SNRI Medication Comparison Tool
Which SNRI Might Be Right For You?
Select your primary symptoms and concerns to see which SNRIs may be most suitable based on scientific evidence and clinical experience.
Recommended SNRIs for Your Symptoms
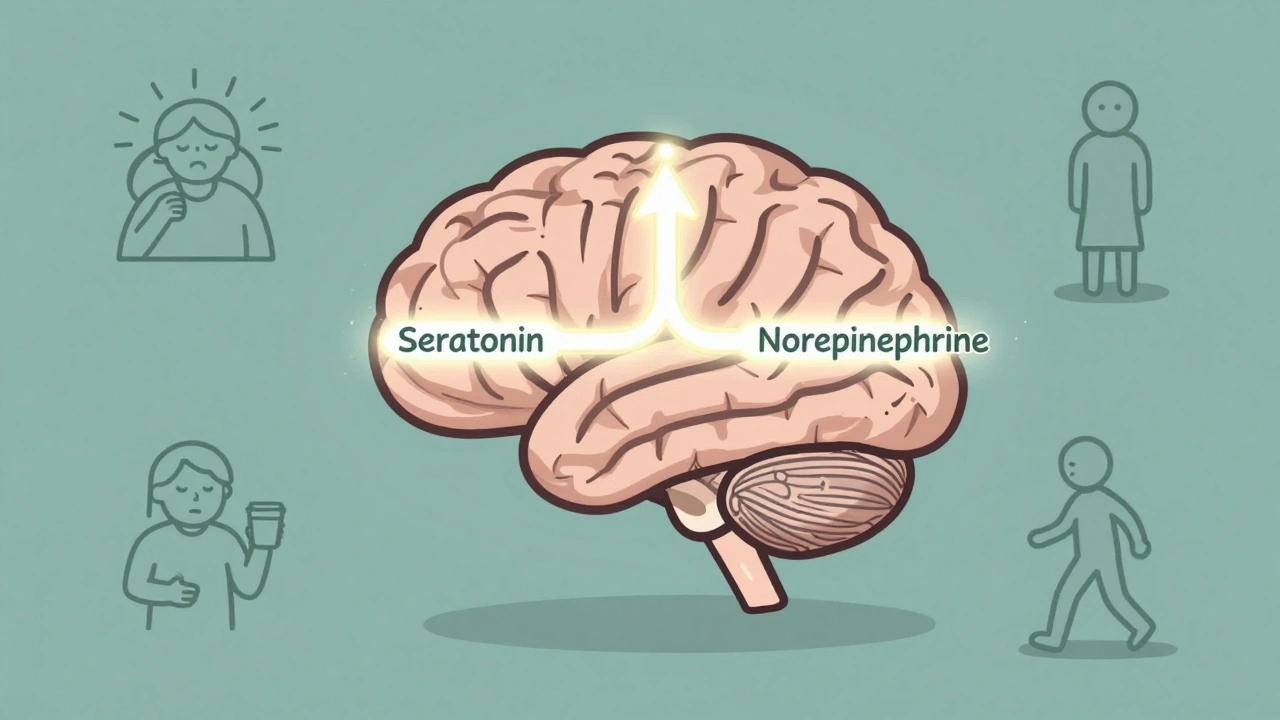
When you’re struggling with depression, anxiety, or chronic pain, finding the right medication can feel like searching for a key in the dark. SNRIs - serotonin-norepinephrine reuptake inhibitors - are one of the most commonly prescribed classes of antidepressants today, and for good reason. Unlike older antidepressants that only target serotonin, SNRIs work on two neurotransmitters at once: serotonin and norepinephrine. This dual action makes them especially useful for people who have both mood symptoms and physical pain, like fibromyalgia or diabetic nerve pain. But they’re not without trade-offs. Side effects range from mild nausea to serious blood pressure spikes and tough withdrawal symptoms. If you’re considering venlafaxine, duloxetine, or another SNRI, it’s important to know what you’re signing up for - not just the benefits, but the real-life downsides too.
How SNRIs Actually Work
SNRIs don’t create new serotonin or norepinephrine. Instead, they stop your brain from reabsorbing these chemicals after they’re released. Think of it like leaving the faucet on but plugging the drain - more of these mood-boosting chemicals stay active in the spaces between your nerve cells. That’s the theory, anyway. Venlafaxine was the first SNRI approved by the FDA in 1993, and since then, others like duloxetine, desvenlafaxine, and levomilnacipran have followed.
Not all SNRIs are created equal. Duloxetine and desvenlafaxine are much stronger at blocking serotonin reuptake than norepinephrine - about 10 times more. Venlafaxine is even more serotonin-focused, with a 30-fold preference. But levomilnacipran and milnacipran tilt the other way, hitting norepinephrine harder. That’s why milnacipran is only approved for fibromyalgia - it’s better suited for pain than pure depression. Some SNRIs, like venlafaxine at higher doses, even nudge dopamine levels up slightly, which might explain why some people feel more energized on them than on SSRIs.
Unlike older tricyclic antidepressants, SNRIs don’t mess with histamine or acetylcholine receptors. That means fewer dry mouth, constipation, or dizziness issues - at least at first. But they still affect platelets, which carry serotonin. That’s why bleeding risks go up, especially if you’re also taking aspirin, ibuprofen, or blood thinners.
Venlafaxine: The Energy Booster With a Catch
Venlafaxine - sold as Effexor or its extended-release version, Effexor XR - is one of the most prescribed SNRIs in the U.S., with over 22 million prescriptions a year. Many people report it gives them a noticeable lift in energy and focus, unlike SSRIs that can sometimes leave them feeling flat or foggy. It’s also approved for generalized anxiety, social anxiety, and panic disorder, making it a go-to for people with overlapping mood and anxiety symptoms.
But venlafaxine has a reputation for being unforgiving. At doses above 150mg a day, about 12-15% of users develop high blood pressure. That’s why doctors often check your BP every few weeks when you’re on higher doses. It’s not rare for someone to feel great for months, then suddenly get headaches or dizziness because their pressure crept up unnoticed.
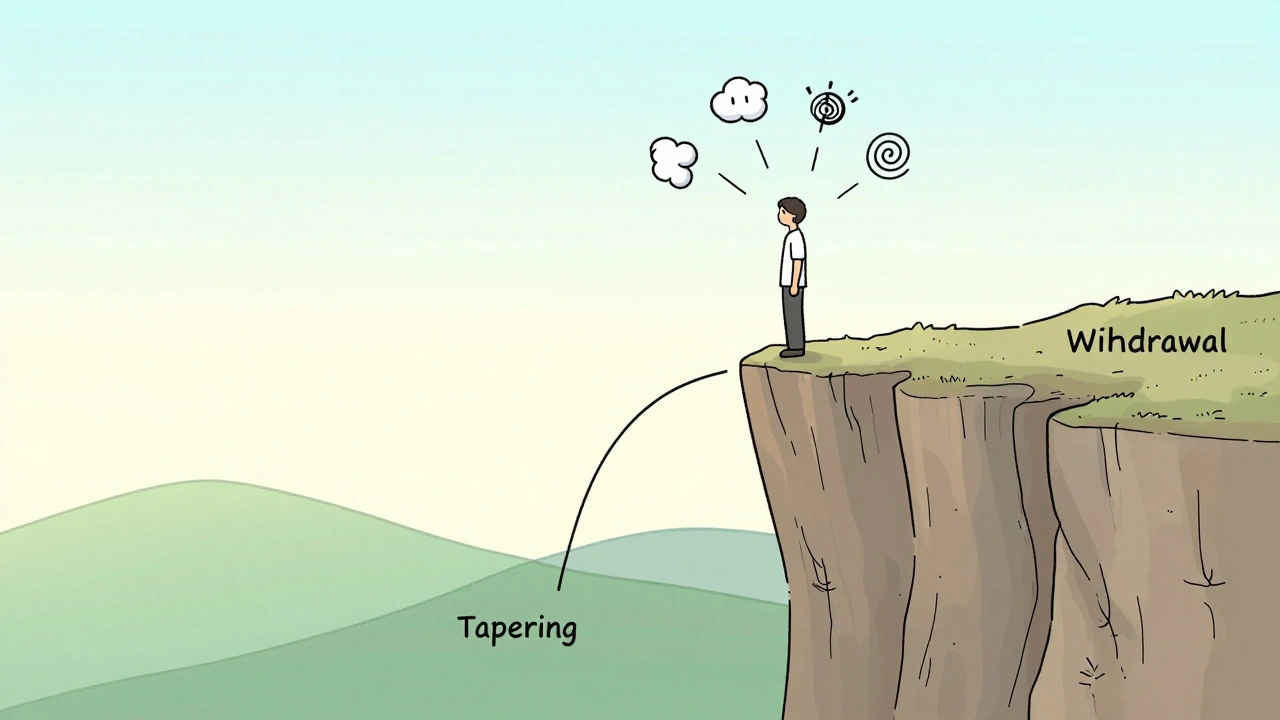
Then there’s the withdrawal. Up to 68% of people who stop venlafaxine abruptly report severe symptoms - brain zaps, dizziness, nausea, insomnia, even flu-like feelings. The term “venlafaxine cliff” is common on patient forums. It’s not just unpleasant; it can make people think their depression is coming back, when it’s really just the drug leaving their system. Tapering slowly - over 2-4 weeks - cuts that risk dramatically. Most doctors now recommend it, and 78% follow the guideline, according to a 2022 JAMA survey.
Duloxetine: The Pain Relief Powerhouse
If you’ve got depression and chronic pain - say, from arthritis, back problems, or diabetic neuropathy - duloxetine (Cymbalta, Drizalma Sprinkle) might be your best bet. It’s one of the few antidepressants FDA-approved for multiple pain conditions. About 45% of users report nausea at first, but for most, it fades after 2-4 weeks. Many also notice a slight weight loss early on - around 5-7 pounds in the first few months - though some gain it back later.
Duloxetine’s strength is its balance. It’s not as strong on norepinephrine as levomilnacipran, but it’s reliable for both mood and physical symptoms. People with fibromyalgia often say it’s the only thing that helps their widespread pain. And unlike some SSRIs, it doesn’t usually cause emotional blunting. But sexual side effects? They’re common. Around 65% of users report low libido, delayed orgasm, or trouble getting aroused. That’s higher than most other antidepressants.
One thing to watch: duloxetine can raise liver enzymes in a small number of people. If you’re on it long-term, your doctor might check your liver function every 6-12 months. It’s not common, but it’s real.
Other SNRIs: What’s Out There?
Desvenlafaxine (Pristiq) is basically the active metabolite of venlafaxine - meaning your body turns venlafaxine into this compound anyway. It’s sold as a once-daily pill, and some people find it easier to tolerate. But studies show it’s not significantly more effective than venlafaxine, and it’s still linked to blood pressure increases.
Levomilnacipran (Fetzima) is the most norepinephrine-heavy SNRI. It’s approved for major depression and sometimes used off-label for fatigue or low motivation. People who feel sluggish on other antidepressants sometimes respond well to it. But because it boosts norepinephrine so strongly, it can raise heart rate and blood pressure more than others. It’s not usually the first pick unless someone’s had bad reactions to other SNRIs.
Milnacipran (Savella) is only approved for fibromyalgia in the U.S. It’s used more for pain than mood, and it’s not commonly prescribed for depression. Still, it’s worth mentioning because it shows how tweaking the serotonin-norepinephrine balance can target specific symptoms.
Side Effects: What to Expect
Most SNRI side effects happen early and fade. But they’re real enough to make people quit before the drug has a chance to work. Here’s what’s common:
- Nausea: 25-30% of users, especially with duloxetine. Taking it with food helps.
- Sexual dysfunction: 20-40% overall, but closer to 65% in user reports. Libido drops, orgasm delays, or complete loss.
- Insomnia or drowsiness: Depends on the person. Some feel wired; others feel sluggish.
- Sweating: About 20% of duloxetine users report increased sweating.
- Dry mouth: Seen in 30% of venlafaxine users.
- Constipation: Around 15% across the class.
Less common but serious:
- Serotonin syndrome: Rare - about 0.5-1 case per 1,000 patient-years - but dangerous. Happens when SNRIs are mixed with other serotonergic drugs like tramadol, triptans, or MAOIs. Symptoms: confusion, rapid heartbeat, high fever, muscle rigidity. Needs emergency care.
- Bleeding risk: SNRIs reduce platelet serotonin, which can make bruising or nosebleeds more likely. Avoid combining with NSAIDs or blood thinners unless monitored.
- Hypertension: Especially with venlafaxine over 150mg/day. Monitor BP regularly.
How SNRIs Compare to Other Antidepressants
SSRIs like fluoxetine or sertraline only block serotonin. They’re great for pure depression and anxiety, but they often fall short for pain. That’s why SNRIs are preferred when pain and mood go hand-in-hand.
Tricyclic antidepressants (TCAs) like amitriptyline also affect both serotonin and norepinephrine - but they hit a bunch of other receptors too. That means more dry mouth, blurred vision, weight gain, and heart rhythm issues. SNRIs are cleaner and safer, especially for older adults.
MAOIs are older, more powerful, and require strict diet rules (no aged cheese, wine, or certain meds). They’re rarely used now unless everything else has failed.
And then there’s tramadol - technically an SNRI, but it’s primarily an opioid painkiller. It’s not approved as an antidepressant, and using it for mood can lead to dependence or seizures. Don’t confuse it with real SNRI antidepressants.
Starting, Adjusting, and Stopping
Doctors don’t start you on the full dose. That’s because side effects hit hardest at the beginning.
- Venlafaxine: Usually starts at 37.5mg/day for a week, then increases to 75mg, then up to 150-225mg if needed.
- Duloxetine: Starts at 30mg/day for a week, then bumps to 60mg for depression. For pain, it can go up to 120mg/day.
- Levomilnacipran: Starts at 20mg, increases to 40mg after a week, then up to 120mg.
It takes 4-6 weeks to feel the full effect. Don’t give up if you feel worse at first. Nausea, jitteriness, or sleep problems often improve after a couple of weeks.
Stopping? Never quit cold turkey. Even if you feel fine, taper slowly over 2-4 weeks. Withdrawal symptoms can mimic a relapse - but they’re not. A 2023 Drugs.com survey found that 54% of venlafaxine users experienced severe withdrawal after missing even one dose.
Who Should Avoid SNRIs?
SNRIs aren’t for everyone. Avoid them if you:
- Have uncontrolled high blood pressure
- Have liver disease (especially with duloxetine)
- Are taking MAOIs or stopped one in the last 14 days
- Have a history of bipolar disorder (SNRIs can trigger mania)
- Are pregnant or breastfeeding (data is limited - talk to your doctor)
- Are under 18 (safety and effectiveness aren’t well-established in teens)
Also, if you’ve had bad reactions to one SNRI, you might not respond well to others. The class is similar, but not identical.
What’s Next for SNRIs?
Research is looking beyond mood. There are 47 active clinical trials studying SNRIs for PTSD, ADHD, and menopausal hot flashes. A new SNRI called LY03015 is in Phase III trials and might offer better balance between serotonin and norepinephrine with fewer side effects.
Also, scientists are exploring whether SNRIs reduce brain inflammation. Microglia - the brain’s immune cells - may calm down with SNRI use, which could explain why some people feel better even before serotonin levels fully adjust. That’s still early science, but it hints that these drugs work in ways we don’t fully understand yet.
The market is growing too. SNRIs made up 32% of new antidepressant prescriptions in 2022, and sales are expected to keep rising as more people live with chronic pain and depression together. Generic venlafaxine now costs $4-8 a month in the U.S., making it one of the most affordable options with broad benefits.
SNRIs aren’t magic. They don’t fix trauma, loneliness, or life stress. But for many, they’re the tool that finally lets them get out of bed, hold a job, or enjoy a meal without pain. The key is knowing what you’re getting into - and working with your doctor to find the right fit.
Can SNRIs cause weight gain?
Some people lose a few pounds in the first few weeks, especially on duloxetine. But over time, many gain weight back - sometimes more than they lost. This isn’t true for everyone, but it’s common enough to be noted in long-term studies. Weight changes are more likely with prolonged use, and they’re not fully understood. If weight becomes a concern, talk to your doctor about adjusting your treatment plan.
Do SNRIs work faster than SSRIs?
Some studies suggest SNRIs may improve energy and motivation faster than SSRIs, especially in people with fatigue or physical pain. But for mood improvement, both classes usually take 4-6 weeks. The difference isn’t huge, but if your main struggle is low energy or chronic pain, SNRIs might feel like they’re working sooner.
Is venlafaxine better than duloxetine?
It depends on your symptoms. Venlafaxine is stronger for anxiety disorders and gives more energy, but it carries a higher risk of blood pressure spikes and harsh withdrawal. Duloxetine is better for pain and tends to be gentler on withdrawal, but it’s more likely to cause nausea and sexual side effects. Neither is “better” overall - it’s about matching the drug to your needs.
Can I drink alcohol while taking SNRIs?
It’s not recommended. Alcohol can worsen dizziness, drowsiness, and liver strain - especially with duloxetine. It can also make depression worse and increase the risk of serotonin syndrome. Even moderate drinking can interfere with how well the medication works. If you drink, talk to your doctor about safe limits.
What happens if I miss a dose?
If you miss one dose, take it as soon as you remember - unless it’s almost time for the next one. Don’t double up. Missing doses of venlafaxine, in particular, can trigger withdrawal symptoms like brain zaps, nausea, or anxiety within hours. That’s why many people use pill organizers or set phone reminders. Consistency matters more with SNRIs than with most other antidepressants.
Are SNRIs addictive?
SNRIs aren’t addictive in the way opioids or benzodiazepines are. You won’t crave them or get high. But your body adapts to them, so stopping suddenly causes withdrawal. That’s not addiction - it’s physical dependence. That’s why tapering is essential. Never stop on your own, even if you feel fine.
Final Thoughts
SNRIs are powerful tools, but they’re not a one-size-fits-all solution. Venlafaxine gives energy but demands careful monitoring. Duloxetine eases pain but can be rough on the stomach. The side effects are real, the withdrawal is serious, and the benefits take time. But for many, they’re the difference between surviving and living. Work with your doctor. Track your symptoms. Don’t rush the process. And remember - if one SNRI doesn’t work, another might. There’s no shame in trying different options until you find the right fit.


Comments
10 Comments
Declan Flynn Fitness
Been on venlafaxine for 3 years now. Nausea was brutal at first, but after 3 weeks, it vanished. The energy boost? Game-changer. I went from barely getting out of bed to running 5Ks. Just monitor your BP-mine crept up at 225mg, so we dropped to 150mg and kept the gains. Tapered off a friend’s leftover dose once by accident-brain zaps for 48 hours. Don’t be that guy.
Nnaemeka Kingsley
u think this is bad? back home in nigeria, we call this 'modern medicine magic' and people just swallow whatever the doctor gives without asking. i had a cousin take duloxetine for depression and he lost 12kg in 2 months then started seeing 'spirits'-doc said it was anxiety. we dont even have liver tests here. just pray and take pills.
Kshitij Shah
So let me get this straight-SNRIs are the ‘I’m too tired to be sad’ pill? Cool. Meanwhile in India, we have ayurvedic gurus selling ‘serotonin laddus’ made from turmeric and hope. At least your drugs come with a 12-page warning label. I’ll take the brain zaps over a guy chanting into my third eye.
Sean McCarthy
68% withdrawal rate? That’s not ‘side effect’-that’s pharmacological sabotage. And you say ‘tapering cuts risk dramatically’? Dramatically? 78% of docs follow the guideline? So 22% don’t? That’s not medical care-that’s Russian roulette with serotonin. And don’t get me started on the ‘weight loss then gain’ trap. It’s a bait-and-switch. You’re not healing-you’re being cycled.
Michelle Smyth
How quaint-the pharmaceutical-industrial complex has finally weaponized neurochemistry into a lifestyle accessory. One must ask: is the ‘energy boost’ merely the illusion of agency, or a pharmacologically induced simulacrum of vitality? The serotonin-norepinephrine binary is a reductive ontological fallacy; the mind is not a chemical ledger, yet we treat it as such. Duloxetine for fibromyalgia? How poetic-we medicate the body’s rebellion against modernity with more modernity. The real tragedy isn’t the withdrawal-it’s that we’ve outsourced our suffering to pill bottles while ignoring the structural rot that made us sick in the first place.
Jaswinder Singh
yo you guys are overcomplicating this. i tried venlafaxine, felt like a robot for 2 weeks, then boom-slept through the night for the first time in 5 years. yeah i had nausea, yeah my dick went MIA for a month, but i’m working again. stop reading Reddit like it’s a textbook. if it works, keep it. if it kills your libido, switch. no one cares about your jargon. just take the damn pill and live.
Matt Dean
Anyone who says SNRIs are ‘safe’ is either a pharma rep or someone who hasn’t experienced the ‘venlafaxine cliff.’ I watched my sister go from functional to suicidal in 72 hours after missing one dose. She thought she was relapsing. She wasn’t. She was detoxing. And her doctor didn’t even warn her. That’s malpractice. If you’re going to prescribe this, you owe people a full 45-minute lecture on withdrawal-not a one-line footnote in the pamphlet.
Patrick Smyth
My sister took duloxetine. She lost 10 pounds. She stopped crying. She started laughing. Then she stopped having sex with me. For 14 months. I asked her if it was me. She said no. It was the drug. I cried. I still cry. I miss her. I miss us. I miss the woman who used to kiss my forehead before bed. Now she’s just… quiet. And I don’t know if it’s the pain, the depression, or the damn pill. But I miss her.
Bee Floyd
Just wanted to say: if you’re reading this and you’re scared to start or stop an SNRI-you’re not alone. I’ve been on three different ones. Each time, I felt like I was betraying my body. But here’s the thing: healing isn’t linear. Some days you’ll feel like a ghost. Other days, you’ll eat ice cream and dance in the kitchen. That’s not the drug-that’s you, coming back. And if you need to switch? Do it. If you need to taper slow? Do it. Your worth isn’t tied to how ‘well’ you tolerate a chemical. You’re already enough, even if you’re still figuring it out.
ANN JACOBS
As a clinical psychologist with over two decades of experience in pharmacological interventions for mood and somatic disorders, I must emphasize that while the empirical data regarding SNRI efficacy and adverse event profiles is robust, the sociocultural framing of these medications within digital forums often devolves into anecdotal sensationalism-thereby obscuring the nuanced, individualized therapeutic calculus that ought to govern clinical decision-making. It is imperative that patients engage in shared decision-making with their prescribers, utilizing validated outcome measures such as the PHQ-9 and GAD-7, rather than relying on algorithmically amplified user testimonials which lack methodological rigor and may induce nocebo effects. Furthermore, the normalization of abrupt discontinuation practices, particularly in the context of venlafaxine, represents a significant public health concern that warrants immediate educational intervention.
Write a comment