When a patient walks into a clinic with five prescriptions, high blood pressure, diabetes, and a $300 monthly drug bill, who’s really in charge of their medication plan? It’s not just the doctor. It’s not just the pharmacist. It’s the whole team working together - and that’s where team-based care changes everything.
What Team-Based Care Really Means for Prescribing
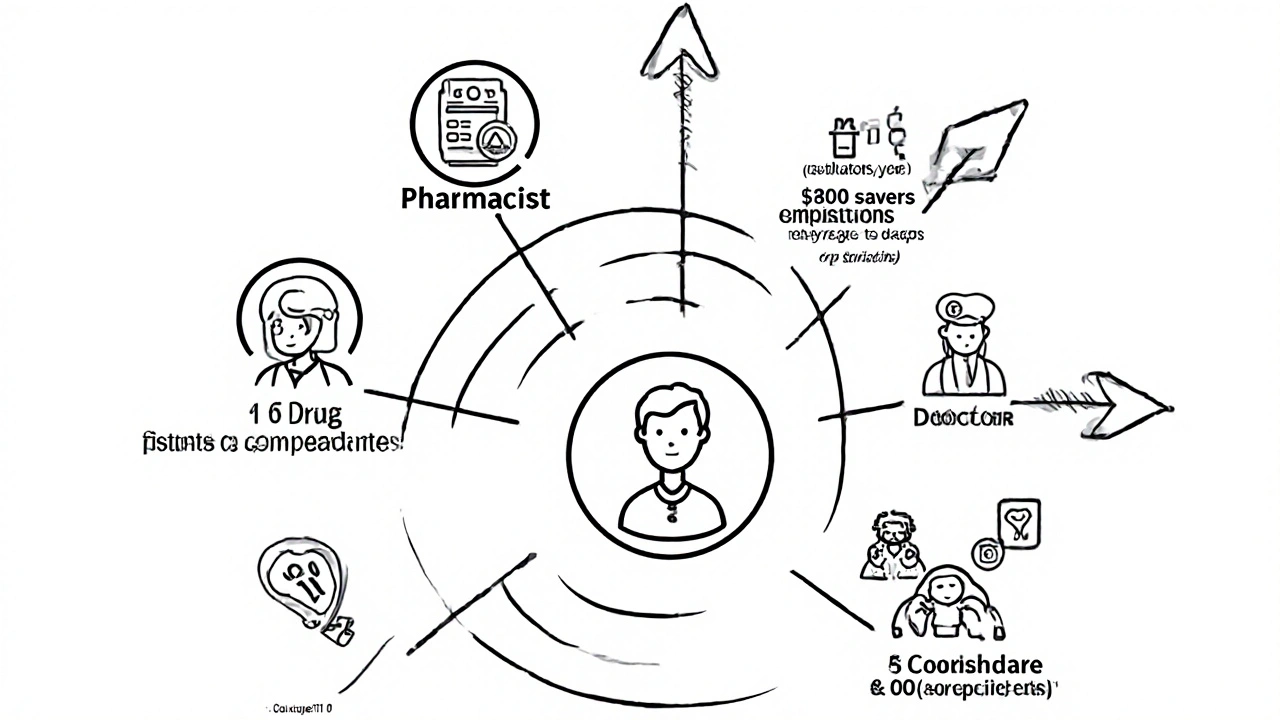
Team-based care isn’t a buzzword. It’s a system where doctors, pharmacists, nurses, and care coordinators share responsibility for a patient’s medication plan. The National Academy of Medicine defined it clearly in 2017: it’s about coordinated, patient-centered care that brings the right people together at the right time. In prescribing, that means moving away from the old model - where one doctor writes a script and hopes the patient fills it - to a structured process where every member has a defined role.Pharmacists don’t just count pills. They’re trained to spot drug interactions, check for therapeutic duplication, and recommend generic alternatives that work just as well but cost a fraction. Nurses track blood pressure trends and remind patients about refills. Care coordinators make sure the specialist’s notes reach the primary care provider. And the doctor? They focus on complex decisions - adjusting insulin doses, diagnosing new conditions - while the team handles the routine but critical stuff.
Why Generic Prescribing Works Better in Teams
Generic drugs are safe, effective, and often 80% cheaper than brand names. But patients don’t always switch - even when it’s the right move. Why? Fear. Confusion. Lack of explanation. In a traditional visit, a doctor might say, “I’m switching you to lisinopril,” and move on. In a team-based model, the pharmacist sits down with the patient and explains: “This is the same medicine as Prinivil, but it costs $12 instead of $120. Here’s how it works. Here’s what to watch for.”Studies show this approach works. One 2023 analysis from PureView Health Center found that team-based medication management led to $1,200-$1,800 in annual savings per patient - mostly from switching to generics and avoiding avoidable hospitalizations. Another study in the National Center for Biotechnology Information (PMC3551433) found that when pharmacists were integrated into care teams, generic substitution rates jumped by 40% without any drop in clinical outcomes.
It’s not just about cost. It’s about adherence. When patients understand why a cheaper pill is just as good, they’re more likely to take it. And when pharmacists document those conversations in the electronic health record, the whole team stays on the same page.
The Roles: Who Does What in a Medication Team
Every effective team has clear roles. Here’s how they break down:- Physicians: Diagnose, manage complex conditions, approve final medication changes, and oversee the team’s recommendations.
- Pharmacists: Conduct comprehensive medication reviews, identify drug interactions, recommend generics, educate patients, and manage Medication Therapy Management (MTM) services.
- Nurses and Medical Assistants: Monitor chronic conditions (blood pressure, glucose, weight), provide adherence counseling, and handle preventive care tasks like flu shots and screenings.
- Care Coordinators: Connect the dots between specialists, pharmacies, and home care. They track referrals, schedule follow-ups, and make sure no one falls through the cracks.
These roles aren’t optional. A 2022 CDC report found that practices using Collaborative Practice Agreements (CPAs) - formal contracts that let pharmacists adjust medications under physician supervision - saw 35% faster medication reconciliation and 22% fewer duplicate tests.
Real Results: Numbers That Matter
Numbers don’t lie. Here’s what team-based care delivers in real-world settings:- 67% reduction in medication errors (American Pharmacists Association, 2022)
- 28% improvement in medication adherence (APhA, 2022)
- 17.3% fewer hospital readmissions (ThoroughCare, 2022)
- 42% more patients switched to generics after pharmacist-led counseling (SICHC case study, 2022)
- $1,200-$1,800 annual savings per patient (PureView Health Center, 2023)
One patient on Healthgrades wrote: “The pharmacist caught three interactions my doctor missed and switched me to generics that saved me $200 monthly.” That’s not luck. That’s a system working.
Challenges: Why It’s Not Everywhere Yet
Despite the benefits, team-based care still isn’t the norm. Why?Cost is a big one. Setting up the infrastructure - hiring pharmacists, training staff, upgrading EHRs - can run $85,000 to $120,000 per practice, according to VA Health Services Research (2021). Smaller clinics can’t afford it alone.
Then there’s culture. Many physicians grew up in a system where they made all the calls. Letting a pharmacist recommend a generic can feel like losing control. But the data shows the opposite: when doctors delegate routine decisions, they have more time for complex cases. One physician on Reddit said his team cut his medication management time by 30% after bringing in a pharmacist.
Technology gaps are another hurdle. If the pharmacist’s notes don’t show up in the doctor’s EHR, or if the care coordinator can’t reach the specialist, the system breaks. A 2022 Commonwealth Fund review found 12% of negative patient experiences came from communication breakdowns between team members.
How to Build a Team-Based Prescribing System
You don’t need a hospital system to start. Here’s a realistic 6-month plan:- Months 1-2: Define roles. Who does what? Draft a simple Collaborative Practice Agreement (CPA) with your local pharmacist. Use CDC templates.
- Months 3-4: Train your team. Pharmacists need 16-24 hours of training on EHR documentation and MTM protocols. Nurses should learn how to flag high-risk patients.
- Month 5: Pick your first 20 patients. Target those with 3+ chronic conditions, 5+ medications, and high drug costs - the exact criteria Medicare Part D uses.
- Month 6: Launch with daily 15-minute huddles. Review each patient’s meds. Track what worked. Fix what didn’t.
Start small. Focus on one condition - say, hypertension. Use generic ACE inhibitors. Track blood pressure trends. Measure savings. Then expand.
The Future: AI, Telepharmacy, and Expanding Access
The field is evolving fast. In 2023, CMS lowered the Medicare Part D eligibility threshold from five to four medications - adding 4.2 million more people to team-based programs. Telepharmacy is booming: 214% growth between 2020 and 2023, according to the American Telemedicine Association. Now, patients in rural towns can get pharmacist-led medication reviews over video.AI is stepping in too. Mayo Clinic’s pilot program used AI to suggest generic alternatives based on patient history and cost data. The result? 22% more appropriate generic switches and 9.3% fewer adverse events.
But the biggest shift isn’t technological. It’s cultural. More healthcare leaders are recognizing that prescribing isn’t a solo act. It’s a team sport. In a 2023 survey by the Advisory Board Company, 92% of executives said they plan to expand team-based medication services.

When It Doesn’t Work
Team-based care isn’t magic. It doesn’t replace the doctor. It doesn’t work well for acute emergencies. If a patient shows up with chest pain, you don’t wait for a team huddle. You act.And there’s risk. Dr. Richard Baron, former CEO of the American Board of Internal Medicine, warned in JAMA that over-reliance on non-physician team members can lead to errors - especially in complex cases. A 2021 study found a 5.2% error rate in medication recommendations from non-physician staff when oversight was weak.
The fix? Clear boundaries. Pharmacists recommend. Doctors approve. Nurses monitor. Everyone documents. Trust is built through consistency, not authority.
What Patients Say
Patient reviews tell the real story. On Healthgrades, practices with team-based medication management average 4.7 out of 5 stars. Comments like:- “I used to skip my meds because they were too expensive. Now I take them every day.”
- “The pharmacist spent 20 minutes with me. My doctor never had time.”
- “I didn’t know I could get the same drug for $15. Thank you for asking.”
These aren’t marketing slogans. They’re proof that when you treat prescribing as a team effort, patients get better outcomes - and feel heard.
Final Thought: It’s Not About Who Prescribes - It’s About Who Cares
The goal isn’t to replace doctors with pharmacists. It’s to make sure no one falls through the cracks. A patient with diabetes shouldn’t need to remember to ask for a cheaper pill. The system should catch it.Team-based care turns generic prescribing from a transaction into a conversation. It turns cost savings into better health. And it turns fragmented care into something that actually works.
Can pharmacists legally prescribe generic medications in team-based care?
Yes, but only under formal Collaborative Practice Agreements (CPAs) that outline their scope of authority. These agreements are signed by both the pharmacist and a supervising physician and are recognized in 49 states. Pharmacists can adjust dosages, switch to generics, or initiate therapy for stable chronic conditions - but they can’t diagnose new diseases or manage complex, unstable cases without physician approval.
What types of patients benefit most from team-based generic prescribing?
Patients with three or more chronic conditions (like diabetes, hypertension, and high cholesterol), taking five or more medications, and spending over $4,000 annually on drugs benefit the most. These are the exact criteria used by Medicare Part D’s Medication Therapy Management (MTM) program. They’re also the patients most likely to experience drug interactions, poor adherence, or financial toxicity - all of which team-based care directly addresses.
Is team-based care more expensive for clinics to run?
Initial setup costs are high - $85,000 to $120,000 per practice - but long-term savings outweigh them. A 2023 analysis found team-based models saved $1,200-$1,800 per patient annually by reducing hospitalizations and unnecessary tests. Many practices recoup their investment within 18 months. Medicare and Medicaid now reimburse for MTM services, and private insurers are following suit.
Do generic drugs work as well as brand names in team-based care?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand name, and to be bioequivalent - meaning they work the same way in the body. Studies consistently show no difference in clinical outcomes. In team-based care, pharmacists educate patients on this equivalence, which increases acceptance and adherence.
How do you know if your practice is ready for team-based prescribing?
Ask these questions: Do you have patients with complex medication regimens? Do you spend too much time on refill requests or drug interactions? Are your staff frustrated by communication gaps? If yes, you’re ready. Start by partnering with a local pharmacist, using CDC’s CPA template, and targeting your top 10 high-cost, high-complexity patients. Track results for 90 days. If adherence improves and costs drop, scale up.




Comments
13 Comments
Robert Merril
Team based care my ass i saw a pharmacist try to switch my blood pressure med last week and he got the generic name wrong twice and my doc had to fix it later
Georgia Green
my clinic just started this and honestly its been a game changer. the pharmacist caught a dangerous interaction between my diabetes med and my new antibiotic. i didnt even know they could do that.
Kathy Grant
its funny how we treat prescribing like its some sacred ritual only doctors can perform when in reality its just applied pharmacology. the real tragedy is that we still let ego dictate who gets to do what instead of letting competence lead. the system isnt broken its just terrified of sharing power.
when a pharmacist spends 20 minutes explaining why lisinopril is the same as prinivil and you finally understand it and feel heard? thats not efficiency thats dignity.
we dont need more doctors we need more people who care enough to listen.
Jennie Zhu
the integration of pharmacists into collaborative practice agreements represents a paradigm shift in pharmaceutical care delivery. evidence from the 2023 PureView Health Center analysis demonstrates statistically significant reductions in medication-related hospitalizations through structured medication therapy management protocols.
furthermore, the implementation of standardized electronic health record documentation protocols ensures continuity of care and mitigates communication fragmentation across interprofessional teams.
this model aligns with the national academy of medicine's 2017 framework for patient-centered, coordinated care delivery systems.
Christina Abellar
my grandma’s meds were a mess until the pharmacist sat down with her. now she takes everything. simple.
Eva Vega
the adoption of collaborative practice agreements (CPAs) under state pharmacy practice acts enables pharmacists to initiate, modify, or discontinue pharmacotherapy for stable chronic conditions, provided physician oversight is maintained per regulatory guidelines.
this operational model enhances therapeutic adherence while reducing polypharmacy risks in high-risk populations.
Margo Utomo
so now the pharmacist is the new doctor? 😏👏 i love it. my meds cost 1/10th now and i actually know what they do. thanks to the person who didn’t rush me out the door 🤗
Noel Molina Mattinez
you think this is new? i been seeing this since 2015 and the docs still act like the pharmacist is just a glorified cashier
the system is rigged to keep doctors in charge even when theyre wrong
they dont want to lose control they just dont want to admit they cant do it all
Roberta Colombin
everyone deserves to understand their medicine. not just the ones who can afford to ask questions.
when someone takes the time to sit down and explain why a $12 pill works just as well as a $120 one, that’s not just saving money. that’s saving dignity.
we should all be able to get care like this.
George Gaitara
team based care is just a fancy way to say theyre cutting doctor salaries and giving the work to underpaid staff
next thing you know nurses will be writing prescriptions and pharmacists will be diagnosing cancer
theyre just trying to make healthcare cheaper not better
Dave Feland
have you considered that this whole team-based model is a stealth government plot to replace physicians with algorithm-driven pharmacists under the guise of cost savings? the FDA’s bioequivalence standards are not legally binding in all jurisdictions, and the 2023 PureView study was funded by a pharmaceutical conglomerate with ties to generic drug manufacturers. this is not progress. this is consolidation.
Ashley Unknown
imagine this: you’re sitting in a clinic, 78 years old, on 8 meds, and the pharmacist pulls up your chart and says ‘i see you’ve been taking this for 12 years and you’ve never once asked why it costs $120’ and then they cry and hug you and you realize your whole life you were just supposed to trust someone who never explained anything and now you’re mad and confused and you dont know if you’re being helped or exploited
what if the real problem is not the system but the fact that we were never taught to ask questions
what if the team is just a bandage on a wound that started when we stopped believing patients could understand
what if the doctor who never had time was the one who should’ve been fired
what if we’re all just waiting for someone to finally say ‘you deserve to know’
and what if that someone was never supposed to be the pharmacist
what if it was always supposed to be the doctor
and what if the doctor was just too tired to care anymore
and what if the system let them be tired
and what if that’s the real tragedy
Matt Wells
the notion that team-based care improves prescribing outcomes is empirically supported by a multitude of peer-reviewed studies, including those published in the Journal of the American Pharmacists Association and the New England Journal of Medicine. however, the implementation of collaborative practice agreements remains inconsistent across jurisdictions due to regulatory fragmentation and institutional inertia. the economic argument for generic substitution is robust, yet the cultural resistance among prescribers-particularly those trained in the paternalistic model of 20th-century medicine-remains a significant barrier to scalability. the future of medication management lies not in technological innovation alone, but in the institutionalization of interprofessional accountability.
Write a comment