Telepharmacy Safety Calculator
How Telepharmacy Improves Medication Safety
Based on studies showing telepharmacy's impact on medication safety, this calculator demonstrates the potential benefits when using telepharmacy services compared to traditional pharmacies.
- Traditional pharmacy error rate: 0.7% (99.3% accuracy)
- Telepharmacy error rate: 0.2% (99.8% accuracy)
- 12.9% increase in hospitalizations without telepharmacy
- 11.1% reduction in pharmacy deserts with telepharmacy
For every 10,000 prescriptions filled through telepharmacy instead of traditional pharmacies:
- 50 fewer errors
+ 4.5 fewer hospitalizations
Medication Safety Calculator
Results
Enter the number of prescriptions to see potential safety benefits.
| Metric | Traditional Pharmacy | Telepharmacy | Difference |
|---|---|---|---|
| Estimated Errors | |||
| Hospitalization Risk |
Safety Benefits
When you live in a rural town with no nearby pharmacy, getting your prescriptions on time isn’t just inconvenient-it can be dangerous. Missing a dose of blood pressure medication or not catching a dangerous drug interaction could land you in the hospital. That’s where telepharmacy comes in. Instead of driving hours to a pharmacy, you video chat with a licensed pharmacist who reviews your meds, answers your questions, and even dispenses your pills-all from a remote location. But does it work? Is it safe? And what do real studies actually say?
What Telepharmacy Actually Does
Telepharmacy isn’t just a video call with a pharmacist. It’s a full pharmacy service delivered over secure technology. A central pharmacy, often called a hub, supports multiple remote sites-like small clinics, rural hospitals, or even mobile units. Pharmacists log in remotely, verify prescriptions, counsel patients, and supervise automated dispensing machines. In some cases, patients get their meds delivered or pick them up at a kiosk. The system uses high-definition video, encrypted electronic health records, and automated checks to catch errors before they happen. It’s not new. North Dakota passed the first telepharmacy law in 2001. But it exploded after 2020. When the pandemic shut down in-person visits, states rushed to legalize remote pharmacy services. By 2022, 28 states had updated their rules to allow it. Today, telepharmacy operates in 42% of areas officially labeled as “health professional shortage zones”-places where doctors and pharmacists are in short supply.Is Telepharmacy as Safe as a Regular Pharmacy?
This is the big question. If you’re getting your meds from a screen instead of a person behind a counter, are you at higher risk? The answer, based on multiple studies, is surprisingly reassuring. A major 2021 review of six studies found that telepharmacy matched traditional pharmacies in accuracy. Both achieved error rates between 0.1% and 0.7%. That’s better than most industries. One study even showed telepharmacy sites had slightly fewer dispensing errors-99.8% accuracy versus 99.3% in brick-and-mortar stores. How? Remote pharmacists often use double-check systems. One pharmacist reviews the prescription, another verifies the dispensed pills. Automated alerts flag potential interactions or wrong dosages. A 2023 study in JAMA Network Open tracked over 3,700 patients. Those using telepharmacy had a 12.9% increase in hospitalizations over a year. The group without telepharmacy access? A 40.2% increase. That’s not a coincidence. When people can’t get their meds on time or get confused about how to take them, things go wrong. Telepharmacy helped prevent that.Where Telepharmacy Outperforms Traditional Pharmacies
The real win isn’t just matching safety-it’s expanding access where it’s needed most. Before telepharmacy, over 10 million Americans lived in “pharmacy deserts”-areas with no nearby pharmacy within 10 miles. In states that passed supportive laws, that number dropped by 11.1% in just one year. That’s over a million people gaining access to a pharmacist for the first time. In rural clinics, telepharmacy cut the time to approve after-hours prescriptions from hours to under 20 minutes. For someone with a sudden infection or a child with a fever, that matters. A pharmacist in South Dakota reported catching about 1.2 errors per 100 prescriptions-same as urban pharmacies. But in places with no pharmacist at all, that number was zero. The Indian Health Service’s telepharmacy program for Navajo Nation communities cut their medication error rate to 0.45%, below the national average of 0.67%. Their secret? Dual verification for high-risk drugs like insulin and blood thinners, plus a rule: if a case is too complex, it’s immediately sent to an in-person pharmacist.
The Hidden Risks and Where Telepharmacy Falls Short
But it’s not perfect. One big concern: poor video quality. A Reddit user in North Dakota shared how a bad connection caused a technician to miss her insulin allergy. She had an adverse reaction. That’s not theoretical-it happened. A 2022 survey found nearly 30% of telepharmacy users worried pharmacists couldn’t fully assess their condition remotely. No one can see if you’re sweating, shaking, or too weak to stand. A pharmacist can’t spot signs of addiction or confusion just from a screen. Dr. Jerry Fahrni, writing in the Journal of the American Pharmacists Association, warned that “the absence of physical presence may limit the pharmacist’s ability to detect non-verbal cues.” Training gaps also exist. Pharmacy students in one study performed consultations 15-20% less effectively via telepharmacy than in person. That’s not because they’re bad-it’s because they’re not trained for it. The American Society of Health-System Pharmacists now recommends 16-24 hours of specialized training for telepharmacy pharmacists. Sites with that training saw 22% fewer errors. And then there’s tech. In 35% of telepharmacy sites, internet connectivity is unreliable. If the video drops during a critical consultation, what happens? Not all systems have backup protocols.What’s Changing Now? The Future of Telepharmacy Safety
The field is evolving fast. In September 2022, the Patient-Centered Outcomes Research Institute gave $3.2 million to run the first large-scale randomized trial comparing telepharmacy and traditional pharmacy safety across 12 rural communities. Results are expected in 2025. The FDA launched a national monitoring project in January 2023 to track adverse drug events tied to telepharmacy. Medicare now reimburses for telepharmacy services under Part D, which means more patients can use it-and more data will be collected. New AI tools are being tested. MedsAI, a company that raised $22 million in 2023, built software that predicts medication errors before they happen. In early trials, it improved adverse event detection by 18.7%. Imagine a system that flags a dangerous combo of blood pressure and kidney meds before the pharmacist even opens the file. The American Pharmacists Association aims to set national safety standards for telepharmacy by 2025. That’s huge. Right now, rules vary wildly by state. Some require 720p video. Others demand redundant internet lines. Standardization will make safety consistent.
Who Benefits Most? And Who’s Left Behind?
The clearest winners? Rural patients, seniors with mobility issues, and people without reliable transportation. One user in rural Montana said telepharmacy had likely prevented two ER visits by helping her manage her warfarin dose. But not everyone benefits equally. If you live in an area with slow or no broadband, telepharmacy won’t work. That’s still true in parts of Appalachia, the Deep South, and Native American reservations. Until internet access improves, telepharmacy won’t fix all access gaps. Also, complex cases still need in-person care. A patient with multiple chronic conditions, new side effects, or mental health concerns might need more than a video call. Telepharmacy works best as a supplement-not a replacement-for full pharmacy services.Bottom Line: Safe? Yes. Perfect? No.
Studies show telepharmacy is as safe as traditional pharmacies-and often safer for people who otherwise wouldn’t get care. It reduces medication errors, cuts wait times, and brings pharmacists to places they’ve never been. But safety depends on good tech, solid training, and reliable internet. Poor connections, untrained staff, or lack of backup plans can create new risks. The evidence says this: if you’re in a rural area with no pharmacy, telepharmacy is likely your best-and maybe only-chance to get safe, consistent medication care. For everyone else, it’s a useful tool that’s here to stay.Is telepharmacy legal in all states?
No. As of early 2026, 28 states have specific laws allowing telepharmacy, while 22 states still lack clear regulations. Some states require video quality standards, dual verification for high-risk drugs, or special pharmacist licenses. Always check your state’s pharmacy board rules before using a telepharmacy service.
Can telepharmacy handle all types of medications?
Most routine prescriptions-antibiotics, blood pressure meds, diabetes drugs-are handled just fine. But high-risk medications like chemotherapy, injectables, or controlled substances often require extra steps. Many telepharmacy programs require dual verification or transfer these cases to in-person pharmacists. Complex cases, especially those involving mental health or multiple drug interactions, are usually referred to a physical pharmacy.
Do I need special equipment to use telepharmacy?
You need a device with a camera and internet-like a smartphone, tablet, or computer. Most services use secure, HIPAA-compliant apps, so no downloads are needed. A stable connection is critical. If your internet drops frequently, you might face delays or safety risks. Some rural clinics provide kiosks with built-in video systems for patients without reliable home tech.
Is telepharmacy covered by insurance?
Yes, under Medicare Part D since late 2022. Many private insurers now cover telepharmacy consultations and dispensing services, especially in rural or underserved areas. Always confirm coverage with your plan before scheduling. Some programs offer free or low-cost services through federal grants or nonprofit partnerships.
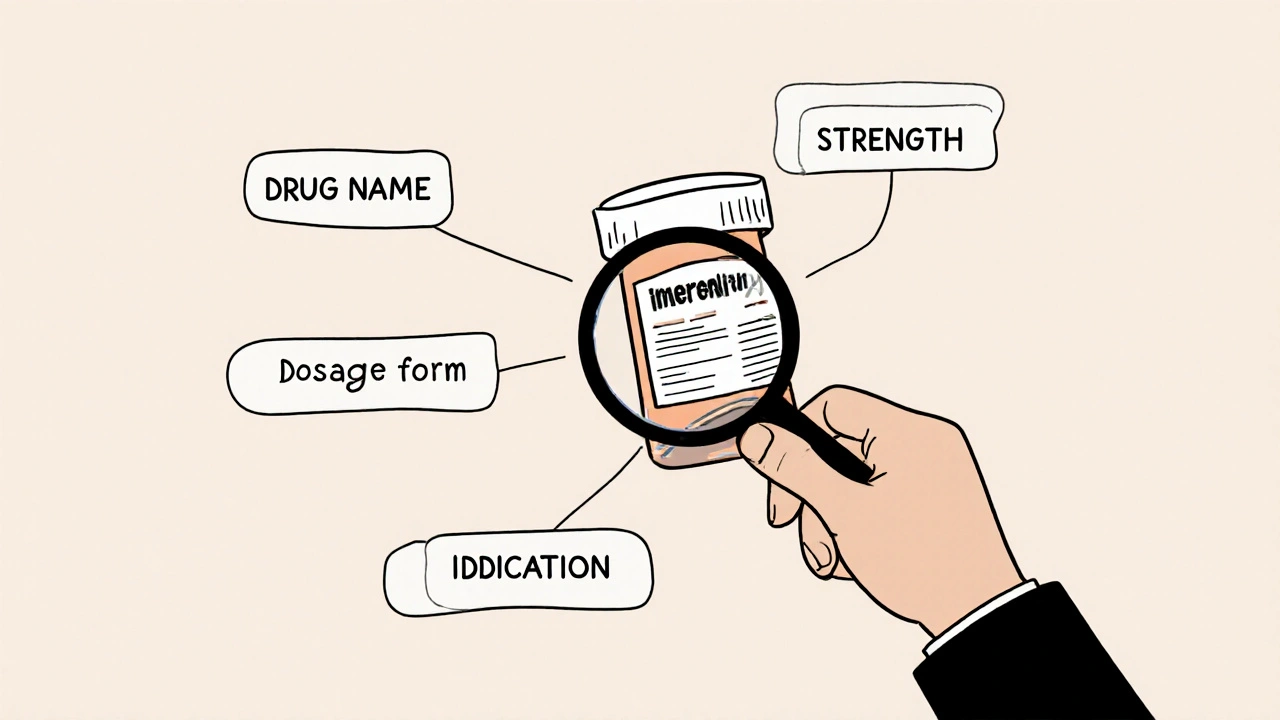
How do I know if a telepharmacy is legitimate?
Look for licensed pharmacists on staff and verify the service is connected to a state-licensed pharmacy. Legitimate providers will show you their pharmacy license number and be registered with your state’s board of pharmacy. Avoid services that don’t require a prescription, offer drugs without consultation, or use unsecured video platforms. If it feels too easy or too cheap, it’s probably not safe.


Comments
8 Comments
Ambrose Curtis
Man, I’ve been using telepharmacy in rural Montana for two years now. My grandma’s warfarin levels? Perfect. No more driving 90 minutes to the nearest pharmacy in the snow. The tech ain’t perfect-once the video froze mid-counseling-but the pharmacist called me back within five minutes. That’s better than some brick-and-mortar places I’ve been to.
And yeah, I know some folks worry about missing body language, but let’s be real-if you’re too weak to stand, you’re probably already in trouble. At least this way you get meds before you collapse.
James Dwyer
Studies show telepharmacy is just as safe as traditional pharmacies. That’s not even close to controversial anymore. The real issue is infrastructure, not the model.
jonathan soba
Let’s not pretend this is some miracle solution. You’re replacing human judgment with a screen and an algorithm. The 0.1% error rate? That’s still 1000 errors per million prescriptions. And when it’s your mom’s insulin dose that’s wrong, you don’t care about the stats. This is a Band-Aid on a severed artery.
Jess Bevis
Telepharmacy saved my dad’s life. No more missed doses. No more driving in the dark. Simple as that.
Rose Palmer
While the data supporting telepharmacy’s safety profile is compelling, it is imperative to acknowledge that regulatory fragmentation across state lines presents a significant systemic vulnerability. Standardization of technical protocols, mandatory continuing education for remote pharmacists, and mandatory redundancy in connectivity infrastructure are non-negotiable prerequisites for equitable and safe deployment.
Howard Esakov
Oh wow, another ‘telepharmacy saves lives’ think piece. Did you even read the JAMA study? The 12.9% hospitalization rate? That’s still higher than urban pharmacies. And now we’re giving Medicare dollars to tech startups instead of fixing the actual healthcare system? Classic. 😒
Mindee Coulter
I work in a rural clinic and we’ve had telepharmacy for a year. The kiosk is a game changer. Patients who never came in before are now getting their meds. One guy came in crying because he hadn’t filled his diabetes script in three months. He said he didn’t have a car. Now he gets it every week. No drama. Just help.
Yeah, the internet drops sometimes. But we’ve got a landline backup and a printed checklist. It’s not perfect. But it’s better than nothing.
Rhiannon Bosse
So let me get this straight-big pharma and tech bros are pushing this because they can’t hire real pharmacists? And now we’re supposed to trust a screen with our insulin? What’s next? AI prescribing from a chatbot? 😂
Remember when they said self-checkout was ‘convenient’? Now grocery stores are full of people staring at screens for 20 minutes trying to scan a banana. Telepharmacy is just the next step in the great dehumanization of healthcare. And don’t even get me started on the data mining.
They’re not saving lives. They’re saving money. And we’re the guinea pigs.
Write a comment