Aldara Cream (imiquimod) has been a go-to prescription for treating genital warts, actinic keratosis, and some early-stage skin cancers for over two decades. But it’s not the only option anymore-and for many people, it’s not even the best one. Side effects like redness, burning, and flaking can be brutal. Treatment courses can last up to 16 weeks. And if it doesn’t work after a few months, you’re back to square one. So what else is out there? And more importantly, which alternative actually works better for your specific condition?
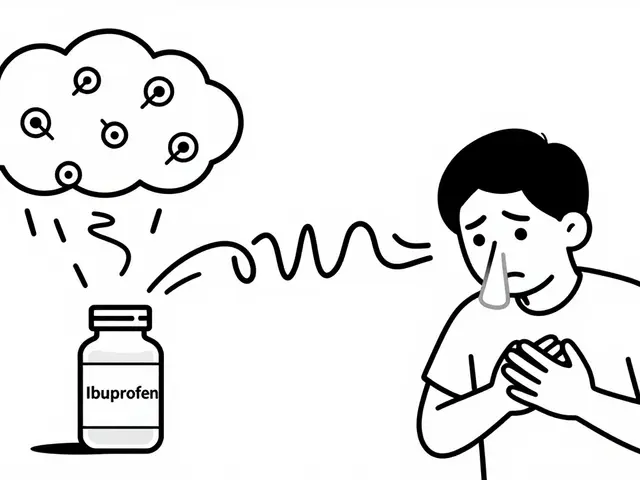
How Aldara Cream Actually Works
Aldara Cream contains imiquimod, a topical immune response modifier. It doesn’t kill the virus or destroy abnormal cells directly. Instead, it tricks your skin into thinking it’s under attack. Your immune system responds by flooding the area with cytokines-tiny signaling molecules that trigger inflammation and activate immune cells to hunt down infected or precancerous tissue.
This mechanism works well for conditions caused by viruses (like HPV) or abnormal cell growth (like actinic keratosis). But because it relies on your body’s response, results vary. Some people clear lesions in 4 weeks. Others need 12 weeks or more. And if your immune system is sluggish-due to age, stress, or medication-it might not respond at all.
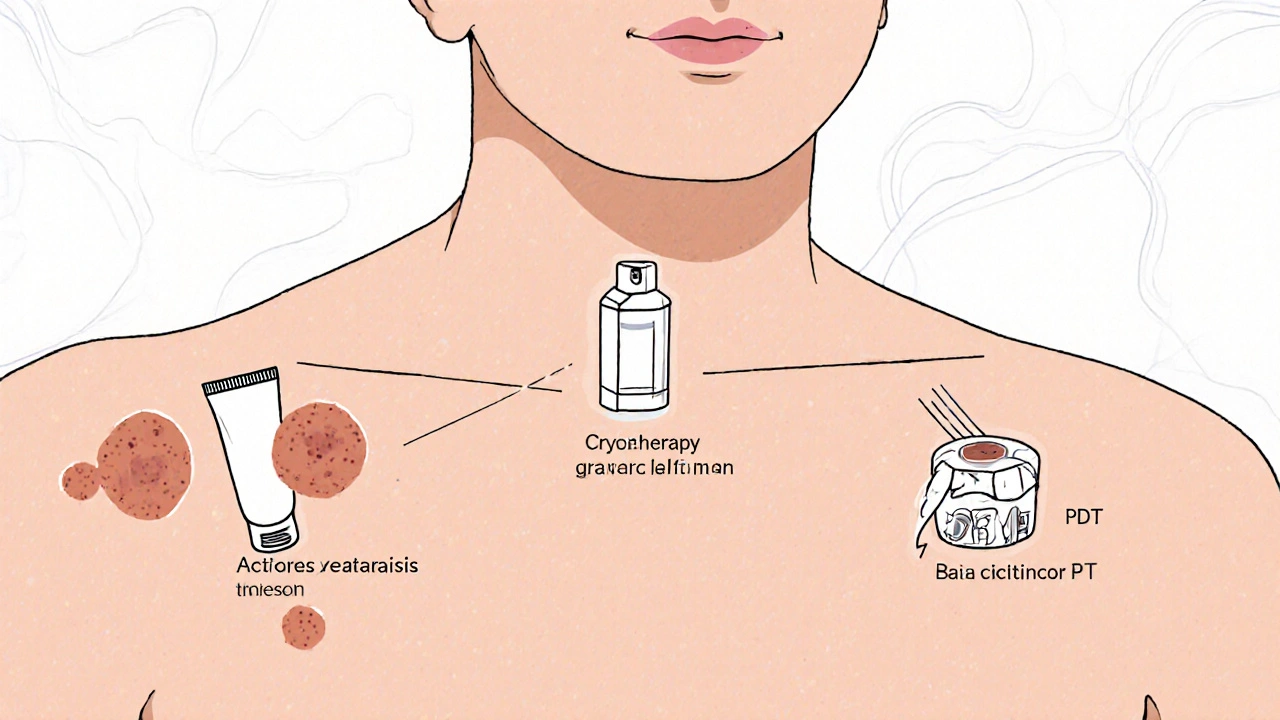
Top Alternatives to Aldara Cream
Here are the most commonly prescribed and clinically proven alternatives, broken down by condition.
For Genital Warts
- Podophyllotoxin (Condyline): A plant-derived compound that stops cell division in warts. Applied twice daily for 3 days, then 4 days off. Repeat for up to 4 cycles. Works faster than Aldara-often clearing warts in 2-4 weeks. Less immune-driven, so fewer systemic side effects. But it’s toxic if ingested and not safe during pregnancy.
- Cryotherapy (liquid nitrogen): Freezes warts off in a doctor’s office. Usually done every 1-2 weeks. Success rate: 70-80% after 3-4 treatments. No daily application needed. Painful during treatment, but recovery is quick. Best for small, isolated warts.
- Trichloroacetic acid (TCA): A chemical that burns off warts. Applied weekly by a clinician. Less messy than Aldara. Works in 4-8 weeks. Can cause scarring if not applied carefully.
- Sinecatechins (Veregen): A green tea extract approved for external genital warts. Applied three times daily for up to 16 weeks. Fewer side effects than Aldara, but slower. Studies show similar clearance rates-around 50% after 16 weeks.
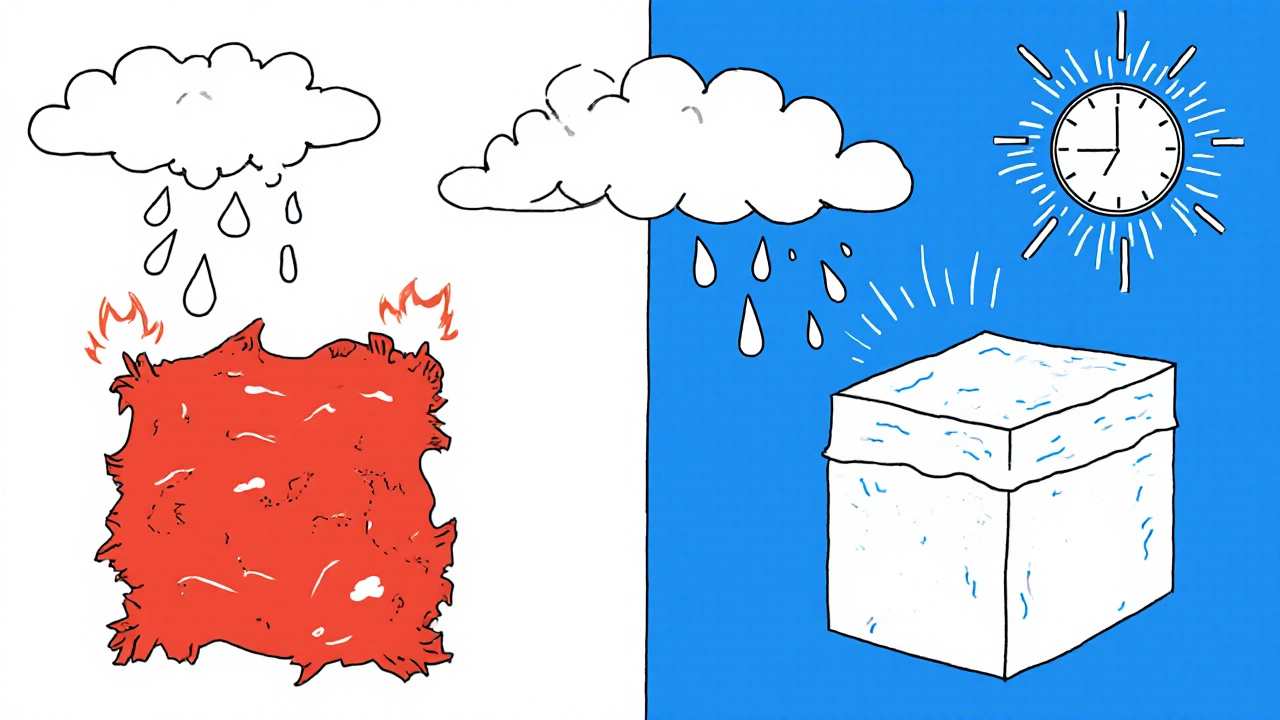
For Actinic Keratosis (Sun Spots)
- Fluorouracil (5-FU) Cream: A chemotherapy drug that kills rapidly dividing cells. Applied once or twice daily for 2-4 weeks. Causes intense redness, crusting, and peeling-often worse than Aldara. But it treats entire areas, not just visible lesions. Clearance rates: 75-90%. Often used for large, diffuse sun damage.
- Diclofenac Sodium Gel (Solaraze): An anti-inflammatory that works slowly over 60-90 days. Mild side effects: slight redness or itching. Best for mild to moderate lesions. Less effective than 5-FU or Aldara, but much gentler.
- Ingenol Mebutate (Picato): A plant extract that causes rapid cell death. Applied for just 2-3 days. Causes severe local reaction, but treatment is short. Clearance rates: 40-50%. Withdrawn in the EU and Canada due to skin cancer risk concerns, but still available in the US under strict monitoring.
- Photodynamic Therapy (PDT): A light-activated treatment. A photosensitizing agent is applied, then exposed to red light after a few hours. One or two sessions. Clears lesions in 80-90% of cases. Minimal downtime. Expensive, but highly effective for large areas.
For Superficial Basal Cell Carcinoma
- Imiquimod (Aldara) is still used here-but only for low-risk, small tumors. Success rates: 70-85%. Requires daily use for 6 weeks. Often paired with surgical confirmation.
- 5-FU Cream: Used off-label. Less reliable than surgery or PDT. Not recommended as first-line.
- Topical Tazarotene: A retinoid. Limited data, but some studies show partial clearance in early lesions. Not FDA-approved for this use.
- Surgical Excision or Mohs Surgery: The gold standard. Removes the tumor with a margin of healthy tissue. Cure rate: 95-99%. No guesswork. Preferred for high-risk or larger tumors.
Side Effects Compared: Aldara vs Alternatives
| Treatment | Common Side Effects | Severity | Duration | Systemic Effects |
|---|---|---|---|---|
| Aldara Cream (Imiquimod) | Redness, swelling, itching, flaking, burning | Moderate to severe | 4-16 weeks | Flu-like symptoms possible |
| Podophyllotoxin | Local irritation, pain | Mild to moderate | 2-4 weeks | None |
| Cryotherapy | Pain during freezing, blistering, pigment changes | Moderate | Days to weeks | None |
| 5-FU Cream | Severe redness, crusting, ulceration | Severe | 2-6 weeks | None |
| Diclofenac Gel | Mild redness, dryness | Mild | 8-12 weeks | None |
| PDT | Burning, swelling, sensitivity to light | Moderate | 24-48 hours | None |
Who Should Avoid Aldara Cream
Aldara isn’t safe for everyone. You should avoid it if:
- You’re pregnant or breastfeeding-imiquimod hasn’t been tested enough in these groups.
- You have an autoimmune disease like lupus or psoriasis-it can trigger flare-ups.
- You’re on immunosuppressants (after an organ transplant, for example)-your immune system won’t respond.
- You have sensitive skin or a history of severe eczema-the irritation can get out of control.
- You’ve tried it before and it didn’t work-repeating it won’t help.
If any of these apply to you, alternatives like cryotherapy, PDT, or TCA are safer and often more effective.
What Works Best for You?
There’s no universal best option. The right treatment depends on your condition, skin type, tolerance for side effects, and lifestyle.
- For small, isolated genital warts: Cryotherapy or podophyllotoxin. Faster, less messy, fewer side effects.
- For widespread sun damage (actinic keratosis): 5-FU or PDT. They treat the whole area, not just visible spots.
- For sensitive skin or low pain tolerance: Diclofenac gel or sinecatechins. Slower, but gentler.
- For early skin cancer: Surgery is still the gold standard. Topical treatments are only for low-risk cases where surgery isn’t possible.
Many patients start with Aldara because it’s well-known. But if you’re not seeing improvement after 8 weeks, it’s time to talk to your doctor about switching. Waiting longer won’t make it work-it just means more irritation and wasted time.
What About Over-the-Counter Options?
Don’t be fooled by OTC wart removers containing salicylic acid. They’re designed for common warts on hands or feet-not genital warts or sun damage. Using them on sensitive areas can cause chemical burns. Prescription treatments are formulated for specific conditions and tested for safety. Skip the drugstore creams for these issues.

When to See a Dermatologist
Don’t self-diagnose. What looks like a wart could be a skin cancer. What looks like a sun spot might be something more serious. Always get a professional evaluation before starting any treatment. A dermatologist can:
- Confirm the diagnosis with dermoscopy or biopsy.
- Recommend the most effective treatment based on your lesion type and location.
- Monitor for recurrence or complications.
- Offer advanced options like PDT or laser therapy if needed.
Even if you’ve used Aldara before, don’t assume it’s still the best choice. Newer options are often better tolerated and just as effective-if not more so.
Final Thoughts
Aldara Cream was revolutionary when it launched. But medicine doesn’t stand still. Today, there are faster, gentler, and more targeted options for almost every condition it treats. The key isn’t just finding a replacement-it’s finding the right replacement for your body, your condition, and your life.
Ask your doctor about alternatives. Bring this list. Ask about success rates, side effects, and how long treatment takes. Don’t settle for a treatment that leaves you in pain for months if something better exists.
Is Aldara Cream still effective for genital warts?
Yes, Aldara Cream can clear genital warts in about 50-60% of cases after 16 weeks. But newer options like cryotherapy or podophyllotoxin work faster-often in 2-4 weeks-with fewer side effects. Aldara is still used, but it’s no longer the first choice for most patients.
Can I use Aldara Cream for acne?
No. Aldara Cream is not approved for acne and won’t help with typical acne breakouts. It’s designed for immune-mediated conditions like warts and sun damage. Using it for acne can cause severe irritation without benefit. Stick to acne treatments like benzoyl peroxide, retinoids, or antibiotics.
How long does it take for Imiquimod to work?
Results vary. For genital warts, you might see changes in 2-4 weeks, but full clearance can take 8-16 weeks. For actinic keratosis, it usually takes 6-12 weeks. If there’s no improvement after 8 weeks, continuing longer won’t help-it’s time to switch treatments.
Is Imiquimod safe during pregnancy?
No. Imiquimod hasn’t been studied enough in pregnant women, and animal studies suggest potential risks. If you’re pregnant or planning to be, avoid Aldara Cream. Cryotherapy or surgical removal are safer alternatives for genital warts during pregnancy.
What’s the most effective treatment for actinic keratosis?
Photodynamic Therapy (PDT) has the highest clearance rate-80-90%-and treats large areas in just one or two sessions. For milder cases, 5-FU cream is very effective but causes more irritation. Diclofenac gel is the gentlest but slowest. The best choice depends on how widespread the damage is and how much irritation you can tolerate.
Can I buy Imiquimod cream without a prescription?
No. Imiquimod is a prescription-only medication in the UK, US, and EU. It’s not available over the counter. Be wary of online sellers claiming to sell it without a prescription-they may be selling counterfeit or unsafe products.
Next Steps
If you’re currently using Aldara Cream and it’s not working-or if the side effects are too much-schedule a follow-up with your dermatologist. Bring a list of your symptoms, how long you’ve been using it, and what you’d like to change. Ask about PDT, cryotherapy, or 5-FU. You don’t have to stick with a treatment that’s not serving you.
For sun damage, prevention matters just as much as treatment. Daily sunscreen (SPF 30+), avoiding midday sun, and annual skin checks can stop new lesions from forming. Topical treatments fix what’s already there-but they don’t stop new ones.

Comments
13 Comments
Ryan Tanner
Just finished my 12th week of Aldara and my skin looks like a battlefield. Tried cryotherapy last week-felt like a tiny ice pick got into my butt cheek, but holy crap, the wart’s gone in 3 days. No more daily cream, no burning, no flaking. Why do doctors even push Aldara first? 🤯
Amina Kmiha
ALDARA IS A BIG PHARMA TRAP. THEY KNOW IT’S SLOW AND PAINFUL-BUT IT MAKES THEM MONEY. THEY DON’T WANT YOU TO KNOW ABOUT PDT BECAUSE IT’S A ONE-TIME DEAL AND INSURANCE WON’T COVER IT IF YOU GO OUT OF NETWORK. THEY WANT YOU STUCK IN A 16-WEEK HELL LOOP WITH A $300 TUBE OF CREAM. 🕵️♀️💸
Rebecca Parkos
OMG YES. I used Aldara for 14 weeks and it barely budged my lesions. Then my dermatologist said ‘try PDT’ and I cried because I thought I was doomed. One session. Two days of looking like a lobster. And now? Zero warts. Zero stress. Stop suffering. Ask for PDT. It’s not magic-it’s medicine.
Jessica Adelle
It is utterly irresponsible to suggest that non-prescription remedies or alternative therapies are viable substitutes for clinically validated pharmaceutical interventions. The integrity of medical science must be preserved. Aldara, despite its drawbacks, has undergone rigorous FDA trials. To casually dismiss it in favor of unregulated or off-label treatments is not only medically unsound-it is ethically indefensible.
Emily Barfield
What is ‘effectiveness,’ really? Is it the absence of a lesion… or the presence of peace? Aldara forces your body to fight-like screaming into a void, hoping the void listens. But PDT? It’s like the sun itself walks in and says, ‘I see you. Let’s fix this.’ No screaming. Just light. Just clarity. And yet-we still cling to the scream, because the silence feels too vulnerable. Are we afraid of healing… or just of trusting it?
Sai Ahmed
Did you know the FDA approved Aldara because a lobbyist from 3M donated to a senator’s daughter’s college fund? I have a friend who works at a clinic in New Jersey. He says 80% of doctors don’t even know about Picato’s withdrawal in Europe. They just keep prescribing it because the reps bring free coffee mugs. 🤫
Albert Schueller
Imiquimod is still the gold standard for low-risk BCCs. The studies are clear. PDT is expensive, cryo is inconsistent, and 5-FU is a chemical warzone. You people are just mad because you don’t want to put in the work. I used Aldara for 10 weeks. My skin was red, yes-but I’m lesion-free. You want fast? Go get surgery. But don’t call it ‘better’ just because it’s easier.
Ted Carr
So let me get this straight. You’re telling me that in 2024, we’re still using a cream that makes your skin look like it survived a lava lamp explosion… to treat a virus that’s been around since the Stone Age? And the alternative is… light? Who wrote this medical textbook? A wizard? 🧙♂️
Bradley Mulliner
People who praise PDT are the same ones who think ‘natural’ means ‘safe.’ Sinecatechins? Green tea extract? That’s what they fed the placebo group in the 2018 trial. It’s not ‘gentler’-it’s statistically inferior. And don’t get me started on TCA. One slip with that acid and you’ve got a scar that lasts longer than your marriage. Stick with the proven. Even if it burns.
Rahul hossain
My cousin in Delhi got treated with neem oil and turmeric paste for genital warts. Two months later, gone. No doctor. No prescription. Just a grandmother’s wisdom and a mortar. We in India don’t need your fancy light machines or $400 creams. Sometimes, the oldest solution is the one that never left the kitchen.
Reginald Maarten
Actually, the clearance rate for Aldara in actinic keratosis is 58% at 16 weeks-not the 70-85% often cited. The 70% figure comes from a 2005 meta-analysis with a small sample size. More recent RCTs (2020, Lancet Dermatology) show 49% efficacy. PDT’s 80-90% is correct, but only if the photosensitizer is applied correctly. Most clinics underdose. So the real efficacy is closer to 65%. Also, ‘surgery’ isn’t a treatment-it’s a procedure. Terminology matters.
Jonathan Debo
Let’s be clear: Aldara is the only treatment that stimulates a systemic immune response. All others are local. That’s why it’s still prescribed for recurrent lesions. You think PDT ‘cures’? It burns the surface. But if your immune system didn’t learn anything? The lesions return. And when they do-where will you be? With your green tea? Your cryo? Your ‘grandmother’s wisdom’? The immune system remembers. Aldara teaches it. The rest? Just arson.
Robin Annison
I’ve used Aldara, PDT, and 5-FU. I don’t think one is ‘better.’ I think they’re different tools. Aldara was my first-painful, slow, but I felt like I was healing from the inside. PDT felt like a reset button. 5-FU felt like punishment. The right one? It’s not about what works fastest. It’s about what you can live with. What you’re willing to endure. And what you’re ready to let go of.
Write a comment