When your hip starts hurting, it’s easy to blame aging, overuse, or a bad workout. But if the pain lingers, especially with a deep ache in the groin or side of the hip, it might be something more specific: a labral tear or early hip arthritis. These aren’t just random injuries-they’re connected, often feeding off each other. And the most powerful tool to stop the cycle isn’t always surgery or pills. It’s how you move.
What’s Really Going On in Your Hip?
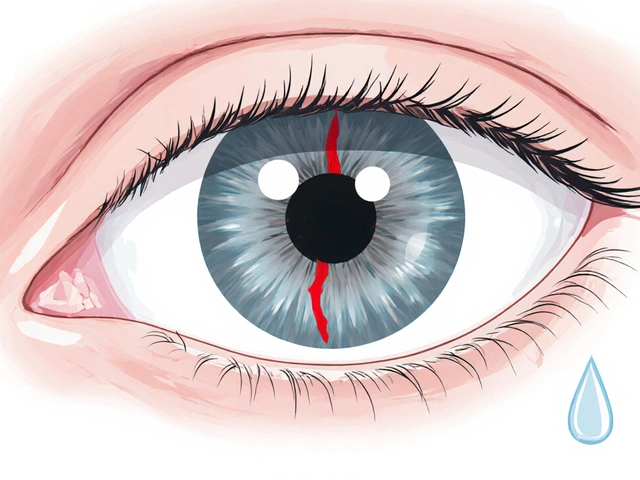
The hip joint is a ball-and-socket, but it’s not just bone meeting bone. Around the socket is a rubbery ring called the labrum-a 3 to 5 millimeter thick structure that acts like a gasket. It seals the joint, holds in lubricating fluid, and keeps the ball centered. When this ring tears, it doesn’t just hurt-it lets pressure build up inside the joint, grinding the cartilage faster. Labral tears are most common in the front (78% of cases), often from repetitive twisting or deep bending, like in yoga, soccer, or even sitting cross-legged for too long. At the same time, hip arthritis (osteoarthritis) slowly eats away at the smooth cartilage covering the ball and socket. It doesn’t happen overnight. It starts with stiffness, then a dull ache that flares after walking or climbing stairs. On X-rays, you’ll see narrowing of the joint space, bone spurs, and sometimes cysts. But here’s the key insight: you don’t need to have one to get the other. A labral tear can speed up arthritis by letting joint fluid leak out and increasing friction. And if you already have arthritis, the worn-down cartilage makes the labrum more likely to tear under normal stress. Studies show that 70-90% of people with a type of hip impingement called FAI (femoroacetabular impingement) have a labral tear. And in people with hip arthritis, over half have labral damage too-even if they never had a specific injury. This isn’t coincidence. It’s mechanics.Why Activity Modification Works Better Than You Think
Most people assume that if they have hip pain, they need to rest completely. That’s the wrong move. Sitting still for too long stiffens the joint, weakens the muscles, and makes pain worse. What you need isn’t less movement-it’s smarter movement. Activity modification means changing how you do things so you don’t trigger pain. It’s not about quitting life. It’s about redesigning it. For example, if you sit at a desk all day, your hips are bent past 90 degrees for hours. That’s the exact position that squeezes a torn labrum against the bone. Simple fixes: raise your chair so your knees are level with or slightly below your hips. Use a small cushion behind your lower back to tilt your pelvis forward slightly. This reduces pressure on the front of the hip. Sleeping? Avoid lying on the painful side. Put a pillow between your knees if you sleep on your back-it keeps your hips aligned and prevents internal rotation. If you’re a side sleeper, a longer pillow under your entire leg helps too. Exercise? Skip deep squats, lunges, and pigeon pose in yoga. These force the hip into flexion and rotation at the same time-the classic pain trigger. Instead, try swimming, cycling on a stationary bike with the seat high, or using an elliptical machine. These let you move without jamming the joint. One study found that 71% of people with hip pain could stay active with swimming or elliptical training, but only 29% could keep running without worsening symptoms. Even walking can be adjusted. Take shorter steps. Keep your hips level-don’t let one side drop when you step. If stairs are painful, go down backward. It shifts the load away from the front of the hip.What Not to Do (And Why)
There’s a lot of bad advice out there. “Just push through the pain.” “Stretch it out.” “Get a massage.” None of these fix the root problem. Stretching the hip too aggressively-especially into deep external rotation-can pull on a torn labrum and make it worse. Foam rolling the hip directly? That’s like pressing on a bruise. It might feel good for a second, but it adds stress to an already damaged area. Corticosteroid injections can help short-term. They reduce inflammation and give you a 3- to 4-month window to work on movement habits. But if you get more than three in a year, you risk damaging the cartilage further. And they don’t fix the tear or the arthritis-they just mask it. Same with viscosupplementation (hyaluronic acid shots). They’re meant to add lubrication, but in hips, they only help about half the people-and only for a few months. For someone with advanced arthritis, it’s like putting oil on a broken gear. The structure is already failing. And surgery? Hip arthroscopy to repair a labral tear works well-85-92% of patients report satisfaction after five years-if the tear is isolated and there’s no major cartilage loss. But if you already have Grade 3 or 4 arthritis (severe joint space narrowing), surgery won’t stop the degeneration. In fact, for people over 60 with advanced OA, 45% still end up needing a hip replacement within five years, no matter what you do.
When to Consider Surgery-and When Not To
Surgery isn’t the enemy. But it’s not the first step. The deciding factor isn’t pain level-it’s what the imaging shows. If you have a cam-type FAI (where the ball of the hip is misshapen, not perfectly round), and your alpha angle on MRI is over 55 degrees, surgery to reshape the bone plus repair the labrum gives you a 73% better chance of long-term success than just resting and doing PT. But if your X-ray shows bone-on-bone contact, large osteophytes, and less than 2mm of joint space, surgery won’t restore the cartilage. Your body has already moved past repair. At that point, the goal shifts from preservation to replacement. That’s when total hip arthroplasty becomes the most reliable option. The biggest mistake? Getting surgery for a labral tear when the real issue is arthritis. Dr. Thomas Vail at UCSF warns that many older patients are pushed toward surgery based on MRI findings alone-even when their symptoms don’t match. One study found that 38% of people over 50 have labral tears on MRI but feel zero pain. That means imaging alone isn’t enough. You need to correlate what you see with what you feel.Real People, Real Changes
A 45-year-old yoga teacher in Bristol had chronic groin pain. She couldn’t do downward dog or pigeon pose without sharp pain. Her MRI showed a moderate labral tear and early cartilage wear. She didn’t want surgery. So she worked with a physical therapist for six weeks. They taught her how to modify poses: reduce hip flexion to under 90 degrees, avoid twisting, and use blocks to support her hips. Three months later, her pain dropped 70%. She still teaches yoga-just differently. A 52-year-old office worker found that after 45 minutes at his desk, his hip locked up. He switched to a standing desk with a footrest, took walking breaks every 30 minutes, and started using a wedge cushion in his car. Within two months, he could drive to work without pain. He didn’t need an injection. He didn’t need surgery. He just changed how he sat. A retired runner in his late 60s had hip OA. He stopped running, switched to swimming three times a week, and started doing seated leg lifts to strengthen his glutes. He still walks his dog daily. He didn’t “cure” his arthritis-but he stopped it from controlling his life.
The Hidden Cost of Inaction
Ignoring hip pain doesn’t make it go away. It just lets it spread. A torn labrum increases contact stress on the cartilage by 92%, according to cadaver studies. That means every time you walk, jog, or even stand up from a chair, you’re grinding down your joint faster. And the longer you wait, the harder it gets. People who wait more than a year to make changes are 3.5 times more likely to need surgery within three years. But those who start activity modification early can delay surgery by 3.5 to 5 years-sometimes longer. The economic cost matters too. Conservative care-PT, modifications, occasional injections-costs $1,200 to $2,500 a year. Hip arthroscopy? $18,000 to $25,000. Total hip replacement? $35,000 and up. And insurance doesn’t always cover it. Medicare approves only 52% of surgeries for patients over 65, because the long-term benefit isn’t clear.How to Start Today
You don’t need a fancy device or a costly program. Just three steps:- Identify your pain triggers. What movement makes it worse? Deep squatting? Sitting cross-legged? Climbing stairs? Write it down.
- Find the alternative. If deep squats hurt, try chair squats-lower yourself only halfway. If sitting cross-legged hurts, sit with both feet flat. If walking uphill hurts, walk on flat ground with shorter strides.
- Build strength without pain. Focus on gluteus medius (hip abductor) exercises. Side-lying leg lifts, clamshells, and standing hip extensions-done slowly and controlled-strengthen the muscles that stabilize your hip. Aim for 80-100 degrees of hip flexion, never deeper.
What’s Next?
New tech is helping. Wearable sensors that give real-time feedback on hip position during daily activities reduced pain episodes by 52% in a 2023 Stanford study. Quantitative MRI can now detect cartilage wear before it shows on X-rays. And new injectables like Durolane last up to six months instead of three. But the real breakthrough isn’t in the lab. It’s in the living room, the office, the gym. It’s in the decision to move differently-not less. Your hip doesn’t need to be perfect. It just needs to be respected.Can a labral tear heal on its own?
No, the labrum doesn’t heal on its own because it has very little blood supply. Once torn, it won’t repair itself like a muscle or ligament. But that doesn’t mean you need surgery. Many people live pain-free by modifying how they move and strengthening the muscles around the hip. The goal isn’t to fix the tear-it’s to stop it from causing pain and further damage.
Is walking good for hip arthritis?
Yes, but only if done correctly. Walking keeps the joint lubricated and prevents stiffness. But long walks, uphill walking, or walking with poor posture can make it worse. Keep steps short, avoid uneven ground, and wear supportive shoes. If your hip hurts during or after walking, shorten your stride, reduce distance, or switch to a flat, soft surface like a track or treadmill. Walking 20-30 minutes a day is better than 60 minutes that leaves you in pain.
Does sitting make hip pain worse?
Yes, especially if you sit with your hips bent past 90 degrees for long periods. This pinches the front of the hip joint, irritating a torn labrum or worn cartilage. To reduce pressure, raise your chair so your knees are level with your hips. Use a lumbar cushion to tilt your pelvis forward slightly. Take breaks every 30 minutes to stand or walk for 2-3 minutes. Even small changes like this can cut pain by 40-60% over time.
Should I avoid all exercise if I have hip pain?
No. Avoiding movement leads to muscle weakness, which makes the hip less stable and increases pain. The key is to avoid movements that cause sharp pain-like deep squats, lunges, or twisting. Instead, focus on low-impact activities: swimming, cycling, elliptical training, and seated leg lifts. These strengthen the hip without stressing it. A physical therapist can help you find safe alternatives based on your specific condition.
When should I see a doctor for hip pain?
See a doctor if your pain lasts more than 4-6 weeks despite rest and activity changes, if it wakes you up at night, if you feel clicking or locking in the joint, or if you have trouble walking or standing. Early diagnosis matters. If you have FAI or early arthritis, starting physical therapy and movement modification within the first few months can delay surgery by years. Waiting too long reduces your options.
Can I still run with a labral tear or hip arthritis?
It depends. Some people can run with mild labral tears if they reduce mileage, run on soft surfaces, and strengthen their hips. But if you have arthritis with joint space narrowing or bone spurs, running is likely to speed up damage. Most people with hip OA find that switching to swimming or cycling gives them the same cardiovascular benefit without the impact. If you’re unsure, get a motion analysis test-it shows exactly how your hip moves during running and can tell you if it’s safe.
Is hip pain just part of getting older?
No. While hip arthritis becomes more common after 50, pain isn’t normal at any age. Many people over 60 live active, pain-free lives with proper management. Pain means something’s wrong-not just that you’re aging. Labral tears, for example, are common in active people in their 30s and 40s, not just older adults. Don’t accept pain as inevitable. Find out what’s causing it and how to fix it.



Comments
11 Comments
Lauren Warner
The data on labral tears and arthritis progression is solid, but what’s missing is the economic reality for people without good insurance. Most of these modifications require PT sessions, ergonomic gear, and time off work-all things that cost money. The article reads like a luxury guide for the well-off.
Craig Wright
It is imperative to note that the British National Health Service has long recognized activity modification as the primary intervention for early-stage hip degeneration. The over-reliance on surgical solutions in the United States is both financially irresponsible and medically unsound. This article, while accurate, fails to contextualize the systemic disparities in care.
Lelia Battle
There’s a quiet wisdom in the idea that we don’t need to fix everything to live well. The labrum doesn’t heal, but the body adapts-if we give it the right conditions. This isn’t about curing a tear. It’s about learning to coexist with it, like living with a scar that still remembers the wound but no longer screams every time you move. That’s the real healing.
Alex Fortwengler
They don't want you to know this but the whole labral tear thing is a scam pushed by ortho docs and MRI companies. 90% of people with 'tears' feel nothing. They're just selling surgeries to people who are scared of aging. You don't need PT, you need to stop listening to medical hype. Walk barefoot, squat deep, and ignore the pain. Your body knows better than some doctor with a clipboard.
jordan shiyangeni
It is profoundly concerning that the prevailing cultural narrative continues to promote the notion that pain is merely a signal to be managed through behavioral adjustments rather than a biomarker of structural pathology requiring clinical intervention. The article, while superficially pragmatic, dangerously romanticizes the avoidance of evidence-based treatment modalities-particularly when imaging correlates with symptomatology, as in the case of FAI with alpha angles exceeding 55 degrees. To equate biomechanical adaptation with therapeutic success is to misunderstand the progressive, irreversible nature of osteoarthritic degeneration. The notion that one can ‘live with’ a torn labrum without accelerating cartilage attrition is not only unsupported by longitudinal biomechanical studies but is, in fact, contradicted by cadaveric pressure mapping data demonstrating a 92% increase in contact stress. The author’s tone, while soothing, is clinically irresponsible.
steve ker
Labral tears? Just move different. Done.
gary ysturiz
This is the kind of advice that actually works. I’ve been dealing with hip stiffness for years and switched from running to swimming last year. No more pain on mornings. No surgery. No shots. Just smarter movement. If you’re reading this and hurting-don’t give up. Just change how you move. It’s not magic, it’s mechanics.
Jessica Bnouzalim
YES!! I’ve been doing the pillow-between-knees trick for months-and it’s changed my sleep! Also, chair squats instead of deep ones? Game changer. I used to think I had to suffer to stay fit, but now I know: movement isn’t about pushing through pain, it’s about listening to your body. Thank you for this! 🙌
laura manning
While the article presents a compelling narrative regarding activity modification, it is imperative to acknowledge the absence of longitudinal, randomized controlled trial data supporting the assertion that biomechanical adjustments alone can delay surgical intervention beyond three years. Furthermore, the citation of cadaveric studies without reference to inter-individual variability in joint kinematics introduces a significant methodological flaw. The recommendation to avoid corticosteroid injections beyond three per year lacks citation from peer-reviewed guidelines, and the economic cost analysis is misleading, as it omits indirect costs such as lost productivity and disability claims.
Bryan Wolfe
Love this. I’m 58, had a labral tear diagnosed 5 years ago, and I’m still hiking, gardening, and playing with my grandkids-just not the way I used to. I swapped deep squats for wall sits, stopped sitting cross-legged, and started using a wedge cushion in my car. No magic, just small changes. If you’re reading this and thinking ‘I’m too old’ or ‘it’s too late’-you’re not. Your hip doesn’t need to be perfect. It just needs you to be smart. Keep going.
Sumit Sharma
From a biomechanical standpoint, the emphasis on gluteus medius strengthening is empirically valid. However, the omission of neuromuscular re-education protocols-specifically proprioceptive training under dynamic loading-is a critical oversight. The referenced studies lack control for muscle activation timing, which is paramount in hip stabilization. Without EMG-guided feedback, activity modification alone risks compensatory movement patterns that exacerbate joint loading. Recommend integrating functional movement screening (FMS) with corrective exercise progression for optimal outcomes.
Write a comment