Trying to get pregnant and wondering why it’s not happening? Your thyroid might be the quiet culprit. For many women, the issue isn’t infertility in the traditional sense-it’s a thyroid that’s just slightly off. And the fix? Often, it’s as simple as getting your TSH level into the right range before conception.
Why TSH Matters More Than You Think
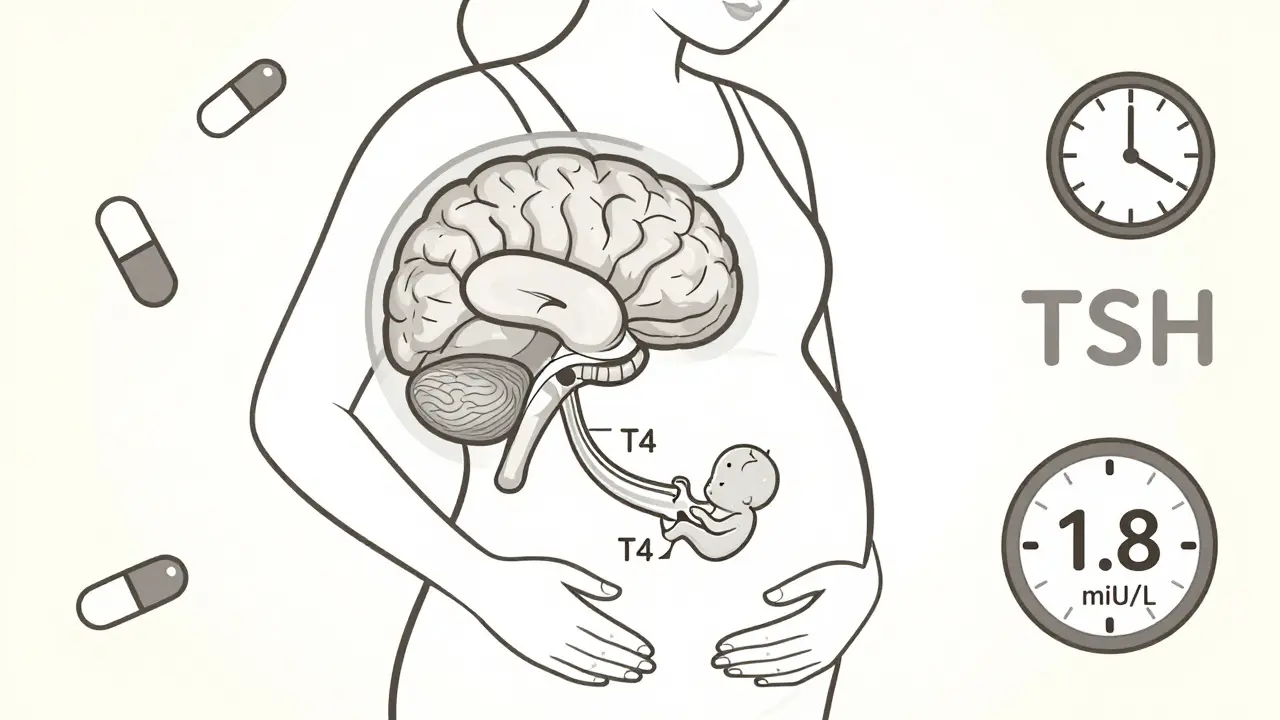
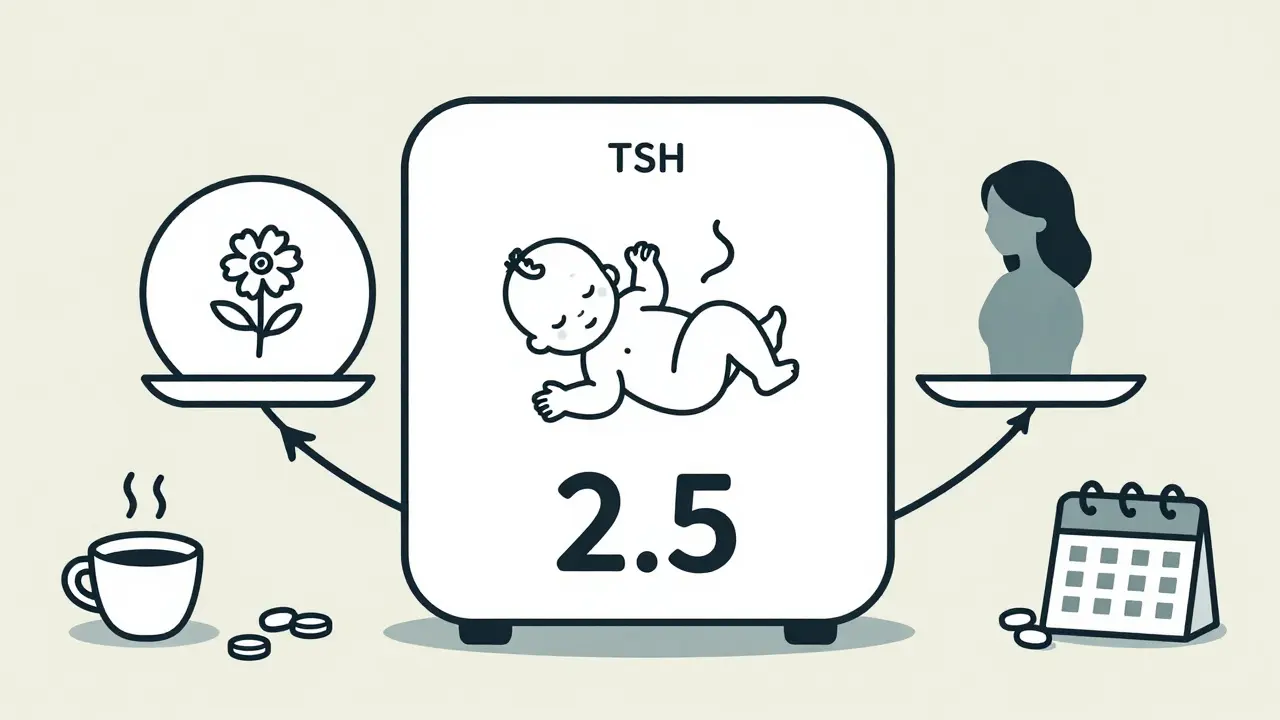
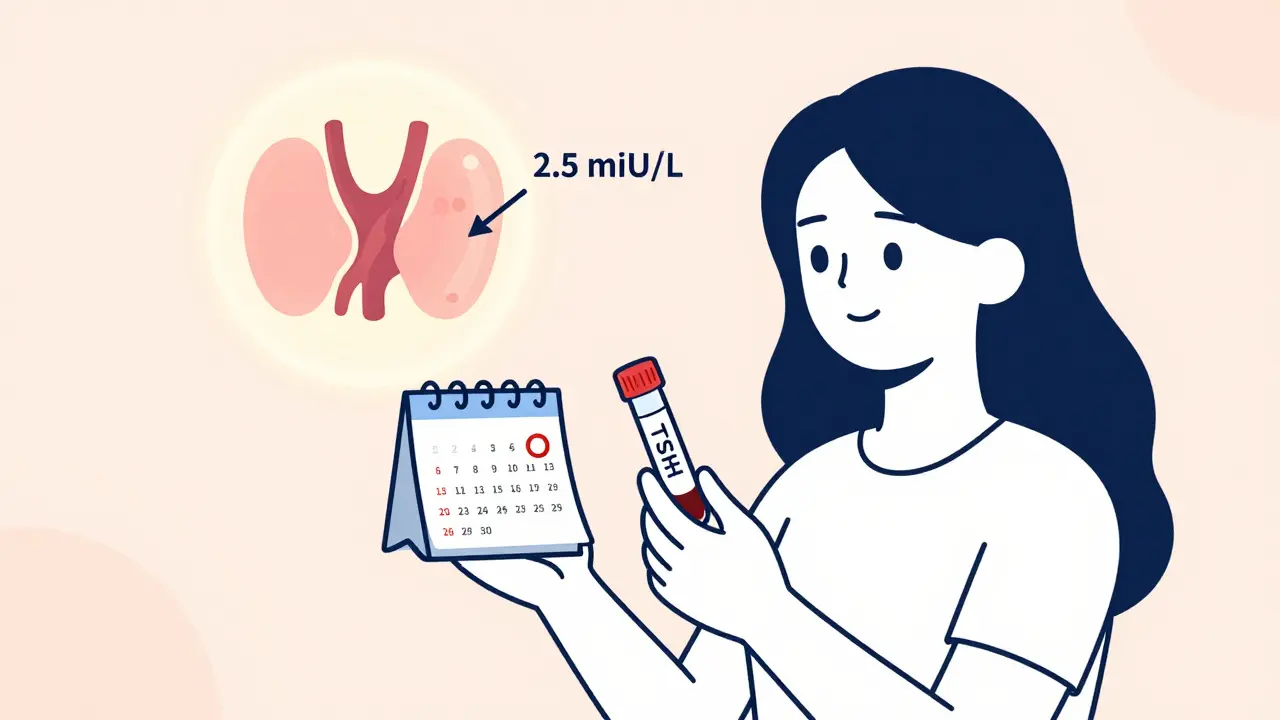
TSH, or thyroid-stimulating hormone, is the signal your brain sends to your thyroid gland to make more hormones. When TSH is too high, your thyroid isn’t working hard enough. That’s hypothyroidism. Even if your TSH is technically in the "normal" range-say, 3.5 or 4.0 mIU/L-it might still be too high for pregnancy. The American Thyroid Association (ATA) recommends that women planning to conceive keep their TSH below 2.5 mIU/L. That’s not a random number. It’s based on decades of research showing that higher TSH levels, even within the "normal" range, are linked to lower pregnancy rates, longer time to conception, and higher miscarriage risk. A 2018 study of over 7,000 women with unexplained infertility found nearly twice as many had TSH levels at or above 2.5 mIU/L compared to women who conceived easily. Another large study of 180,000 women showed that those with TSH levels between 2.5 and 4.5 had a 15% higher chance of miscarriage than those below 2.5. This isn’t about being "sick." It’s about optimizing your body for the massive hormonal shift pregnancy demands. Your thyroid has to work 30-50% harder during early pregnancy. If it’s already struggling before you conceive, your baby won’t get enough thyroid hormone when it matters most-during the first 12 weeks, when the fetal brain is forming and your own thyroid is the only source.Who Needs to Check Their TSH?
You don’t need to be diagnosed with hypothyroidism to benefit from a TSH test before trying to conceive. The American Society for Reproductive Medicine (ASRM) recommends screening all women seeking fertility help. But even if you’re not actively trying yet, you should consider testing if you have:- A family history of thyroid disease
- Hashimoto’s thyroiditis (even if you’re not on medication)
- Unexplained fatigue, weight gain, or irregular periods
- Previous miscarriage(s)
- Been trying to conceive for more than 6 months without success
What’s the Ideal TSH Level?
The target isn’t one-size-fits-all. Here’s what the experts say:- General preconception target: Below 2.5 mIU/L
- For women with Hashimoto’s: Aim for 1.25-1.75 mIU/L
- For women with antibodies but normal TSH: Consider treatment if trying to conceive, especially after a miscarriage
Levothyroxine: The Go-To Treatment
If your TSH is too high, levothyroxine is the standard treatment. It’s safe, effective, and cheap-usually $4 to $10 a month. But here’s what most doctors don’t tell you: you’ll need more after you conceive. Studies show that 63% of women with hypothyroidism don’t get their dose increased quickly enough after pregnancy starts. That’s dangerous. Your body needs 25-50% more levothyroxine by week 4-6 of pregnancy. If you don’t adjust, your baby’s brain development could be affected. Don’t wait for your OB to catch it. Work with your endocrinologist or fertility specialist before you get pregnant. Set a plan: get your TSH under 2.5, then schedule a blood test every 4 weeks while trying. Once pregnant, test again at 6 weeks, then again at 12 weeks. Many women need to increase their dose by 12.5-25 mcg right away. And avoid desiccated thyroid (like Armour Thyroid). It’s not stable enough for pregnancy. It can cause low T4 levels, which is exactly what you’re trying to avoid.How to Take Levothyroxine Right
Medication only works if you take it properly. Here’s the simple routine:- Take it on an empty stomach, first thing in the morning
- Wait at least 30 minutes before eating or drinking anything but water
- Avoid calcium, iron, or multivitamins within 4 hours of your dose
- Don’t switch brands without checking with your doctor-absorption can vary
What About Women With Normal TSH?
Not everyone needs treatment. If your TSH is below 2.5 and you have no thyroid antibodies, you’re likely fine. But if you’ve had a miscarriage, or if you’re over 35 and trying for more than 6 months, testing for antibodies is worth it. And if your TSH is between 2.5 and 4.5? That’s where things get murky. Some studies, like one from 2017, found no difference in pregnancy rates between women with TSH levels of 2.5-4.5 and those below 2.5. But those studies focused on women undergoing IVF or IUI. They didn’t look at natural conception or miscarriage rates. The bigger picture? If you’re trying to conceive naturally and your TSH is above 2.5, the risk isn’t zero. It’s small, but real. And since levothyroxine is safe and inexpensive, many experts say: why wait?Costs and Benefits
Levothyroxine costs about $4-$10 a month. A single miscarriage? Around $7,200 in medical costs, not counting emotional toll or lost time. A preterm birth? Even more. A 2021 economic analysis found that optimizing TSH before pregnancy saves $1,850-$2,400 per pregnancy by reducing miscarriages and preterm deliveries. That’s not just money-it’s peace of mind. And the long-term impact? The Global Thyroid Health Initiative estimates that universal preconception TSH screening could prevent 65,000-80,000 miscarriages in the U.S. every year. That’s more than the number of babies born in a mid-sized city.What’s Changing in 2026?
The ATA is currently reviewing new guidelines. A major NIH trial (NCT03856002) finished in late 2024 and is analyzing whether personalized TSH targets-based on thyroid reserve and antibody status-work better than the universal 2.5 cutoff. Early results suggest that women with low thyroid reserve (meaning their gland can’t ramp up easily) benefit most from tighter targets. That could mean future guidelines won’t just say "keep TSH under 2.5," but "keep TSH under 1.8 if you have antibodies and a history of miscarriage." For now, the safest, most evidence-backed advice remains: if you’re planning to conceive, get your TSH checked. If it’s above 2.5, talk to your doctor about levothyroxine. Don’t wait for a diagnosis. Don’t wait for a miscarriage. Optimize your thyroid before you get pregnant.It’s one of the few things in fertility care that’s simple, safe, cheap, and backed by strong science.
Should I get my TSH checked if I’m not trying to get pregnant yet?
Yes-if you have any risk factors. Family history of thyroid disease, unexplained fatigue, weight gain, irregular periods, or a history of miscarriage are all reasons to get tested. Even if you’re not trying now, knowing your TSH level helps you plan. It’s easier to adjust your thyroid before pregnancy than during it.
Can I just wait until I’m pregnant to check my TSH?
Not recommended. By the time you’re pregnant, your thyroid needs have already jumped by 30-50%. If your TSH was high before conception, your baby may have already missed critical thyroid hormone during the first 6-8 weeks, when the brain is developing. Waiting until pregnancy to act puts your baby at risk. Preconception optimization is the goal.
Is a TSH of 3.0 dangerous for fertility?
It’s not an emergency, but it’s not ideal. Studies show women with TSH levels between 2.5 and 4.0 take longer to conceive and have higher miscarriage rates than those below 2.5. If you’ve been trying for more than 6 months without success, a TSH of 3.0 is a red flag worth addressing with your doctor.
Do I need to take levothyroxine for life?
Not necessarily. Many women with Hashimoto’s or mild hypothyroidism can reduce or stop levothyroxine after pregnancy, especially if their TSH returns to normal. But some will need it long-term. Your doctor will monitor your levels after delivery and adjust accordingly. Don’t stop on your own.
Can stress or diet affect TSH levels before conception?
Stress can temporarily raise TSH, but it won’t cause lasting thyroid dysfunction. Diet has minimal direct impact unless you have severe iodine deficiency-which is rare in the UK. The main issue is autoimmune thyroid disease (Hashimoto’s), which is genetic and not caused by lifestyle. Focus on getting tested, not on miracle diets.


Comments
5 Comments
rajaneesh s rajan
So let me get this straight - we’re telling women to pop a $4 pill to fix a number that’s technically "normal" just so they don’t cry in a doctor’s office later? I get the science, but it feels like we’re medicalizing normal human variation. My grandma had 7 kids with no TSH test and still lived to 92. Sometimes the body just knows.
Frank Declemij
TSH below 2.5 for preconception is supported by ATA guidelines and multiple meta-analyses. The 2018 study of 7000+ women with unexplained infertility showed a clear correlation. Levothyroxine is safe, cheap, and prevents avoidable miscarriages. This isn’t overmedicalization - it’s evidence-based optimization.
Eli In
OMG YES THIS. 😭 I had 2 miscarriages and my TSH was 3.2... my doctor said "it's fine" until I pushed for a second opinion. Started levothyroxine, got pregnant in 3 months. My baby is 1 now and thriving. Please, if you're trying, get tested. It's not a big deal, but it's a BIG deal for your future kid 🤱❤️
Megan Brooks
While the data supporting TSH targets below 2.5 mIU/L is compelling, it is also essential to acknowledge the potential for overtreatment and the psychological burden of pathologizing subclinical conditions. The decision to initiate levothyroxine should be individualized, particularly in the absence of thyroid antibodies or a history of adverse pregnancy outcomes.
Ryan Pagan
Let’s be real - if your TSH is above 2.5 and you’re trying to get pregnant, you’re basically playing Russian roulette with your baby’s brain development. Levothyroxine isn’t some scary drug - it’s just synthetic thyroid hormone. Your body makes it. The pill just fills the gap. And yeah, you’ll need more after you conceive. Don’t wait for your OB to catch it - go to your endo BEFORE you even stop using birth control. This is low-hanging fruit in fertility care. Stop overthinking it.
Write a comment