More than 4 in 10 adults over 65 are taking five or more medications at once. That’s not just common-it’s dangerous. Polypharmacy, the term for taking multiple drugs simultaneously, has become a silent crisis in aging populations. In the UK, the US, and across Europe, older adults are often caught in a web of prescriptions from different doctors, each treating one condition without seeing the whole picture. The result? Confusion, falls, hospital stays, and even early death. But there’s a better way: deprescribing.
What Exactly Is Polypharmacy?
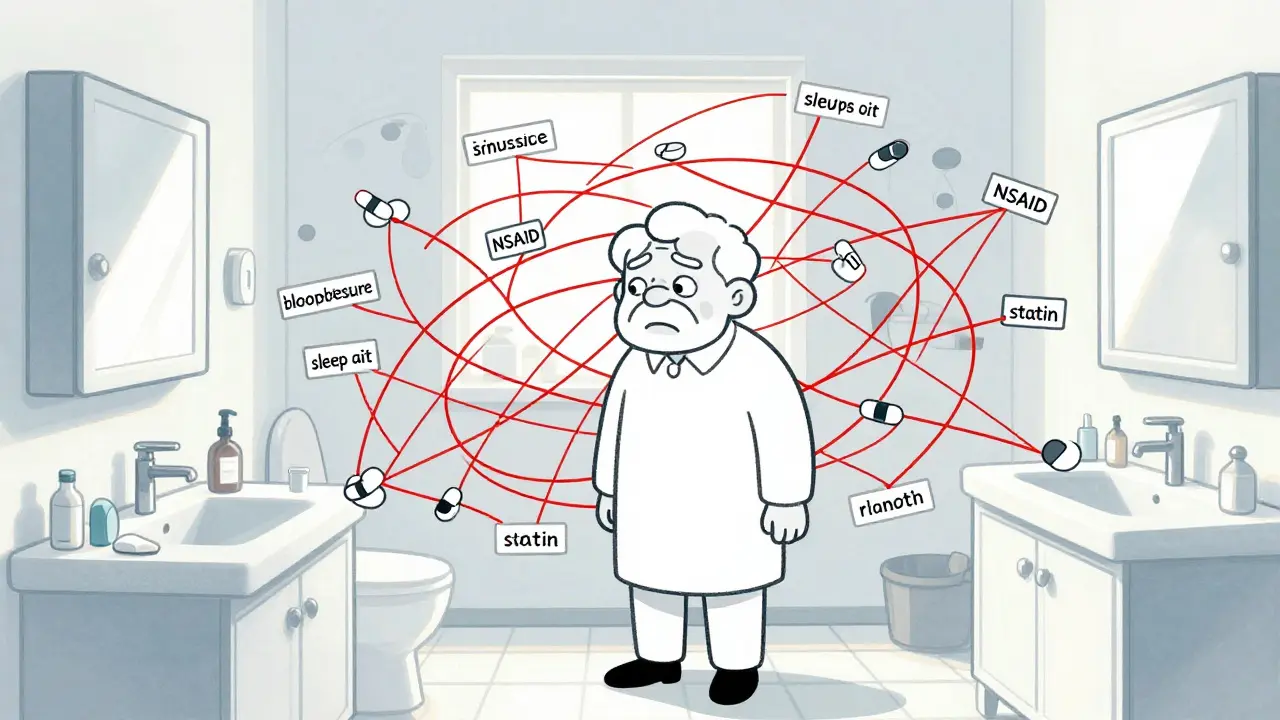
Polypharmacy isn’t just about taking a lot of pills. It’s when someone is on five or more medications at the same time, and those drugs start to clash. It’s not always the doctor’s fault. Many older adults see multiple specialists-a cardiologist for heart issues, a rheumatologist for arthritis, a neurologist for dementia-and each one adds a new prescription. No one is looking at the full list. The numbers are startling. In the US, nearly 65% of older adults visiting a doctor are on five or more drugs. In nursing homes, it’s as high as 80%. Even more worrying: the use of 10 or more medications-called hyper-polypharmacy-has grown by over 4% every year since 2010. And that’s not counting over-the-counter painkillers, herbal supplements, or as-needed meds like sleep aids or laxatives. Those often get left out of the count, but they’re just as risky.Why Do Drug Interactions Happen?
As we age, our bodies change. Kidneys and liver don’t clear drugs as quickly. Muscles shrink, fat increases, and the brain becomes more sensitive to certain chemicals. A drug that was safe at 50 might cause dizziness or confusion at 75. But the real danger comes from combinations. Take a common scenario: an older person takes blood pressure medicine, a statin for cholesterol, an NSAID like ibuprofen for joint pain, a benzodiazepine for anxiety, and a sleeping pill. Each one is fine alone. Together? They can cause a dangerous drop in blood pressure, kidney damage, severe drowsiness, and a much higher risk of falling. Studies show that with just two medications, there’s a 6% chance of an interaction. With five, it jumps to 50%. With seven or more? It’s almost guaranteed. One of the most dangerous patterns is the prescribing cascade. A patient takes a diuretic for high blood pressure and starts feeling dizzy. The doctor prescribes a benzodiazepine for “anxiety.” But the dizziness wasn’t anxiety-it was low blood pressure from the diuretic. Now the patient is on two drugs instead of one, and the root cause is ignored.Who’s Most at Risk?
It’s not just about age. People with multiple chronic conditions are the most vulnerable. Nearly 8 out of 10 adults over 65 have two or more long-term illnesses-like diabetes, heart disease, arthritis, and depression. Each condition brings its own set of drugs. A person with heart failure might be on five medications. Add osteoporosis? Two more. Depression? Another. Sleep problems? One more. Suddenly, they’re on ten pills a day. The risk is even higher for those in care homes or recently discharged from hospital. Studies show that 80% of older adults hospitalized for psychiatric reasons are on five or more medications. Many of these are antipsychotics or sedatives, which increase the risk of stroke, confusion, and death in seniors. And let’s not forget the financial burden. Paying for ten prescriptions a month can cost hundreds of pounds. Many older adults skip doses or split pills to save money-making the problem worse.
What Is Deprescribing-and Why Does It Matter?
Deprescribing isn’t about stopping meds cold turkey. It’s a planned, step-by-step process of reducing or eliminating drugs that are no longer helping-or are doing more harm than good. It’s about asking: “Is this still necessary? Could it be causing more problems than it solves?” The American Geriatrics Society’s Beers Criteria and the STOPP/START guidelines are the gold standards here. They list medications that should be avoided in older adults-like benzodiazepines, anticholinergics, and certain NSAIDs-and highlight drugs that are often missed but should be added, like vitamin D or bone-strengthening agents. Real-world results? When deprescribing is done right, people get better. One study found a 22% drop in falls after reducing sedatives and antipsychotics. Emergency visits went down. Quality of life improved. People felt more alert, less dizzy, and more in control. But here’s the catch: deprescribing is rare. Less than 10% of older adults have a formal medication review. Why? Doctors are rushed. Patients are scared. “I’ve been on this pill for 15 years,” they say. “What if I stop and my pain comes back?”How Deprescribing Actually Works
It’s not a one-time decision. It’s a conversation. Here’s how it works in practice:- Review the full list-including OTC meds, vitamins, and supplements. Many patients don’t tell their doctor about aspirin they take daily or turmeric capsules they bought online.
- Identify red flags-medications on the Beers Criteria list, drugs with no clear purpose, or those prescribed to treat side effects of another drug.
- Prioritize-start with the drugs that have the highest risk and lowest benefit. For example, a proton pump inhibitor (PPI) for heartburn taken for years without a diagnosis is often unnecessary.
- Slow tapering-don’t stop abruptly. For example, antidepressants or blood pressure meds need to be reduced gradually to avoid rebound effects.
- Monitor closely-check in after 2-4 weeks. Watch for changes in mood, energy, sleep, or symptoms. Did the headache go away? Did the dizziness stop?

Barriers to Change
Why isn’t deprescribing happening more often? First, the system isn’t built for it. Doctors get paid for prescribing, not for reviewing. A 10-minute appointment doesn’t leave time to untangle a 12-drug regimen. Second, patients are afraid. They’ve been told these pills are “for their health.” Stopping one feels like giving up. Third, specialists rarely talk to each other. A cardiologist prescribes a beta-blocker. A neurologist adds a dementia drug. Neither knows what the other prescribed. Even the tools we use are outdated. Electronic health records flag dangerous combinations, but they don’t suggest alternatives or help prioritize what to stop. They just say “warning.” That’s not enough.What You Can Do
If you or a loved one is on five or more medications:- Ask your GP or pharmacist: “Is every one of these still needed?”
- Bring a full list-written down, with doses and times-to every appointment.
- Don’t be afraid to ask: “What happens if I stop this?”
- Request a Medication Use Review (MUR) through your pharmacy-it’s free and confidential.
- Track changes: Note if energy improves, dizziness lessens, or sleep gets better after reducing a drug.
The Future of Medication Safety
New tools are emerging. AI systems are being trained to spot high-risk polypharmacy patterns before they cause harm. Pharmacist-led clinics are expanding in the UK and US, offering in-depth medication reviews. Some hospitals now have “deprescribing teams” that work with geriatricians and pharmacists to simplify regimens before discharge. But the biggest change needed? A shift in mindset. Medications aren’t always the answer. Sometimes, movement, better sleep, or social connection can replace a pill. And sometimes, stopping a drug is the most powerful treatment of all. As the population ages, we can’t keep adding pills. We need to start removing them-with care, with science, and with courage.What is considered polypharmacy in older adults?
Polypharmacy is generally defined as taking five or more medications at the same time. This includes prescription drugs, over-the-counter medicines, vitamins, and herbal supplements. While some definitions vary, the five-drug threshold is widely used in clinical guidelines because the risk of harmful interactions rises sharply at this point.
Can stopping medications be dangerous?
Yes, stopping some medications suddenly can be risky-especially antidepressants, blood pressure drugs, or seizure medications. That’s why deprescribing must be done slowly and under professional supervision. The goal isn’t to quit cold turkey, but to reduce or stop drugs in a planned, monitored way to avoid withdrawal or rebound effects.
Which medications are most often unnecessary in older adults?
According to the Beers Criteria, common culprits include benzodiazepines (like diazepam) for sleep or anxiety, long-term proton pump inhibitors (PPIs) for heartburn without diagnosis, anticholinergics (like diphenhydramine in sleep aids), and NSAIDs (like ibuprofen) for chronic pain. These carry higher risks of falls, confusion, kidney damage, and stomach bleeding in older adults.
How can I get a medication review?
In the UK, you can ask your community pharmacy for a free Medication Use Review (MUR). Your GP can also refer you for a comprehensive medication review, especially if you have multiple long-term conditions. Bring your complete list of all medications-prescription and over-the-counter-to the appointment.
Does deprescribing improve quality of life?
Yes. Studies show that when older adults safely reduce unnecessary medications, they often experience fewer falls, less confusion, better sleep, more energy, and improved mobility. Many report feeling more in control of their health. Reducing pill burden can also lower costs and simplify daily routines.





Comments
10 Comments
Nina Stacey
i know this is real because my grandma was on like 12 pills a day and no one ever sat down with her to figure out what was even working
she was dizzy all the time but they just kept adding more for the dizziness
turns out it was the blood pressure med and the sleep aid fighting each other
once they cut the sleep aid she slept better and stopped falling
why do doctors not do this more often
Dominic Suyo
polypharmacy is the medical-industrial complex’s favorite profit center
each pill = a paycheck
each interaction = another ER visit = another revenue stream
they don’t want deprescribing-they want lifelong subscribers
the Beers Criteria? ignored
the STOPP/START guidelines? buried under 37 pages of EHR alerts that say ‘warning’ and do nothing
this isn’t a clinical issue-it’s a corporate disease
Kevin Motta Top
pharmacists can do free med reviews in the UK. why don’t more people know this?
Alisa Silvia Bila
my mom’s on 7 meds and she’s 78
she’s way more alert since they stopped the anticholinergic sleep aid
she didn’t even realize how foggy she was until it was gone
sometimes less really is more
and yes i cried when she said ‘i feel like myself again’
William Liu
the prescribing cascade is terrifying
one doctor sees a symptom and prescribes
another sees the side effect and prescribes more
no one sees the chain
it’s like playing Jenga with someone’s health
Frank Drewery
i’ve seen this in my dad’s care team
cardiologist adds a beta-blocker
neurologist adds a dementia med
primary care forgets to ask what’s been added
no one talks
and the patient is left holding 14 pills and a headache
jessica .
the government is pushing deprescribing because they want to save money not because they care about us
they’re trying to get old people to stop taking their meds so they die faster and the system doesn’t have to pay for their care
its socialism disguised as medicine
Ryan van Leent
people who say 'just stop the meds' are irresponsible
you dont just quit your blood pressure pills
you could die
why are people so reckless with other peoples health
you think its easy to be old and sick
you think its fun to be on 10 pills
no its a nightmare but you dont fix it by taking them all away
Adrienne Dagg
my aunt took her meds for 20 years then finally asked ‘what if i stop this one?’
they took her off the ppi and her acid reflux vanished
she’s been off it for 3 years
no more bloating no more $200/month
she’s alive and happy
and no one told her she could do this 😭
Glen Arreglo
the system is broken but we can still fix it one conversation at a time
ask your doctor: is this still helping?
bring your full list
talk to your pharmacist
track how you feel after changes
you don’t need permission to question your care
you just need to be brave enough to ask
and if your doctor resists? find one who listens
your health is worth it
Write a comment