Support Group Finder for Diabetic Gastroparesis
Find the right support resources for managing diabetic gastroparesis. Select your location and preferred format to see relevant options.
Choose your location and format to see matching support resources
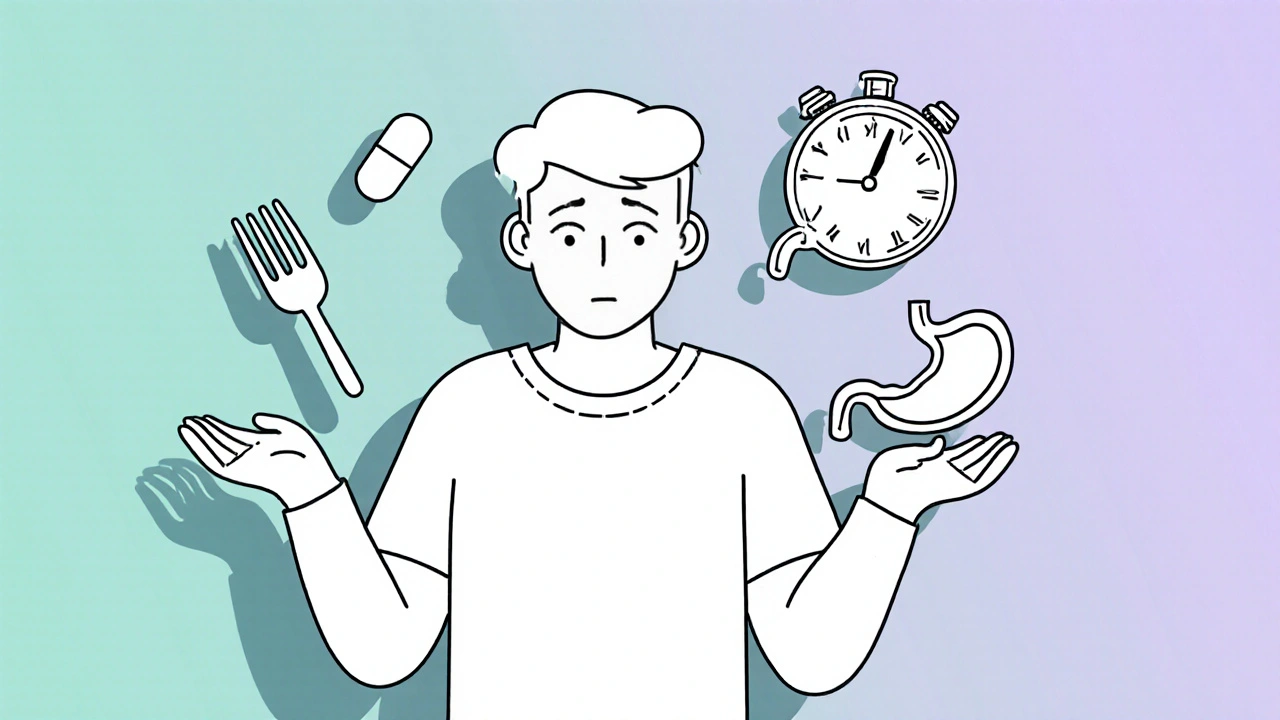
Living with diabetic gastroparesis can feel like a constant juggling act. The stomach’s sluggish movements make meals unpredictable, blood sugars swing wildly, and everyday activities become stressful. While medication and diet are essential, many patients overlook a powerful ally: emotional and peer support. This article explains why joining a support group and seeking counseling can ease symptoms, boost confidence, and help you reclaim a normal routine.
What Is Diabetic Gastroparesis?
Diabetic gastroparesis is a condition where high blood sugar damages the nerves that control stomach muscles, slowing the passage of food into the intestines. Without proper movement, food sits in the stomach longer, causing nausea, bloating, early satiety, and erratic glucose spikes. The condition affects roughly 5% of people with long‑term type 1 diabetes and up to 1% of those with type 2 diabetes, according to the British Diabetes Association.
Why Emotional Health Matters
When you’re constantly guessing how much food you can tolerate, anxiety builds. Stress hormones like cortisol can further slow gastric emptying, creating a vicious cycle. Studies from the American Diabetes Association (2024) show that patients with gastroparesis who report higher stress levels also have poorer glycemic control. In other words, mental strain directly worsens physical symptoms.
Support Groups: The Peer Connection
Support groups are organized gatherings-online or in‑person-where people share experiences, coping strategies, and encouragement. For gastroparesis, groups often include diabetologists, dietitians, and gastroenterologists who answer questions while peers relate to daily struggles.
Key benefits include:
- Validation: Hearing someone else describe the same nausea or “food‑fear” removes the feeling of being alone.
- Practical tips: Members swap recipes that stay light in the stomach yet keep blood sugar stable.
- Motivation: Group challenges-like a 7‑day “small‑meal” plan-create accountability.
- Resource sharing: Access to local specialist directories, clinical trial notices, and affordable medical devices.
Types of Support Groups
Not every group fits every personality. Here are common formats:
- In‑person clinic meetings: Often hosted by a hospital’s gastroenterology department. Example: the Sheffield Diabetes & Gastroparesis Forum runs monthly at Royal Hallamshire Hospital.
- Online forums: Platforms like HealthUnlocked host dedicated threads where you can post anonymously at any hour.
- Social media circles: Closed Facebook groups such as “Gastroparesis Warriors UK” provide daily prompts and live Q&A sessions.
- Hybrid programs: Some charities (e.g., British Diabetes Association) combine quarterly face‑to‑face meet‑ups with a moderated Slack channel.
Counseling: Professional Guidance
Counseling involves a trained therapist helping you process anxiety, depression, or chronic‑illness fatigue. For gastroparesis, the most useful approaches are:
- Cognitive Behavioral Therapy (CBT): Re‑frames catastrophic thoughts about meals, reducing stress‑induced gastric slowdown.
- Mindfulness‑Based Stress Reduction (MBSR): Short daily meditations calm the nervous system, which can improve motility.
- Solution‑Focused Brief Therapy: Sets concrete, short‑term goals-like “eat three small meals per day for two weeks”-and tracks progress.
Therapists with experience in chronic illness, such as clinical psychologists at the University of Bristol’s Health Psychology Unit, understand the medical context and can coordinate with your gastroenterologist.
How Support Groups and Counseling Work Together
Think of them as two sides of the same coin. A support group gives you community and real‑world tricks; counseling equips you with mental tools to apply those tricks consistently. A 2023 pilot study at Manchester Royal Infirmary found that patients who attended both a peer‑led group and weekly CBT sessions showed a 15% reduction in average post‑prandial glucose spikes compared with medication alone.
Finding the Right Group or Counselor
Start with these steps:
- Ask your gastroenterologist or endocrinologist for local referrals.
- Check reputable charities: British Diabetes Association (BDA) lists certified peer‑support programs on its website.
- Search for “diabetic gastroparesis support group UK” on HealthUnlocked or the NHS “Find Services” tool.
- When selecting a counselor, verify credentials: a chartered psychologist with a specialty in chronic disease (e.g., “Health Psychology” registration).
- Arrange a trial session (often free) to gauge comfort level.
Tips for Getting the Most Out of a Group
- Come prepared: Write down one symptom you want advice on before each meeting.
- Set boundaries: It’s okay to skip topics that feel too personal.
- Share successes: Positive stories reinforce group morale and inspire others.
- Be consistent: Regular attendance builds trust and yields better outcomes.
- Combine with self‑monitoring: Use a simple spreadsheet to log meals, symptoms, and mood-then discuss patterns with the group.
Real‑World Example: Emma’s Journey
Emma, a 42‑year‑old teacher from Bristol, was diagnosed with type 1 diabetes at 18 and developed gastroparesis at 35. She tried several pro‑kinetic drugs with limited relief. After joining a local support group hosted by the BDA, she learned about low‑residue meals and paced eating. Simultaneously, she started weekly CBT with a health psychologist. Within three months, Emma reported:
- Less frequent nausea (down from daily to twice a week).
- More stable A1C-dropping from 8.2% to 7.4%.
- Improved confidence in social settings, allowing her to return to staff lunches.
Emma credits the “buddy system” in her group for keeping her accountable, and the CBT techniques for stopping the panic that once triggered gastric slowdown.
Resources You Can Start Using Today
| Resource | Type | How to Access |
|---|---|---|
| British Diabetes Association Peer‑Support Directory | Online list | Visit BDA website, click “Support Groups” |
| HealthUnlocked Gastroparesis Forum | Online community | Create a free account, join the “Gastroparesis” group |
| Local NHS Psychological Therapies (IAPT) Service | Counseling referral | Call your GP and ask for a mental‑health referral |
| Sheffield Gastroparesis Support Meet‑up | In‑person gathering | Check the hospital’s events calendar or call the gastroenterology dept. |
Next Steps: Building Your Support Plan
Take a moment to write down three actions you’ll try this week:
- Contact one of the listed resources and ask about upcoming meetings.
- Schedule an initial counseling session with a health psychologist.
- Start a simple symptom diary-note time of meals, nausea level, mood, and blood glucose.
Even small steps can break the isolation loop and set you on a path toward smoother digestion and steadier sugars.
What triggers gastroparesis symptoms in diabetics?
High blood‑sugar spikes damage the vagus nerve, which controls stomach muscles. Large, high‑fat meals, stress, and certain medications (e.g., opioids) can also slow gastric emptying.
Can a support group replace medical treatment?
No. Peer groups provide emotional and practical help, but they don’t replace medication, diet plans, or specialist care. They work best when combined with standard medical management.
How often should I attend counseling?
Many patients start with weekly 45‑minute sessions for 8‑12 weeks, then move to bi‑weekly or monthly check‑ins based on progress.
Are online support groups safe for privacy?
Choose moderated platforms that require verification (e.g., HealthUnlocked or private Facebook groups). Read the privacy policy and avoid sharing personal identifiers in public posts.
What should I tell my doctor about attending a support group?
Mention the group’s name, meeting frequency, and any new strategies you’re trying. This lets the doctor monitor any diet changes and adjust medications if needed.



Comments
12 Comments
jessie cole
Dear reader, I understand how overwhelming diabetic gastroparesis can feel, and I want to assure you that you are not alone. Joining a supportive community can bring hope and practical tips that fit your day‑to‑day routine. Remember to celebrate even the smallest victories, such as a symptom‑free morning or a steady blood‑sugar reading. Together, we can turn challenges into opportunities for growth.
Kirsten Youtsey
It is quite astonishing that mainstream medical discourse still promotes generic support groups as a panacea, while the elite circles discuss nuanced neuro‑gastroenterology in hushed seminars. One must question whether these gatherings are merely façades engineered by pharmaceutical interests to pacify patients. A discerning individual would seek peer‑to‑peer exchanges that are truly independent, not curated by corporate agendas.
Matthew Hall
Man, the whole thing feels like a secret operation, doesn’t it? They tell us to join a “support group” while they’re probably gathering our data for some hidden agenda. The same folks who push pills also host the chats, and we sit there, spilling our guts, oblivious. It’s like being part of a reality show that nobody told us about, and the script is written in medical jargon.
Vijaypal Yadav
Indeed, the pathophysiology of diabetic gastroparesis involves vagal neuropathy which impairs gastric emptying. Evidence from multiple cohort studies shows that structured peer interaction can improve self‑management metrics. Moreover, integrating cognitive‑behavioral therapy has been associated with a modest reduction in post‑prandial glucose variability. These data underscore the importance of a multidisciplinary approach.
Ron Lanham
The moral responsibility of the medical community extends beyond prescribing pro‑kinetic agents.
It includes fostering environments where patients can share their lived experiences without fear of judgment.
When individuals are isolated, their mental health deteriorates, leading to a cascade of physiological setbacks.
Support groups serve as a collective antidote to that isolation, offering validation and practical wisdom.
Yet, many clinicians dismiss these forums as peripheral, focusing solely on pharmacology.
Such a narrow view neglects the biopsychosocial model that has been championed for decades.
It is ethically indefensible to overlook the proven benefits of peer support in chronic disease management.
Studies have demonstrated that participants in structured groups report lower anxiety scores.
Lower anxiety, in turn, translates to more stable autonomic regulation of the gastrointestinal tract.
Therefore, the argument that support groups are superfluous is grounded in outdated dogma.
Moreover, the integration of counseling, especially cognitive‑behavioral therapy, equips patients with coping strategies that medications cannot provide.
These strategies empower individuals to rehearse healthier eating patterns and stress‑reduction techniques.
When patients internalize these skills, they become active agents in their own recovery.
The medical establishment must therefore endorse and facilitate access to both peer groups and qualified mental‑health professionals.
Failure to do so not only compromises patient outcomes but also betrays the oath to do no harm.
In summary, a holistic treatment plan that weaves together medication, diet, community, and counseling is the only ethically sound pathway forward.
Mahesh Upadhyay
Such moralizing ignores the real struggles of patients.
Rajesh Myadam
I hear the frustration behind the statistics, and I want to acknowledge how brave you are for sharing your journey. It takes courage to confront both the physical symptoms and the emotional weight they carry. Knowing that you are not walking this path alone can make each step feel a little lighter.
Andrew Hernandez
While passion is understandable, it is crucial to respect the scientific evidence that underscores the value of support networks. Dismissing them outright may inadvertently silence voices that could benefit most from communal encouragement.
Alex Pegg
Honestly, I find the hype around support groups overrated; most participants merely exchange anecdotes that rarely translate into measurable health improvements.
laura wood
It’s true that personal stories can feel repetitive, yet they also create a tapestry of shared experience that can be comforting during isolated moments.
Kate McKay
Take this week as a chance to experiment with one new coping tool-perhaps a brief mindfulness pause before each meal or a quick check‑in with a fellow group member. Document how it influences your nausea and blood‑sugar trends, and celebrate any positive shift, no matter how subtle. Consistency, rather than perfection, will drive lasting change.
Demetri Huyler
Oh, sure, “just try a mindfulness pause,” as if the universe would bend for a ten‑minute breather. In reality, many of us are juggling jobs, families, and endless medical appointments, so such breezy advice often feels disconnected from the daily grind.
Write a comment