Fluoroquinolone Side Effect Risk Calculator
This tool helps you understand your potential risk of tendon or nerve damage when taking fluoroquinolone antibiotics like ciprofloxacin or levofloxacin. Results are for informational purposes only and should not replace professional medical advice.
When you take an antibiotic like ciprofloxacin or levofloxacin for a sinus infection or urinary tract infection, you expect to feel better. But for some people, these drugs don’t just fight bacteria-they can start damaging tendons and nerves, sometimes permanently. The risks aren’t rare. They’re real, documented, and increasingly restricted by health agencies worldwide. If you’ve been prescribed a fluoroquinolone antibiotic, you need to know what’s at stake.
What Are Fluoroquinolones?
Fluoroquinolones are a class of broad-spectrum antibiotics that include ciprofloxacin, levofloxacin, moxifloxacin, and norfloxacin. They’ve been used since the 1980s to treat serious infections like pneumonia, complicated UTIs, and anthrax. Their strength lies in how deeply they penetrate tissues and how wide their range of action is. But that same power comes with a dark side: a growing list of serious, sometimes irreversible side effects.
By 2016, the U.S. Food and Drug Administration (FDA) issued a black-box warning-the strongest safety alert they can give-after reviewing hundreds of reports showing fluoroquinolones could cause disabling nerve and tendon damage. The European Medicines Agency (EMA) followed suit in 2019, restricting these drugs to only the most serious infections when no other options exist. In the UK, the MHRA updated its guidance in April 2019, saying fluoroquinolones should be avoided for mild infections like bronchitis or simple UTIs.
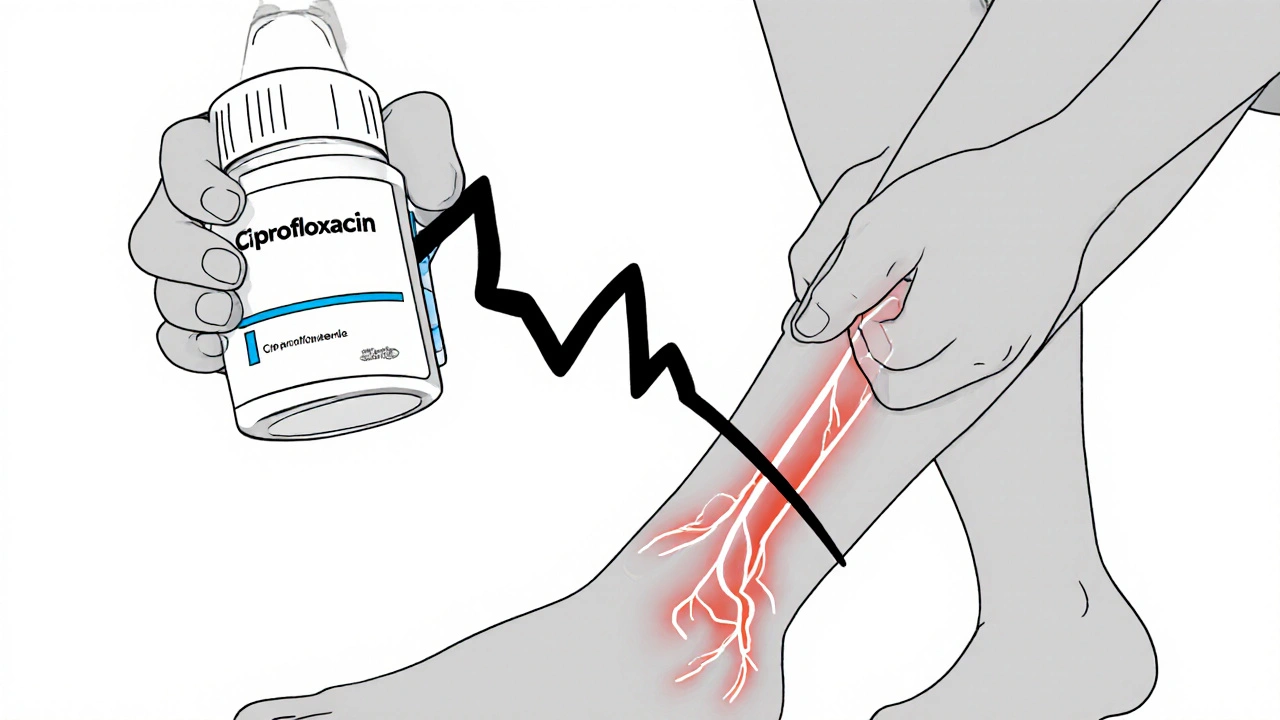
Tendinopathy: More Than Just a Strain
Tendinopathy from fluoroquinolones isn’t a typical sports injury. It’s sudden, often painless at first, and strikes without warning. The Achilles tendon is the most common target-accounting for nearly 90% of cases. But shoulders, hands, and rotator cuffs can also be affected.
Here’s what the data shows:
- Between 0.14% and 0.4% of people taking fluoroquinolones develop tendinopathy.
- Up to 40% of those cases turn into full tendon ruptures.
- Half of all tendon injuries happen after the antibiotic course is finished.
- Onset can be as early as 2 days-or as late as 152 days after starting the drug.
Age is a major factor. People over 60 are 2.7 times more likely to suffer a rupture. Those taking corticosteroids at the same time? Their risk jumps 46-fold. Diabetes and kidney disease also increase vulnerability. One study found that 50% of patients experienced symptoms in both tendons at once.
What does it feel like? A sharp, deep pain in the heel or shoulder, often described as “like a rubber band snapping.” Swelling may follow. Some patients report a popping sound at the moment of rupture. The damage doesn’t always heal cleanly. Up to 10% of affected individuals end up with chronic pain, reduced mobility, or permanent disability.
Nerve Damage: The Silent Threat
Peripheral neuropathy is another serious risk. This isn’t a pins-and-needles sensation you shake off. It’s damage to the nerves that control sensation and movement in your arms and legs. Symptoms include burning, tingling, numbness, and weakness. In some cases, it’s permanent.
Studies show about 4.3% of patients on fluoroquinolones develop this condition. Onset is usually within the first month of treatment, but again-delayed cases are common. Some patients report symptoms starting weeks or even months after stopping the drug. The FDA says this nerve damage can be irreversible, even after the antibiotic is gone.
Unlike muscle soreness or minor nerve irritation, fluoroquinolone-induced neuropathy doesn’t improve with rest or time. Many patients describe it as a slow, creeping loss of feeling that turns into constant discomfort. Some can no longer walk without support. Others lose fine motor skills-buttoning shirts, typing, or holding a cup becomes difficult.
Why Are These Risks So Overlooked?
Doctors aren’t ignoring the risks-they’re often unaware of how common or severe they are. A 2022 study found only 43% of primary care physicians correctly identified fluoroquinolone-induced tendinopathy in simulated cases. Patients are told it’s “just aging” or “overuse.”
Real patient stories paint a different picture. On Reddit’s r/floxing community, over 14,000 members share experiences of sudden tendon ruptures after a 7-day course of levofloxacin for a sinus infection. One user, “TendonWarrior,” described bilateral Achilles ruptures 12 days after finishing his prescription. He spent 11 months in rehab.
The Fluoroquinolone Effects Research Foundation has collected over 8,500 patient reports. Of those, 78% had tendon problems. Median symptom duration? 14 months. In Australia’s Floxie support group, 35% of members needed surgery. Many say their doctors dismissed their concerns until it was too late.
Who Should Avoid These Antibiotics?
Fluoroquinolones are not for everyone. Regulatory agencies now agree: they should be reserved for life-threatening infections with no alternatives. That means:
- Avoid for: uncomplicated UTIs, acute bronchitis, sinus infections, ear infections.
- Consider only for: complicated UTIs, hospital-acquired pneumonia, anthrax exposure, or severe infections unresponsive to safer antibiotics.
If you’re over 60, have kidney disease, are on steroids, have had a prior tendon injury, or have diabetes-you’re at higher risk. Ask your doctor: “Is this the safest option?”
What to Do If You’re Already Taking One
If you’re on a fluoroquinolone and feel any unusual pain, tingling, or weakness in your tendons or limbs-stop the drug immediately and call your doctor. Don’t wait. Don’t assume it’s just soreness. Tendon damage can progress rapidly.
Do not take corticosteroids while on fluoroquinolones. That combination is a known recipe for rupture.
Rest the affected area. Ice and elevation help. Avoid strenuous activity. Physical therapy may be needed later, but only under careful supervision.
Document everything. Write down when symptoms started, what you were doing, and how they’ve changed. This helps your doctor connect the dots.

Are There Safer Alternatives?
Yes. For most common infections, there are better, safer options:
- UTIs: Nitrofurantoin, trimethoprim-sulfamethoxazole
- Sinus infections: Amoxicillin, doxycycline
- Bronchitis: Usually no antibiotics needed, but if required, azithromycin or amoxicillin
- Pneumonia: Doxycycline, amoxicillin-clavulanate, or macrolides
These alternatives carry far lower risks of permanent damage. They may not be as broad-spectrum, but for most community infections, they’re just as effective-and much safer.
The Bigger Picture
The global use of fluoroquinolones has dropped 27% since 2015. In the U.S., prescriptions for simple UTIs fell from 17% to 5% in seven years. That’s because doctors are finally listening to the data.
But the damage has already been done for thousands. Many patients report long-term pain, mobility issues, and a loss of trust in the medical system. The FDA’s Sentinel Initiative is now tracking real-world outcomes across 150 million Americans. Researchers are testing drugs like doxycycline to see if they can prevent tendon breakdown in high-risk patients.
Fluoroquinolones aren’t going away. They’re still vital for life-threatening infections. But their role is shrinking-and it should. The cost of a few days of antibiotics shouldn’t be years of pain, disability, or loss of function.
If you’ve been prescribed one, ask: Is this truly necessary? If the answer isn’t clear, get a second opinion. Your tendons and nerves aren’t expendable.
Can fluoroquinolone tendon damage be reversed?
In some cases, yes-if caught early and treated properly. But for many, the damage is permanent. Up to 10% of patients experience long-term mobility issues, chronic pain, or reduced range of motion even after stopping the drug. Early discontinuation and rest improve outcomes, but full recovery isn’t guaranteed.
How soon after starting fluoroquinolones do side effects appear?
Symptoms can start as early as 2 days after beginning treatment, but most occur within the first month. Shockingly, half of all tendon injuries happen after the antibiotic is stopped. Some people report nerve or tendon pain weeks or even months later.
Are all fluoroquinolones equally risky?
No. Ciprofloxacin is the most commonly linked to tendon damage, followed by norfloxacin and levofloxacin. But all fluoroquinolones carry the same black-box warnings from the FDA and EMA. No one in this class is considered safe for routine use.
Can I take ibuprofen or other painkillers if I’m on a fluoroquinolone?
Avoid NSAIDs like ibuprofen if you’re at risk for tendon damage. They may mask early warning signs. Acetaminophen (paracetamol) is safer for pain relief, but the best approach is to stop the antibiotic entirely if symptoms appear. Never take corticosteroids with fluoroquinolones-this combination drastically increases rupture risk.
What should I do if my doctor insists on prescribing a fluoroquinolone?
Ask for the specific infection they’re treating and why other antibiotics won’t work. Request guidelines from the FDA, EMA, or MHRA that restrict fluoroquinolones to serious cases. If they dismiss your concerns, get a second opinion. Your health isn’t worth the risk for a mild infection.
Next Steps
If you’ve taken a fluoroquinolone and feel pain, numbness, or weakness-don’t wait. See a doctor who understands these risks. Bring printed guidelines from the FDA or MHRA if needed. If you’ve had a tendon rupture or nerve damage, consider joining a patient support group like the Fluoroquinolone Effects Research Foundation. You’re not alone.
For future prescriptions, always ask: Is this the safest option? If the answer isn’t clear, say no. Your body doesn’t owe you a quick fix.



Comments
13 Comments
Chuckie Parker
Stop coddling patients with this fearmongering. Fluoroquinolones save lives. If you can't handle a little tendon pain you shouldn't be running marathons anyway. The FDA is just being politically correct. People die from untreated pneumonia every day.
George Hook
I've been a family physician for 28 years and I've seen firsthand how the medical community has been slow to recognize the full scope of fluoroquinolone toxicity. What's alarming isn't just the incidence rate-it's the delayed onset, the fact that patients are often told it's just aging or overuse, and the complete lack of follow-up care once the prescription ends. I've had patients come in years later with chronic neuropathy and tendon degeneration, and the system has no protocol for them. We need mandatory patient education materials and a national registry to track long-term outcomes-not just warnings buried in tiny print.
jaya sreeraagam
As someone from India where antibiotics are sold over the counter like candy, I can't believe how lucky we are to have this info! My uncle took cipro for a 'bad cold' and ended up in a wheelchair for 8 months. He thought it was just arthritis. Please please please share this with your grandparents, your aunts, your neighbors. This isn't just science-it's survival. We need public service ads on TV, posters in pharmacies, even WhatsApp forwards. One person reading this could save a life. 💪❤️
Katrina Sofiya
Thank you for this comprehensive, evidence-based overview. As a healthcare professional, I am deeply grateful for posts like this that elevate patient safety above convenience. The data is unequivocal: fluoroquinolones should be reserved for life-threatening conditions only. I have personally discontinued prescriptions of these agents for uncomplicated UTIs and have seen dramatic improvements in patient outcomes. Let us continue to advocate for cautious, informed prescribing-not just for the sake of guidelines, but for the dignity and integrity of our patients' bodies.
kaushik dutta
Let's contextualize this. Fluoroquinolones are bactericidal topoisomerase inhibitors with high bioavailability and tissue penetration-phenomenal pharmacokinetics. But their off-target effects on mitochondrial DNA replication and collagen synthesis are well-documented in peer-reviewed literature. The real issue is not the drug-it's the diagnostic inertia in primary care. When a 62-year-old diabetic on prednisone presents with heel pain after cipro, and the clinician says 'it's plantar fasciitis,' that's systemic failure. We need antimicrobial stewardship programs integrated into EMRs with mandatory alerts. This isn't anti-antibiotic-it's pro-rational medicine.
doug schlenker
I took levofloxacin for a sinus infection back in 2018. Two weeks later, my Achilles started hurting. I thought it was from hiking. By month three, I couldn't walk without a cane. No doctor connected the dots until I showed them the FDA warning. Now I have permanent nerve damage in my feet. I'm not mad at my doctor-he didn't know. But we all need to know. Please, if you're reading this and you're about to take one of these-ask. Ask twice. Ask until they give you a real answer.
Denise Wiley
OMG I JUST READ THIS AND MY HEART IS RACING. My cousin got cipro for a UTI and ended up with a ruptured tendon and chronic neuropathy. She's 32. She can't wear heels anymore. She cries when she tries to dance. This isn't just a 'side effect'-it's a life-altering trauma. Why isn't this on every pharmacy flyer? Why aren't doctors REQUIRED to say this out loud? I'm sharing this everywhere. No one should go through this alone.
Nicola Mari
It's pathetic how people treat antibiotics like candy. If you can't wait a few days for a mild infection to clear on its own, you're not sick-you're lazy. Fluoroquinolones have saved countless lives. Your tendon pain is a consequence of your own poor lifestyle choices. Stop blaming the medicine and start taking responsibility for your body.
Leah Doyle
Wait so if I'm 58 and have diabetes and take prednisone for asthma... I should never get cipro? Even if I have a bad lung infection? What if I'm allergic to everything else? 😔 I just want to feel better. Is there a safe way to use these if I'm high risk? Or is it just... don't take them period?
Alexis Mendoza
Everything has a cost. Even life-saving drugs. The question is: what are we willing to trade? Speed of cure for years of pain? Convenience for disability? We've been trained to want instant fixes. But the body doesn't work that way. Maybe the real problem isn't the antibiotic-it's our expectation that medicine should be risk-free.
Michelle N Allen
So basically don't take antibiotics unless you're dying? Sounds good I guess. I mean I got cipro last year for a UTI and I'm fine so idk why everyone's making a big deal. Maybe it's just bad luck. Or maybe people are just sensitive. Anyway I'm gonna go eat tacos now
Madison Malone
If you're reading this and you're scared-you're not alone. I went through tendon rupture after cipro too. It took over a year to walk normally again. But I found a physical therapist who specialized in fluoroquinolone recovery. She changed my life. Please don't give up. There are people who understand. You can heal. You can still move. You can still live. I'm rooting for you.
Graham Moyer-Stratton
They banned it in Europe. That's the real story. America still sells it like soda. Weak.
Write a comment