug you’d pick. But it shines in three situations:
- When gentamicin or tobramycin have failed - because amikacin resists the enzymes that break down those drugs.
- In patients with known or suspected resistant infections - especially in ICU settings where drug-resistant bacteria are common.
- When a patient has allergies to beta-lactams - like penicillins or cephalosporins - and other options are limited.
It’s also preferred in neonatal sepsis in some countries, because it crosses the placenta well and has a proven track record in newborns.
What About Oral Antibiotics?
You can’t swap amikacin for an oral pill. It doesn’t work that way. But once the infection is under control, doctors often switch from IV amikacin to an oral antibiotic to finish the course.
Common follow-up options include ciprofloxacin, levofloxacin, or trimethoprim-sulfamethoxazole - depending on the bacteria and local resistance patterns. This reduces hospital stays and lowers the risk of side effects.
Side Effects: What to Watch For
All these antibiotics carry risks. But amikacin’s are more predictable - and more dangerous.
- Kidney damage - Seen in 10-25% of patients. Usually reversible if caught early.
- Hearing loss - Can be permanent. More common in older adults, those on long courses, or with existing hearing issues.
- Nerve damage - Tingling, numbness, or muscle weakness. Rare but serious.
- Allergic reactions - Rash, fever, or low blood pressure.
Other antibiotics have different side effect profiles. Ceftriaxone can cause diarrhea or liver enzyme changes. Piperacillin-tazobactam can trigger allergic reactions in penicillin-sensitive people. Meropenem can cause seizures. Colistin? Almost always causes kidney damage.
How Doctors Decide
There’s no single rule. But most hospitals follow a stepwise approach:
- Start with the broadest, safest antibiotic - often ceftriaxone or piperacillin-tazobactam.
- If the infection doesn’t improve in 48 hours, or if culture results show resistant bacteria, switch to amikacin or meropenem.
- If the patient can’t tolerate aminoglycosides, choose meropenem or colistin (if no other options).
- Always confirm the bacteria’s sensitivity through lab testing. Never guess.
Drug sensitivity reports from the lab are the real guide. Amikacin might be listed as ‘sensitive’ even when gentamicin is ‘resistant’. That’s why it’s still in the toolbox.
Cost and Availability
In the UK, amikacin is available through the NHS and is relatively inexpensive - around £10-£15 per dose. Gentamicin is even cheaper. Ceftriaxone and piperacillin-tazobactam cost more - £30-£60 per dose. Meropenem and colistin are the most expensive, often over £100 per dose.
Availability isn’t usually an issue in hospitals. But in smaller clinics or low-resource settings, amikacin may be one of the few options left.
Final Takeaway
Amikacin isn’t the strongest antibiotic. It’s not the safest. But it’s one of the most reliable when others fail. Its value lies in its ability to kill bacteria that have shrugged off gentamicin, tobramycin, or even some cephalosporins.
For most infections, doctors start with safer, broader-spectrum drugs. Amikacin comes in when those don’t work - or when lab tests show the bacteria are resistant to everything else.
It’s a powerful tool. But like any weapon, it’s only as good as the person using it. Proper dosing, monitoring, and timing make the difference between saving a life and causing harm.
Is Mikacin Injection the same as amikacin?
Yes. Mikacin Injection is a brand name for the antibiotic amikacin. The active ingredient is identical. Other brands include Amikin and Kanamycin. Generic amikacin is widely available and works the same way.
Can I take amikacin by mouth?
No. Amikacin is not absorbed through the stomach. It must be given as an injection - either into a muscle or through an IV. Oral amikacin is only used to treat gut infections, like before bowel surgery, and doesn’t enter the bloodstream.
How long does amikacin stay in your system?
Amikacin clears from the blood in about 2 to 3 hours in people with normal kidney function. But it can build up if kidneys aren’t working well. That’s why doctors check blood levels and adjust doses. It’s usually given every 8 to 12 hours during treatment.
Does amikacin cause hearing loss?
Yes. Hearing loss is a known side effect, especially with long-term use or high doses. It’s more common in older adults, newborns, and people with kidney problems. The damage is often permanent. Doctors monitor hearing and kidney function closely during treatment.
Can amikacin be used during pregnancy?
Amikacin crosses the placenta and can affect the baby’s hearing and kidneys. It’s only used in pregnancy if the infection is life-threatening and no safer option exists. Doctors weigh the risk of the infection against the risk of the drug.
What happens if amikacin doesn’t work?
If amikacin fails, doctors look at culture results to see what bacteria are causing the infection. They may switch to meropenem, colistin, or a combination therapy. Sometimes, they’ll test for rare resistance genes. In severe cases, surgery or drainage may be needed along with antibiotics.


Comments
12 Comments
Kenneth Meyer
It’s wild how we treat antibiotics like weapons in a war instead of tools in a toolkit. Amikacin isn’t magic-it’s a sledgehammer. And we keep swinging it because it’s the last thing left in the cabinet when everything else breaks. But the real problem isn’t the drug-it’s the system that lets resistant bugs thrive in the first place. Overuse in agribusiness, poor infection control in hospitals, patients demanding antibiotics for viral infections… we’re breeding monsters and then acting shocked when they survive our best shots.
Lauren Hale
My uncle was on amikacin for 11 days after sepsis. He lost 30% of his kidney function and never recovered his hearing fully. The doctors said it was ‘necessary’-but they didn’t talk about alternatives until after the damage was done. I wish they’d pushed piperacillin-tazobactam harder. It’s pricier, sure, but if you’re going to risk someone’s hearing and kidneys, the trade-off better be worth it. And honestly? Too many docs still treat amikacin like it’s the default. It’s not. It’s a backup plan.
Ankita Sinha
So amikacin is like the last knight standing in a castle under siege? That’s actually kinda poetic. I love how you broke down each alternative like a chessboard-each move has consequences. Ceftriaxone’s the knight, piperacillin’s the rook, meropenem’s the queen… and colistin? That’s the guy who sets the whole castle on fire just to stop the enemy. Brutal. But effective. I’m printing this out for my med school buddy.
Donald Sanchez
lol amikacin? more like amikacin-2.0 the original amikacin was a lil gentler lmao now it’s just a chemical war crime. also why tf is everyone still using gentamicin?? it’s like using a flip phone in 2024. piperacillin-tazobactam all day. also meropenem is the real MVP but only if ur rich or in a fancy hospital 😭
Greg Knight
Let me tell you something-this isn’t just about antibiotics. It’s about how we train doctors. I’ve seen residents grab amikacin like it’s a fire extinguisher for every fire. But the real skill isn’t knowing which drug to use-it’s knowing when *not* to use it. The best clinicians don’t just pick the strongest weapon. They pick the right one for the situation. And that takes time, experience, and humility. Too many of us are trained to fix, not to wait. And that’s dangerous.
rachna jafri
They don’t want you to know this, but amikacin is a Western pharmaceutical scam. In India, we’ve been using herbal combos for centuries-neem, turmeric, garlic extract-those are the real antibiotics. Why do you think our resistance rates are lower? Because we don’t poison our bodies with these toxic chemicals. They push amikacin because it’s profitable. Hospitals profit. Pharma profits. Patients? They get deaf and kidney-dead. Wake up. This isn’t medicine-it’s a corporate extraction model disguised as science.
darnell hunter
While the comparative pharmacological analysis presented is technically accurate, the underlying premise remains fundamentally flawed. The implicit normalization of empirical antibiotic use, even in last-line scenarios, disregards the foundational principles of antimicrobial stewardship. The reliance on culture and sensitivity data is not merely advisable-it is non-negotiable. The omission of local antibiogram integration as a mandatory step constitutes a critical oversight in clinical protocol design.
Hannah Machiorlete
Amikacin gave me tinnitus that never went away. I was 28. They said "it's rare" but it happened to me. Now I can't hear my own kids laugh clearly. And the worst part? No one ever told me that. No consent form, no "this might ruin your life" talk. Just "you need this." I hate that they still use it like it's no big deal. It's not a drug. It's a gamble with your senses.
Bette Rivas
One thing the post doesn’t emphasize enough: the importance of therapeutic drug monitoring. Amikacin’s efficacy and toxicity are both dose-dependent, and peak/trough levels aren’t optional-they’re mandatory. In many hospitals, especially outside academic centers, they skip this because it’s "too expensive" or "too slow." But if you’re going to use a drug with a narrow therapeutic index, you have to measure it. Otherwise, you’re just guessing. And guessing with amikacin is a one-way ticket to nephrotoxicity or deafness. Always check levels. Always.
prasad gali
From a clinical microbiology standpoint, the resistance profile of amikacin is contingent upon the presence of aminoglycoside-modifying enzymes (AMEs), particularly AAC(6')-Ib, which is prevalent in ESBL-producing Enterobacterales. While amikacin retains activity against many gentamicin-resistant strains, its utility is diminishing in carbapenemase-producing organisms where co-expression of AMEs and porin mutations confers cross-resistance. The shift toward carbapenems and newer β-lactam/β-lactamase inhibitors reflects evolutionary pressure, not merely cost or convenience.
Paige Basford
Okay but like… can we just talk about how weird it is that we still use injectables in 2024? Like, why can’t we make a pill version? It’s not like amikacin is a magic molecule that only works in a syringe. We’ve got nanoparticles and liposomes and all this fancy tech-why not make a GI-stable version? I get it’s hard, but we’re still using needles like it’s 1950. Also, why is this so expensive in the US? In Canada, it’s like $5 a dose. We’re getting ripped off.
malik recoba
this is so helpful. i had a friend go through this and no one explained it well. thanks for breaking it down like this. i’ll save this for my mom shes gonna need it.
Write a comment