Why Reading Medicine Labels by Age and Weight Saves Lives
Every year, over 150,000 children in the U.S. end up in emergency rooms because of medicine mistakes. Most of these aren’t accidents-they’re caused by parents giving the wrong dose because they didn’t understand the label. It’s not about being careless. It’s about confusion. Medicine labels for kids don’t just say "give 5 mL." They list weight ranges, concentration numbers, and confusing abbreviations. One small mistake-a misread decimal, a kitchen spoon instead of a syringe, mixing up infant drops with children’s liquid-can mean the difference between healing and hospitalization.
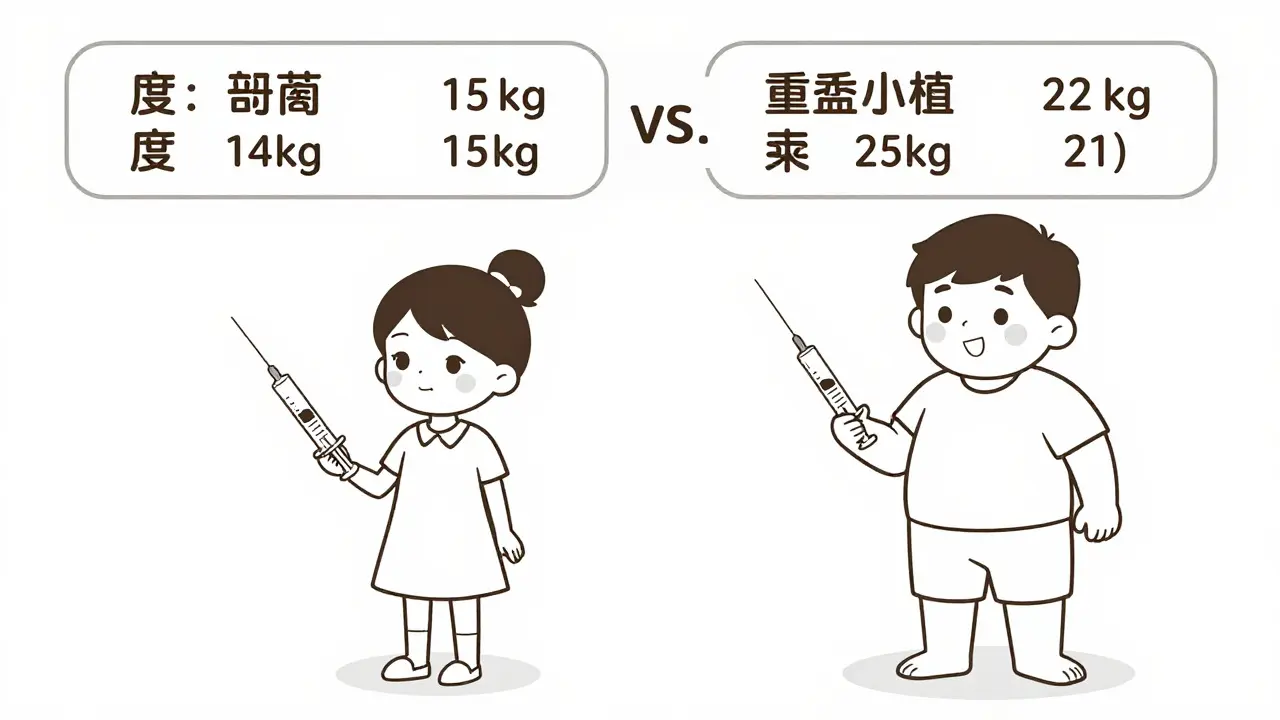
The truth? Age alone doesn’t tell you how much medicine to give. A 4-year-old who weighs 15 kg needs less than a 4-year-old who weighs 22 kg. But if you only look at the age chart on the bottle, you’ll give them the same dose. That’s why experts say weight-based dosing is the gold standard. The FDA, the American Academy of Pediatrics, and hospitals like Children’s Hospital of Philadelphia all agree: if you know your child’s weight, use it. Always.
The Seven Parts of a Children’s Medicine Label (And What They Really Mean)
Every over-the-counter kids’ medicine has a "Drug Facts" label. It’s not just text-it’s your safety guide. Here’s what each section actually tells you:
- Active ingredient: This is the medicine itself. Look for the name (like acetaminophen or ibuprofen) and the concentration. For example: "acetaminophen 160 mg/5 mL." That means every 5 milliliters contains 160 milligrams of medicine. This is the most important number. If you see "infant drops" at 80 mg/1 mL, that’s four times stronger than children’s liquid. Never use them interchangeably.
- Uses: What the medicine treats. Fever? Pain? Cough? Make sure it’s for the right symptom. Giving a cough medicine for a fever won’t help-and might cause harm.
- Warnings: This section tells you when NOT to give the medicine. Look for "Do not use in children under 2 years" or "Do not give with other medicines containing acetaminophen." This is where overdose risks are spelled out.
- Directions: Here’s where age and weight dosing live. You’ll see two charts: one by age (2-3 years, 4-5 years), and one by weight (24-35 lbs, 36-47 lbs). Always check both. If your child’s weight falls between two ranges, round up to the next dose. Never go below the lowest weight recommendation.
- Inactive ingredients: These are fillers, flavors, dyes. Important if your child has allergies. Some products contain alcohol, sugar, or artificial colors you might want to avoid.
- Purpose: Explains what the active ingredient does. "Pain reliever/fever reducer" tells you what it’s for, not how much to give.
- Other information: Storage tips, expiration date, and manufacturer info. Never use expired medicine.
Prescription labels add more: your child’s name, the doctor’s name, the pharmacy’s phone number, and the exact strength (like "amoxicillin 250 mg/5 mL"). Always double-check the name on the bottle matches your child’s. Mistakes happen.
Weight vs. Age: Why Weight Always Wins
Many labels still list age ranges because they’re easier to remember. But here’s the hard truth: age is a poor substitute for weight. A 3-year-old can weigh anywhere from 12 kg to 20 kg. That’s a 67% difference in body mass. Giving the same dose to both? That’s like giving a full tank of gas to a scooter and a pickup truck.
Studies show weight-based dosing cuts errors by nearly 40%. A 2023 JAMA Pediatrics study found that parents who used both age and weight instructions reduced mistakes by over half. Why? Because kids metabolize medicine based on how much they weigh-not how old they look.
For acetaminophen (Tylenol), the correct dose is 10-15 mg per kg of body weight every 4-6 hours. No more than 75 mg per kg in 24 hours. For ibuprofen (Advil, Motrin), it’s 5-10 mg per kg every 6-8 hours, max 40 mg per kg per day.
Let’s say your child weighs 22 pounds. That’s 10 kg (22 ÷ 2.2 = 10). For acetaminophen (160 mg/5 mL), that’s 100-150 mg total. That equals 3.1-4.7 mL. You round up to 5 mL to be safe. But if you only looked at the age chart and saw "2-3 years: 5 mL," you’d get the same number. That’s fine in this case. But if your child weighed 15 kg (33 lbs), you’d need 7.5-11.25 mL. The age chart might still say "5 mL"-but that’s dangerously low.
How to Measure Liquid Medicine Correctly
Never use a kitchen spoon. Not even the "measuring" spoon in your drawer. A tablespoon is 15 mL. A teaspoon is 5 mL. But household spoons? They vary wildly. A 2019 FDA study found 68% of dosing errors came from using spoons.
Use the tool that came with the medicine: an oral syringe. It’s the only way to measure accurately. For infants, use a syringe marked in 0.1 mL increments. For older kids, 0.5 mL works. Hold the syringe at eye level. Look at the bottom of the curve in the liquid-the meniscus. If you look from above, you’ll see less than you have. From below, you’ll think you have more. Both cause errors.
Here’s what to do:
- Draw the exact amount into the syringe.
- Hold it steady at eye level.
- Give it slowly into the side of the mouth, not straight down the throat.
- Wipe the syringe clean after use. Store it in a clean, dry place.
Some pharmacies will even mark the syringe with a dot or line for your child’s exact dose. Ask for it. It’s free.
Common Mistakes That Put Kids at Risk
Parents make the same mistakes over and over. Here are the top five:
- Confusing infant drops with children’s liquid: Infant drops used to be 80 mg/1 mL. Now, all children’s liquid is 160 mg/5 mL. That’s the same concentration. But many parents still think infant drops are stronger and use less. That’s wrong. If you’re using a product labeled "Children’s Tylenol," it’s 160 mg/5 mL. Use the same dose whether you call it "infant" or "children’s." The FDA mandated this standard in 2011 to prevent errors.
- Misreading decimals: "1.25 mL" looks like "12.5 mL" if you rush. Always read slowly. Write it down if you need to.
- Using "tsp" and "tbsp" without knowing what they mean: "tsp" = teaspoon = 5 mL. "tbsp" = tablespoon = 15 mL. One tablespoon is three times a teaspoon. Giving "1 tbsp" when it says "1 tsp" is a 300% overdose.
- Combining medicines: Cold medicines often contain acetaminophen. So does Tylenol. Giving both? You’re doubling the dose. Always check the active ingredient before mixing.
- Not checking the expiration date: Expired medicine doesn’t work. Worse, it can break down into harmful chemicals.
What to Do Before Giving Any Medicine
Use this five-step checklist every time:
- Confirm the name: Is it your child’s name on the prescription? Is the medicine labeled correctly?
- Check the dose: Use weight, not age. Calculate it. Use a calculator if needed.
- Verify the unit: Is it mg? mL? tsp? Don’t guess.
- Use the right tool: Syringe, not spoon. No exceptions.
- Double-check expiration: If it’s expired, throw it out and get a new bottle.
And if you’re unsure? Call your pharmacist. They’re trained for this. A 2023 survey found 93% of pharmacists offer free counseling for pediatric prescriptions. Take 5 minutes. Ask: "Is this the right dose for my child’s weight?"
Tools and Resources to Help You
You don’t have to do this alone. Free, trusted tools exist:
- HealthyChildren.org (from the American Academy of Pediatrics): Has printable dosing charts and a weight-based calculator.
- FDA’s "Medicine: Play It Safe" toolkit: Downloadable guides and videos on reading labels.
- KnowYourDose.org: Interactive quizzes to test your understanding.
- CDC’s Medication Safety Checklist: A printable one-pager to hang on your fridge.
There’s also a free app from the AAP called "Safe Dosage Calculator." It lets you enter your child’s weight and automatically calculates the right dose for acetaminophen, ibuprofen, and more. Download it now. It takes 30 seconds.

Special Cases: Infants Under 2 Years
If your child is under 2, don’t give any medicine without talking to a doctor first. Their liver and kidneys aren’t fully developed. They process drugs slower. Even the "right" dose can be too much. The AAP says all medications for babies under 2 require professional guidance. That includes teething gels, cough syrups, and even children’s Tylenol. Call your pediatrician. Don’t rely on the label.
What’s Changing in 2025
The FDA now requires every OTC children’s medicine to include both weight and age dosing by December 31, 2024. That means labels will be clearer. But you still need to read them. Some companies are testing QR codes on bottles that link to video instructions. Smart bottle caps that record when medicine is given are in testing. These will help. But they won’t replace your attention.
Final Reminder: You’re the Most Important Safety Device
Technology can help. Apps can guide. Pharmacists can advise. But only you can check the label, measure the dose, and say "no" when something doesn’t feel right. If the label seems confusing, if the dose feels off, if you’re unsure-stop. Call your doctor. Call the pharmacy. Wait. Don’t guess. One moment of caution can prevent a lifetime of regret.



Comments
14 Comments
Adrienne Dagg
I literally cried reading this. 🥹 My 3-year-old had a fever last winter and I used a teaspoon because the syringe was lost. I didn’t even know the difference between infant drops and children’s liquid. This post saved my life. Thank you.
Erica Vest
The FDA’s 2011 standardization of acetaminophen concentrations (160 mg/5 mL) was a critical public health win. Prior to this, the 80 mg/mL infant drops and 160 mg/5 mL children’s formulations coexisted, leading to catastrophic dosing errors. Always verify concentration-not just product name. The weight-based calculation formula is: (weight in kg) × (10–15 mg/kg for acetaminophen) ÷ concentration (mg/mL). For example: 10 kg × 15 mg/kg = 150 mg; 150 mg ÷ 32 mg/mL (160 mg/5 mL = 32 mg/mL) = 4.7 mL. Round up to 5 mL. Never guess.
Chris Davidson
People need to stop treating medicine like a guessing game. If you cant read a label you shouldnt be parenting. Simple. The syringe thing is non negotiable. Kitchen spoons are for cooking not dosing. End of story
Kinnaird Lynsey
I appreciate the effort put into this. Really. But can we talk about how the phrase "you’re the most important safety device" makes me feel like a failed robot? I’m not a machine. I’m a tired human who just wants my kid to feel better. Sometimes I use a spoon because I’m holding a screaming toddler and the syringe is buried under laundry. No one tells you that part.
Andrew Kelly
This whole thing is a corporate scam. The FDA doesn’t care about your kid. They care about lawsuits. That’s why they forced the concentration standardization-so companies wouldn’t get sued for overdoses. Meanwhile, they’re still letting phthalates and propylene glycol into kids’ meds. And don’t get me started on the QR codes. That’s just surveillance disguised as safety. You think they’re helping? They’re tracking you.
Isabel Rábago
I used to think I was careful. Then I gave my daughter ibuprofen because she had a fever and I thought, "it’s just a little extra." I didn’t know 40 mg/kg/day was the max. She got sick. Not the fever kind. The liver kind. I didn’t know. I thought I was being helpful. Now I measure everything. Twice. And I cry every time I open the cabinet. Don’t be like me.
Anna Sedervay
One must observe that the proliferation of OTC pediatric pharmaceuticals represents a profound epistemological crisis in contemporary domestic healthcare governance. The conflation of pharmacokinetic variables with heuristic age-based guidelines constitutes a systemic failure of evidence-based practice, wherein lay caregivers are coerced into assuming the epistemic authority of clinical pharmacologists without adequate pedagogical infrastructure. One is compelled to inquire: Is the burden of molecular arithmetic truly a maternal obligation?
Jedidiah Massey
Let’s be real - if you’re still using a syringe, you’re doing it wrong. The real pro move? Use a graduated dropper with a calibrated tip. It’s more precise, less messy, and gives you that satisfying *click* when you depress the plunger. Also, if you’re not using a digital scale to weigh your kid every time, you’re just winging it. I’ve got a 2.5kg infant. I weigh her before every dose. You should too. 🧪
Alex Curran
I’m from Australia and we have the same issues here. The labels are just as bad. I didn’t know until last year that "tsp" meant 5mL and not "a spoonful". My niece got too much because her mum used a dessert spoon. I printed the CDC checklist and taped it to our fridge. Best thing I ever did.
Lynsey Tyson
I used to think I was bad at this until I realized everyone else is just pretending they know what they’re doing. I’ve asked pharmacists three times now. They don’t judge. They just give you the syringe and say "here, sweetie, this one’s for your little one." I cried. Then I bought three extra syringes.
Edington Renwick
I don’t know why people are acting like this is new information. I’ve been doing this since 2012. I’ve got spreadsheets. I’ve got color-coded syringes. I’ve got a laminated chart taped to the medicine cabinet. And I’ve got a kid who’s never been to the ER for meds. So if you’re still using spoons? You’re not just careless. You’re reckless. And frankly, it’s embarrassing.
Kitt Eliz
YESSSSS THIS IS THE MOST IMPORTANT POST I’VE SEEN ALL YEAR 🙌🙌🙌 I JUST BOUGHT THE AAP SAFE DOSAGE CALCULATOR APP AND IT’S A GAME CHANGER. I’M TELLING EVERY MOM I KNOW. MY 18-MONTH-OLD IS NOW ON A 100% SYRINGE-ONLY POLICY AND I’M NOT APOLOGIZING. 🩹💉 #ParentingWin #NoMoreSpoons
Dikshita Mehta
In India, many parents rely on local pharmacies for advice, and not all pharmacists are trained in pediatric dosing. I’ve seen people give adult doses to children because the label says "for children" and they assume it’s safe. This guide should be translated and shared in every community clinic. Knowledge saves lives.
Adrienne Dagg
I just used the app and it told me to give 4.2 mL for my 12kg kid. I was about to round up to 5mL like always… but then I remembered your comment about the meniscus. So I measured exactly. Took a deep breath. Gave it. She slept through the night. I’m never going back to guessing. 🤍
Write a comment