When a nurse pulls a vial of concentrated potassium chloride from the automated dispensing cabinet, or a pharmacist prepares an IV bag of insulin for a diabetic patient, the stakes aren’t just high-they’re life-or-death. One wrong decimal point, one misread label, one rushed step, and the result can be cardiac arrest, brain damage, or death. That’s why certain medications require extra verification procedures-not as a formality, but as a non-negotiable safety net.
What Makes a Medication "High-Risk"?
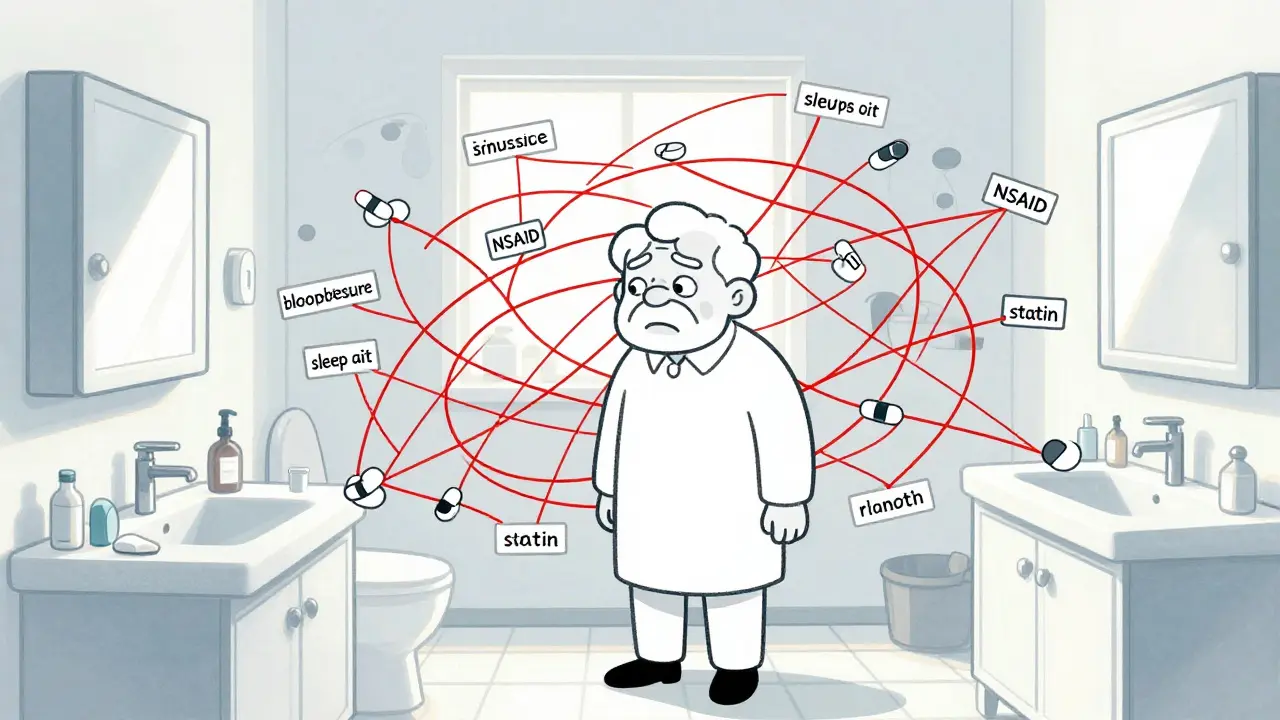
Not all medications are created equal when it comes to danger. High-risk medications, often called high-alert medications, are drugs that carry a heightened risk of causing serious harm if used incorrectly-even if the error seems small. The Institute for Safe Medication Practices (ISMP) has been tracking these since the early 2000s, and their list is updated regularly based on real-world error data.These aren’t just "strong" drugs. They’re drugs where the margin for error is razor-thin. For example:
- IV insulin: A dose of 10 units instead of 1 can send a patient into a coma within minutes.
- IV heparin: Too much can cause uncontrolled bleeding; too little can lead to deadly clots.
- Concentrated potassium chloride: A single vial contains enough to stop a heart if given by IV without proper dilution.
- Chemotherapy agents: Even small dosing mistakes can destroy bone marrow or damage vital organs.
- IV opioids like morphine or fentanyl: Overdose can cause respiratory arrest within seconds.
These aren’t theoretical risks. In 2021, the ECRI Institute reported that over 40% of fatal medication errors in hospitals involved one of these high-alert drugs. The error wasn’t always a calculation mistake-it was often a misread label, a skipped double check, or a distracted provider.
When Is a Double Check Required?
The standard for safety in these cases is the independent double check (IDC). It’s not just two people looking at the same thing. It’s two qualified professionals verifying each step-separately, without influence from each other.Here’s what a true independent double check looks like:
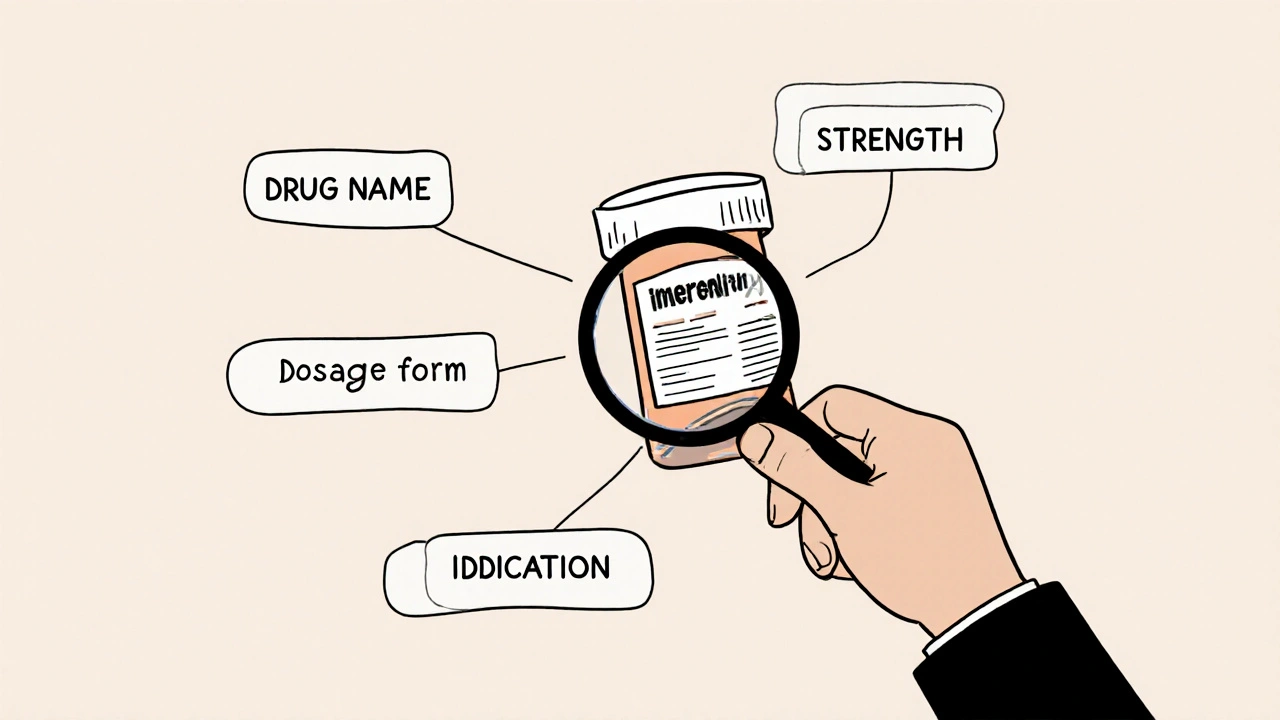
- The first provider prepares the medication and checks all details: patient name, drug name, dose, route, expiration, and appearance.
- The second provider-without seeing the first person’s work-goes through the same checklist from scratch.
- Both independently confirm the "Nine Rights": right patient, right drug, right dose, right route, right time, right documentation, right reason, right response, and right to refuse.
- Both sign the Medication Administration Record (MAR) or electronic equivalent.
This isn’t optional. The Joint Commission requires it. The Department of Veterans Affairs mandates it. Hospitals across the UK and US have policies spelling out exactly which drugs trigger this process.
Providence Health, for example, requires double checks for all IV opioids, TPN, antiarrhythmics, beta blockers, and calcium channel blockers. The VHA includes all chemotherapy, insulin, and heparin-regardless of route. In NICUs, every high-alert drug gets this level of scrutiny. Pediatric units often extend it to all cardiac medications.
Who Can Perform the Verification?
Not just anyone can be the second checker. The person must be qualified, trained, and licensed to handle the medication. That usually means:- Registered nurses with current competency in high-alert meds
- Pharmacists
- Physicians, nurse practitioners, or physician assistants
Technicians, students, or unlicensed staff are not permitted. Why? Because they might not recognize a dangerous error. A nurse might spot that a vial of heparin is labeled 10,000 units/mL instead of 1,000-but a student might not know the difference.
And here’s the critical part: the second person can’t just nod along. They must independently calculate doses, verify concentrations, and visually inspect the medication. If the first person says, "It looks right," the second person must ask, "How do you know?"

The Real Problem: Double Checks Are Often Broken
Here’s the uncomfortable truth: many double checks are just theater.A 2022 ISMP survey found that 68% of nurses admitted skipping required double checks during busy shifts. Why? 42% said there simply wasn’t a second person available. Others said it took too long. Some admitted they just "knew the med was right"-a dangerous assumption.
Worse, some teams do "double checks" by standing side-by-side, watching each other’s work. That’s not independent. That’s confirmation bias. If the first person misreads 5 mg as 50 mg, the second person is likely to see the same thing and assume it’s correct.
Studies published in the Journal of Patient Safety show that when double checks are performed poorly, they create a false sense of security. Nurses feel safer, but errors still slip through.
Technology Is Changing the Game
Barcode scanning at the bedside is now the gold standard for verifying patient and drug identity. If the system says, "This insulin doesn’t match the order for this patient," it stops the process cold. No human error. No assumption. No bypass.But technology doesn’t fix everything. It can’t catch:
- Wrong concentration in a premixed bag
- Incorrect dilution of a vial
- Misprogrammed infusion pump rates
- Look-alike, sound-alike drug labels
That’s why manual double checks still matter-for the moments when tech can’t help. For example, when a pharmacist prepares a custom chemotherapy blend, no barcode can confirm the right drug was added in the right amount. That’s where human eyes and brains are irreplaceable.
The VA is now combining both: barcode scanning for patient and drug ID, plus manual double checks only for high-risk preparations like IV push medications or compounded infusions.
What’s the Future of Medication Safety?
The trend is clear: fewer, smarter double checks-not more.Instead of requiring double checks for every high-alert drug in every situation, hospitals are now asking: "What are we trying to catch?"
For IV insulin, the goal is catching the wrong dose. So the focus is on dose verification and pump programming. For heparin, it’s concentration and route. For potassium chloride, it’s dilution and labeling.
Organizations are now designing targeted verification steps based on actual error patterns, not blanket rules. This reduces staff burnout and increases effectiveness.
Training is also evolving. Instead of annual PowerPoint slides, staff now get hands-on simulations with real vials, pump settings, and error scenarios. One hospital in Bristol reported a 70% drop in near-misses after implementing monthly safety drills with pharmacists and nurses working together.
What You Can Do
If you’re a nurse, pharmacist, or provider:- Never skip a double check-even if you’re tired or rushed.
- Insist on true independence. Don’t let someone "just look over your shoulder."
- Speak up if you see a colleague cutting corners. Safety isn’t optional.
- Know your facility’s list of high-alert medications. If it’s not posted, ask for it.
- Use technology when it’s available, but never rely on it alone.
If you’re in leadership:
- Don’t just require double checks-train for them. Practice them.
- Make sure staffing allows time for verification. No one should be forced to choose between speed and safety.
- Review your error data. Are most mistakes happening with insulin? Heparin? Then focus your efforts there.
Medication safety isn’t about rules. It’s about culture. It’s about recognizing that behind every vial, every dose, every IV bag, is a person who trusts you to get it right. And sometimes, getting it right means taking two extra minutes to double-check-before it’s too late.
What medications require a double check in hospitals?
Medications that require independent double checks include IV insulin, IV heparin, concentrated potassium chloride, chemotherapy agents, epidural or IV opioids, and TPN. Some hospitals also require it for antiarrhythmics, calcium channel blockers, and cardiac medications in pediatric or neonatal units. Each facility develops its own list based on ISMP guidelines and internal error data.
Can a nurse and pharmacist both do the double check?
Yes. In fact, having a nurse and pharmacist perform the double check is often ideal because they bring different perspectives. The nurse focuses on patient safety and administration, while the pharmacist verifies dosage accuracy, compatibility, and preparation. Both must independently verify all steps without influencing each other.
Is a double check always necessary for insulin?
Yes-for all forms of insulin, especially IV and concentrated forms. Even small dosing errors can cause severe hypoglycemia or hyperglycemia. Many hospitals require two people to verify the dose, concentration, and patient identity before administration, regardless of whether it’s given by syringe, pump, or pen.
Why do some nurses skip double checks?
The most common reasons are staffing shortages, time pressure, and fatigue. In high-volume units like the ER or ICU, nurses may feel they can’t afford the extra minutes. But studies show skipping these checks increases the risk of fatal errors. Facilities that build safety into workflow-like having dedicated verification times or using tech to reduce manual steps-see better compliance.
Do barcode scanners replace the need for double checks?
No. Barcode scanners confirm the right patient and right drug, but they can’t catch wrong concentrations, incorrect dilutions, or pump programming errors. Manual double checks are still essential for complex preparations like chemotherapy or IV push medications. The best approach combines both: tech for identity, humans for safety.
What happens if a double check misses an error?
If an error slips through, the facility must conduct a root cause analysis. Was the double check done properly? Was the staff trained? Was the process too complex? The goal isn’t to blame individuals-it’s to fix the system. Many hospitals now use near-miss reporting to improve processes before a patient is harmed.




Comments
11 Comments
david jackson
Let me tell you something that keeps me up at night: I’ve seen a nurse hand a vial of concentrated KCl to a tech with no dilution label, and the tech just shrugged and said, 'It’s probably fine.' That’s not negligence-it’s systemic collapse. We’ve turned safety checks into checkboxes because we’re understaffed, overworked, and emotionally bankrupt. And yet, when a patient codes? We point fingers. The system doesn’t fail because people are bad-it fails because we’ve normalized the unsustainable. Double checks aren’t bureaucracy-they’re the last breath before the heart stops. If your hospital doesn’t have dedicated time for them, you’re not a healthcare provider-you’re a liability waiting for a headline.
Zina Constantin
As a nurse who’s worked in three different hospitals across three states, I can tell you this: the double-check culture isn’t broken-it’s been abandoned. We need to stop treating safety like a policy document and start treating it like a sacred ritual. Every time I verify insulin with a pharmacist, I say out loud: 'Patient name, drug name, dose, route, expiration.' Not because the form says so-but because I owe that person my full attention. If you’re rushing, you’re not healing-you’re gambling. And no one deserves to be a roll of the dice.
Angela Spagnolo
I… I just… I’ve seen so many near-misses, and I don’t know if I’m brave enough to speak up anymore. I’m scared if I say something, I’ll be labeled 'difficult' or 'slow.' But last week, I caught a 10x overdose on heparin because I asked, 'Wait, why is this bag labeled 5000 units/mL?' and no one else had noticed. I didn’t get a thank you. I got a sigh. And now I wonder… is it worth it? Maybe I’m just being paranoid. But what if I’m not?
Sarah Holmes
It is an absolute moral outrage that healthcare institutions continue to permit the existence of a system wherein the lives of patients are entrusted to overworked, underpaid, and psychologically depleted personnel who are expected to perform precision medical tasks under conditions that would be deemed criminal in any other industry. The notion that a 'double-check' can be performed by a nurse who has been on a 12-hour shift with no break, while simultaneously managing five other critical patients, is not merely negligent-it is a form of institutionalized violence against the vulnerable. The Joint Commission should be sued. The administrators should be held personally accountable. This is not healthcare. This is a death sentence with a clipboard.
Jay Ara
i been a nurse for 15 years and i can say this - double checks save lives. but if u dont have time or help its not your fault. we need more staff not more rules. simple.
Michael Bond
True double checks work. Bad ones don’t.
Kuldipsinh Rathod
Back in India, we don’t have the same tech or staffing, but we still do double checks-because we know if we don’t, someone’s kid might not wake up. It’s not about money. It’s about respect. For the job. For the person. For the fact that we’re holding life in our hands. I wish more places here thought like that.
SHAKTI BHARDWAJ
Oh please. Double checks are just corporate theater to make administrators feel like they’re doing something while they cut your pay and fire your colleagues. The real problem? Hospitals are profit mills. They don’t care if you live or die-they care if the audit passes. I’ve seen a manager laugh when a nurse reported a near-miss because 'it didn’t hurt anyone.' Guess what? It almost did. And you know what? I’m done pretending this system cares about patients.
Matthew Ingersoll
The most dangerous myth in healthcare is that technology replaces human judgment. Barcode scanners tell you if the right drug is going to the right patient-but they can’t tell you if the dose is lethal, if the bag was mixed wrong, or if the pump is programmed for mL/hr instead of mcg/kg/min. Human eyes are still the final filter. And that’s not a weakness-it’s our responsibility.
carissa projo
Every time I do a double check, I think of my mother-how she used to say, 'If you’re going to hold someone’s life in your hands, do it like you’re holding a baby bird.' Not too tight. Not too loose. With reverence. We’ve lost that. We’ve turned safety into a checklist and compassion into an afterthought. But the truth? The most powerful tool we have isn’t a barcode or a policy manual-it’s the quiet moment when two professionals pause, look each other in the eye, and say, 'Let’s make sure.' That’s not procedure. That’s love in action.
Lori Anne Franklin
soooo i was on night shift last week and we were so swamped i just did a quick check on the insulin… and then i saw the post and i felt awful. like… i know i should’ve stopped. but i was so tired. and now i’m scared i did something bad. i’m gonna start doing it right again. promise.
Write a comment