Every year, hundreds of thousands of people in the U.S. take the wrong medication or the wrong dose because of a simple mistake on a pharmacy label. It’s not rare. It’s not just something that happens to other people. It happens to someone you know - maybe even you. And the scary part? Most of these errors are preventable - if you know what to look for.
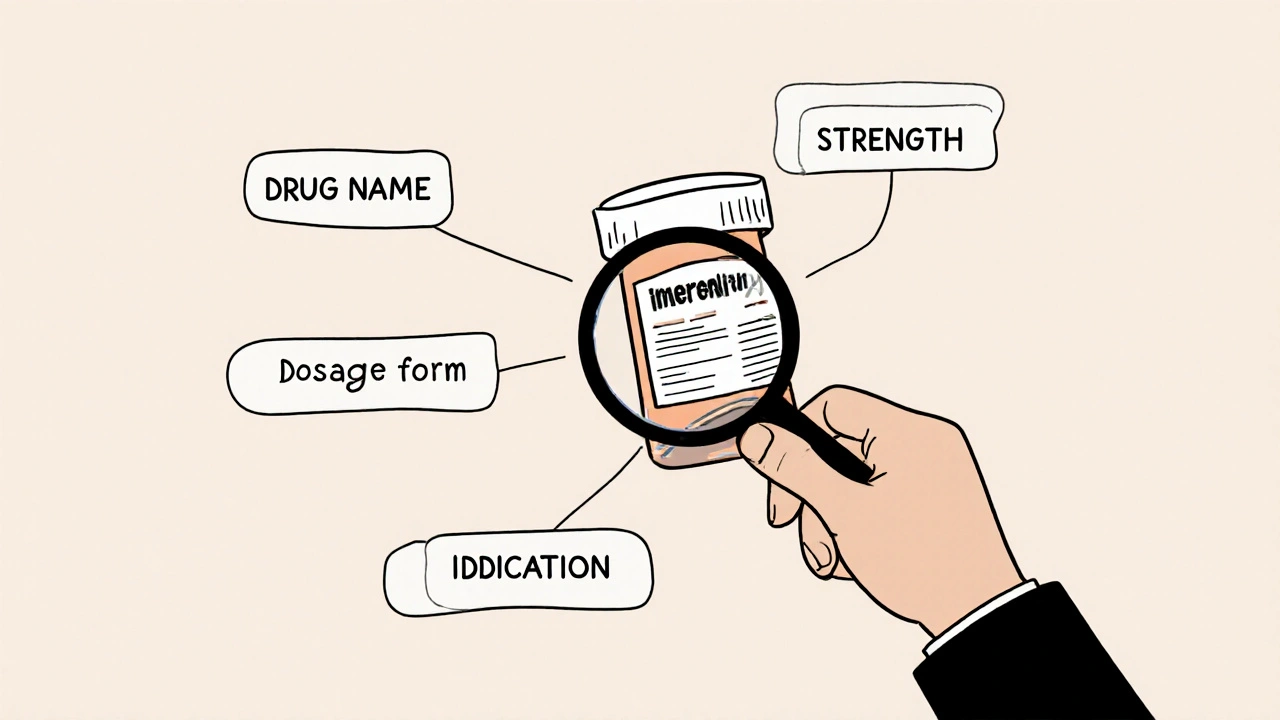
What a pharmacy label should tell you
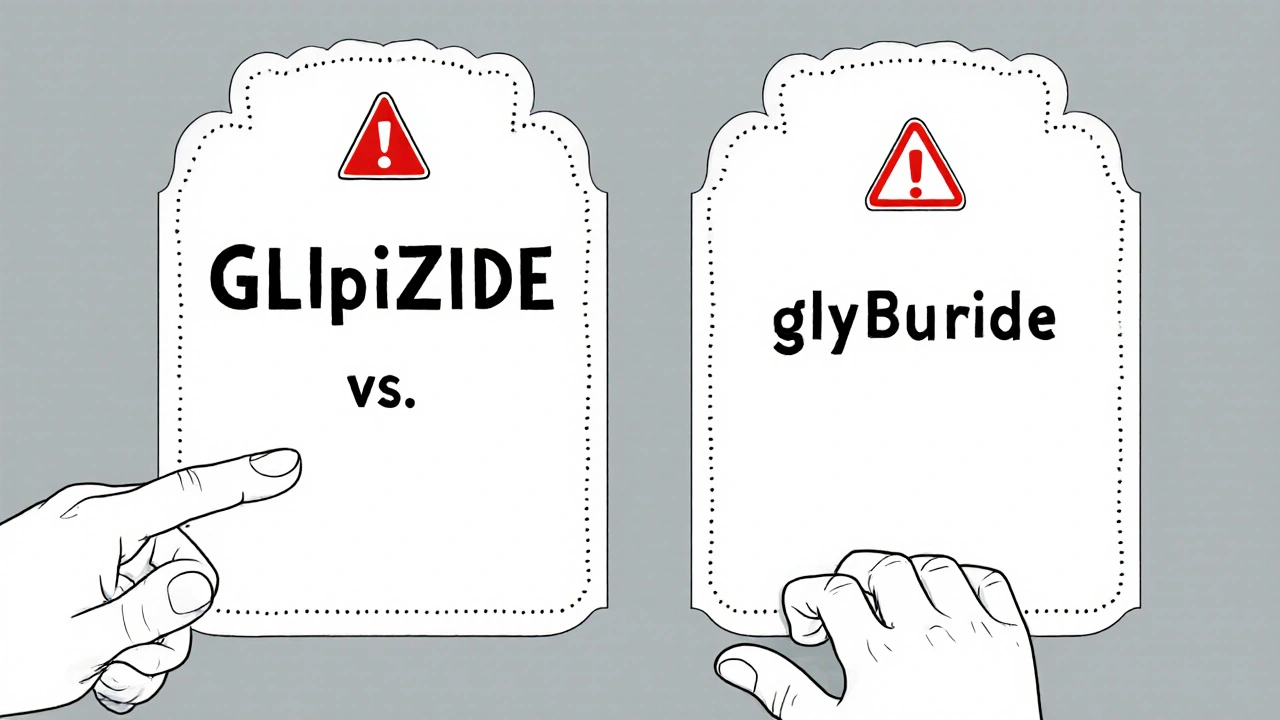
Your prescription label isn’t just a piece of paper with your name on it. It’s your last line of defense. Before you swallow that pill, the label should clearly show five things: the drug name (both brand and generic), the strength (how much is in each pill or dose), the dosage form (tablet, capsule, liquid), the directions (how often and how to take it), and the indication (why you’re taking it - like "for high blood pressure" or "for diabetes").Here’s the problem: many labels leave out the indication. Only about 18% of community pharmacy labels include it, even though adding it cuts wrong-medication errors by 63%. Without knowing why you’re taking a drug, you won’t realize you’ve been given the wrong one. Glipizide and glyburide? They both treat diabetes, but they’re not the same. One can cause dangerous low blood sugar if you meant to take the other. If the label doesn’t say "for type 2 diabetes," you might never catch the mix-up.
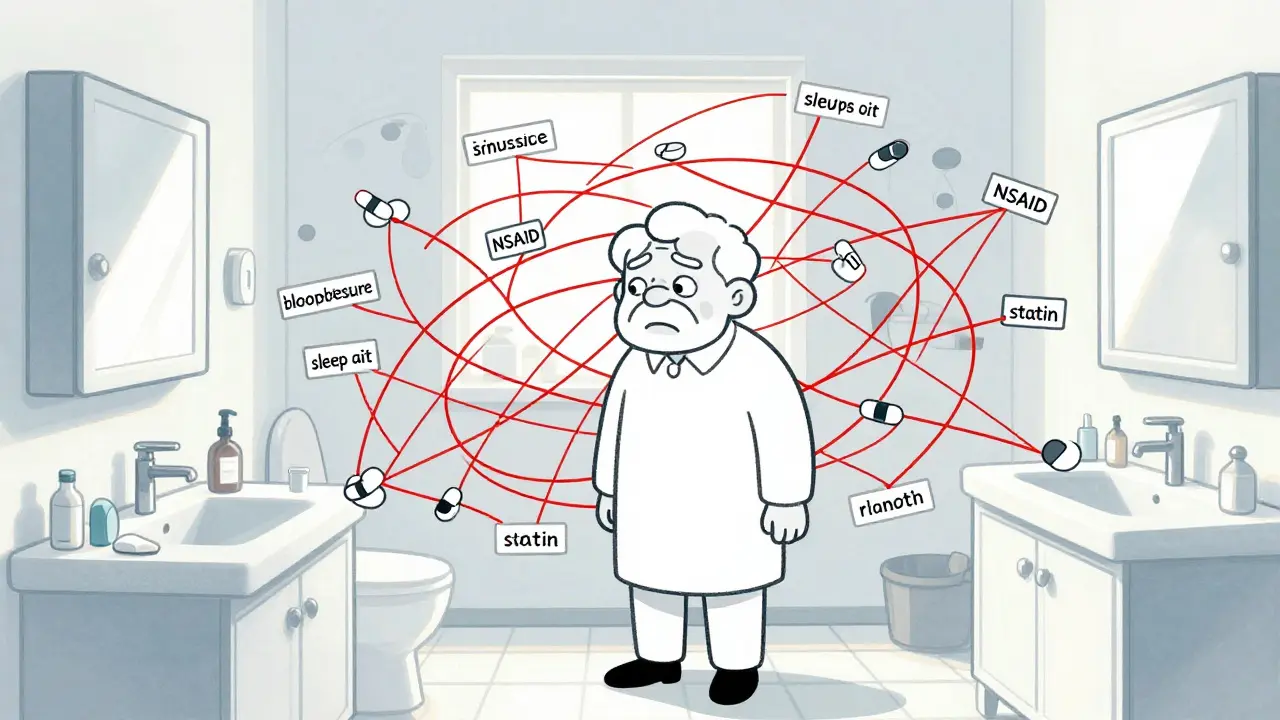
Common labeling mistakes - and how to spot them
Not all errors are obvious. Some look perfectly normal. Here are the top five mistakes you’re most likely to see:- Look-alike, sound-alike (LASA) errors: These happen when two drugs have names that look or sound similar. Think cycloserine vs. cyclosporine, or hydralazine vs. hydroxyzine. There are over 1,500 such pairs flagged by the FDA. The fix? Look for tall-man lettering - where part of the name is capitalized to show the difference. GLIpiZIDE vs. glyBURide. If you don’t see it, ask. Most pharmacies still don’t use it consistently.
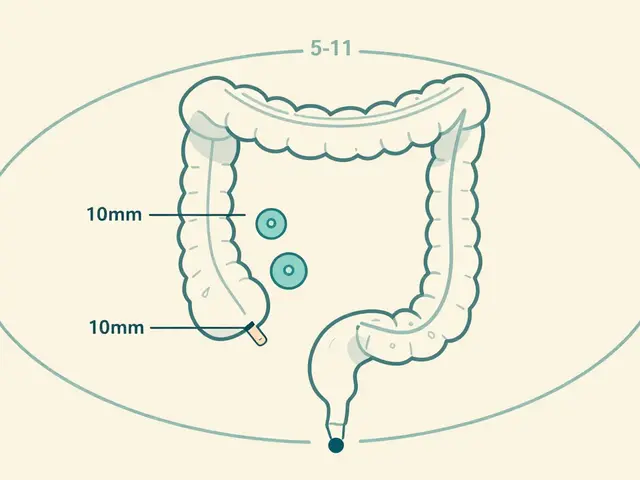
- Dosage strength errors: A decimal point in the wrong place can mean a 10x overdose. Warfarin, insulin, and levothyroxine are top culprits. If your label says "5 mg" but your doctor prescribed "0.5 mg," you’re in danger. Read the number out loud. Say it to yourself: "Zero point five milligrams." If it sounds off, it probably is.
- Wrong dosage form: Did you get a tablet when you were supposed to get a liquid? Or a capsule when you need a patch? These errors are common in elderly patients or those with swallowing issues. Check the shape, size, and wording. "Tablet," "capsule," "solution" - these words matter.
- Wrong patient name: Yes, this still happens. I’ve seen cases where a label had the right drug but the wrong person’s name. Always check your full name and date of birth. If it’s wrong, don’t take it.
- Incorrect directions: "Take one by mouth twice daily" vs. "Take one by mouth every 12 hours" - these sound similar, but they’re not the same. If your doctor told you to take it with food, but the label says "on an empty stomach," stop and ask.
How to check your label - a simple 4-step system
You don’t need to be a pharmacist to catch an error. Just follow this quick routine every time you pick up a new prescription:- Compare it to your doctor’s prescription. Did your doctor write "metformin 500 mg twice daily"? Does the label say the same? If your doctor changed the dose, did they tell you? If not, double-check.
- Read the drug name aloud. Say it slowly. If it sounds like another drug you’ve taken before, pause. Say it out loud to the pharmacist. Hearing it helps your brain catch mismatches your eyes miss.
- Check the strength with your fingers. Point to the number. Is it "10 mg" or "1.0 mg"? If you see a zero after a decimal - like "5.0 mg" - ask if it’s supposed to be "0.5 mg." That’s a classic mistake.
- Ask: "Why am I taking this?". If the label doesn’t say, ask the pharmacist. If they say "for your condition," push back. "Which condition? My blood pressure? My cholesterol? My pain?" If they can’t say it clearly, something’s wrong.
This takes 60 to 90 seconds. It’s not a hassle - it’s a lifesaver.
High-alert medications: Be extra careful
Some drugs are more dangerous if given wrong. These are called "high-alert medications." They include:- Insulin
- Warfarin (blood thinner)
- Hydromorphone (opioid painkiller)
- Epinephrine (for allergic reactions)
- Chemotherapy drugs
These account for 65% of serious errors that lead to hospitalization or death. If you’re getting any of these, treat the label like a bomb squad checklist. Don’t just glance. Verify. Double-check. Ask again. If you’re unsure, don’t take it. Call your doctor or go back to the pharmacy.
Why people don’t check - and how to overcome it
Most people don’t check their labels because they trust the pharmacy. Or they don’t know what to look for. Or they’re afraid of looking foolish.Here’s the truth: pharmacists are human. They’re busy. They make mistakes. A 2020 study found that even pharmacist double-checks miss 3.4% of errors. That’s one in 30 prescriptions. If you’re the last person to see it, you’re the last chance to stop harm.
And you’re not being rude by asking. In fact, pharmacists want you to. A 2022 study found that 89% of patients who checked their labels against previous bottles caught errors - compared to just 42% who didn’t. The most successful checkers didn’t just look - they compared. They held their last bottle next to the new one. They read both labels side by side.
If you’re older, have trouble reading small print, or don’t speak English well, ask for help. Many pharmacies now offer audio labels. CVS’s "Label Lens" lets you scan a QR code and hear your medication details spoken aloud. Some pharmacies even have staff trained to walk you through it - no shame in asking.
New tools to help you stay safe
Technology is catching up. In 2024, new rules require all pharmacy labels to use at least 12-point font and high contrast (4.5:1) so seniors can read them. Apps like MedSafety Check can scan your label with your phone’s camera and compare it to your prescription database - with 94.7% accuracy.But tools alone won’t fix the problem. The real change comes when patients stop feeling like they’re "bothering" the staff. You’re not bothering them. You’re helping them. One nurse on Reddit caught a 10x warfarin error because she asked, "Wait, why is this so much higher than last time?" That saved her from a life-threatening bleed.
What to do if you find a mistake
If you spot an error:- Don’t take the medication.
- Take the label and the bottle back to the pharmacy.
- Ask them to double-check the prescription with your doctor.
- If they dismiss you, call your doctor directly.
- Report it to your state board of pharmacy - most have online forms.
Don’t wait. Don’t assume it’s a typo. Don’t think "it’s probably fine." If it doesn’t match what you were told, it’s not fine.
What should I do if my pharmacy label doesn’t include why I’m taking the medication?
Ask the pharmacist to write it in or call your doctor to confirm. The indication is a critical safety feature - without it, you can’t tell if you’ve been given the wrong drug. If they refuse, ask for a printed copy of your prescription from your doctor’s office to compare. You have the right to know why you’re taking any medication.
Can I use my phone to check if my prescription label is correct?
Yes. Apps like MedSafety Check (launched in 2022) let you take a photo of your label and compare it to your doctor’s prescription using the RxNorm database. These apps are 94.7% accurate at catching mismatches. CVS also offers a QR code scanner on labels in over 5,200 stores that plays an audio description of your medication. Use them - they’re free and designed for exactly this.
Why do pharmacies make labeling errors so often?
Most errors happen because pharmacies are overwhelmed. They process over 4 billion prescriptions a year in the U.S. alone. Many use manual systems, and staff are under pressure to fill prescriptions quickly. Only 32% of community pharmacies use barcode scanning to prevent errors - compared to 78% in hospitals. Technology helps, but human verification is still the most reliable final check.
Are some drugs more likely to be mislabeled than others?
Yes. The FDA lists high-alert medications as the most dangerous when mislabeled. These include insulin, warfarin, morphine, hydromorphone, and chemotherapy drugs. Look-alike drugs like glipizide/glyburide, cycloserine/cyclosporine, and hydroxyzine/hydralazine are also common sources of error. Always double-check these - even if you’ve taken them before.
I’ve been taking this medication for months. Why should I check the label now?
Because prescriptions can change without you knowing. Your doctor may have switched you to a new drug, changed your dose, or added a refill. Your pharmacy may have run out of your usual brand and substituted a different one. Even if you’ve taken it before, each refill is a new chance for error. Never assume it’s the same.
Final reminder: Your eyes are your best safety tool
No system is perfect. Not the pharmacist. Not the computer. Not the barcode scanner. The final check - the one that stops harm before it happens - is yours. It takes less than two minutes. It doesn’t require special knowledge. Just attention. And the courage to ask.Next time you pick up a prescription, don’t just grab it and go. Stop. Read. Compare. Ask. You’re not being difficult. You’re being smart. And you might just save your life.



Comments
11 Comments
Mark Kahn
Just picked up my metformin yesterday and did the 4-step check. Turned out they gave me 1000mg instead of 500mg. Asked them to double-check - they apologized and fixed it right away. Seriously, folks, take 90 seconds. It’s not a hassle, it’s your life.
Anne Nylander
OMG YES!! I used to just grab my pills and run till my aunt almost took someone else's blood thinner. Now I read everything out loud. Even if I'm in a rush. No more guessing!!
Franck Emma
I once took a 10x warfarin dose because I didn't check. Ended up in the ER. Don't be me.
Leo Tamisch
How quaint. In my day, we trusted professionals. Now we're all amateur pharmacists with our QR scanners and audio labels. 😒
But fine. If you need to stare at a label like it's the Rosetta Stone to avoid a cosmic catastrophe, I suppose that's your kink.
Daisy L
THIS IS WHY AMERICA IS FALLING APART!! People don't check labels because they're too lazy to care!! We've turned pharmacies into fast-food joints and now we're surprised people die from a misplaced decimal point?!?!?!?!
My grandma used to write down every med she took on a notecard - and she was 82 and didn't own a smartphone!! We've lost our minds!!
Pravin Manani
From a clinical perspective, the omission of indication on labels represents a critical gap in the pharmacovigilance chain. The cognitive load on patients is significantly increased without semantic context - particularly with high-alert agents like anticoagulants or insulin. The 63% reduction in error rates with indication inclusion is statistically robust (p<0.001, CI 95%).
Moreover, LASA errors are exacerbated by non-standardized tall-man lettering protocols across dispensing systems. The FDA's 2023 guidance recommends mandatory implementation, yet only 19% of community pharmacies comply. This is a systemic failure, not an individual one.
Technology like MedSafety Check is a stopgap, not a solution. We need interoperable EHR-pharmacy integration with real-time alerting, not patient-driven verification as the primary safety layer. We're putting the burden on the most vulnerable - elderly, non-native speakers, cognitively impaired - while the infrastructure remains under-resourced.
Noah Fitzsimmons
Oh wow, you mean you’re supposed to READ the label? Like, actually look at the words? I thought you just shook the bottle and hoped for the best. 😂
Also, who the hell writes "for high blood pressure" on a label? That’s like putting "for breathing" on your oxygen tank.
Eliza Oakes
Wait - so you're telling me we're supposed to ACTUALLY VERIFY our meds? Like, not just trust the system? That’s just... so... American. I mean, in Sweden, they just hand you the pills and say "here, you’re fine." Why do we have to turn everything into a survival game?
Chris Vere
There is a deeper truth here beyond the mechanics of checking labels. We live in a world where trust has been commodified and replaced by verification protocols. We are taught to question the authority of the pharmacist because the system has failed us so often that even the most well-intentioned professional cannot be fully relied upon.
But consider this - if your life depends on reading a tiny font on a slip of paper, then the system has already lost. We have outsourced our health to institutions that are structurally incapable of safeguarding it - and now we are told to become our own pharmacists, our own doctors, our own regulators.
Is this progress? Or is it the quiet collapse of collective care, disguised as personal responsibility?
Corra Hathaway
YESSSSS this is so important!! I used to think I was being annoying asking questions - until my sister almost got the wrong chemo dose because the label said "5mg" instead of "0.5mg" 😭
Now I bring my old bottle to the pharmacy every time and say "compare these, please" - and guess what? They LOVE it. They feel supported!! 🙌
Also - use the QR code!! It talks to you!! It’s like a little voice angel telling you you’re safe 💖
Clifford Temple
Stop being so weak. If you can't read a label, don't take medicine. Simple. No apps. No QR codes. No crying. You want to live? Pay attention. This isn't a daycare. It's America. We don't coddle people who can't handle a 12-point font.
Write a comment