Why Your Psoriasis Flares Up When Nothing Seems to Change
If you have psoriasis, you know the frustration: one day your skin is calm, the next it’s red, itchy, and covered in plaques - and you didn’t change your lotion, didn’t eat anything unusual, and didn’t get hurt. What happened?
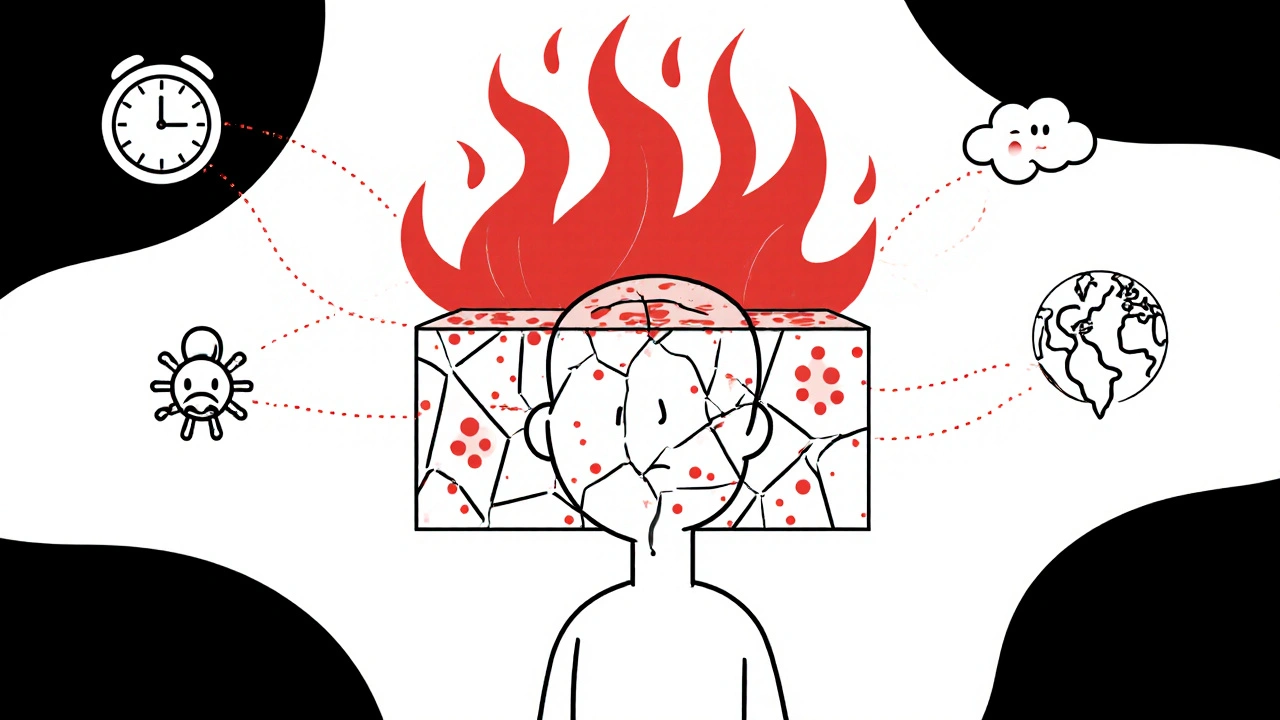
The truth is, psoriasis doesn’t flare randomly. It reacts. And the three biggest triggers hiding in plain sight are stress, infection, and a broken skin barrier. These aren’t just annoyances - they’re biological switches that turn on your immune system’s attack on your own skin.
Think of your skin like a wall. Normally, it keeps bad stuff out and moisture in. But when that wall cracks - from dryness, scratching, or a bug bite - your immune system sees it as an invasion. That’s when the real trouble starts. And stress? It doesn’t just make you feel overwhelmed. It literally rewires your immune response. Even infections you think are "just a cold" can spark a full-blown flare.
Understanding these triggers isn’t about blame. It’s about control. You can’t change your genes. But you can change how you respond to these three forces. And that makes all the difference.
Stress: The Silent Flame That Ignites Psoriasis
Stress doesn’t just make you feel tired. It sets off a chemical chain reaction in your body that directly fuels psoriasis.
When you’re under stress - whether it’s from grief, work pressure, or even a big life change like moving or starting a new job - your body releases cortisol and other inflammatory chemicals. These don’t just affect your mood. They activate immune cells called T-cells and dendritic cells that pump out IL-17 and IL-23, the exact cytokines that drive psoriasis plaques.
Studies show that 60-70% of people with psoriasis report stress as their top flare trigger. One patient on Reddit shared that after losing her mother, her plaques spread from small patches to covering 30% of her body in just three months. That’s not coincidence. It’s biology.
And here’s the cruel twist: psoriasis itself causes stress. The itch, the embarrassment, the constant management - it all piles up. That creates a loop: stress triggers flares, flares cause more stress, and the cycle keeps spinning.
Breaking that loop doesn’t mean eliminating all stress. It means building buffers. Research shows that 20 minutes of daily mindfulness meditation can lower cortisol by 25% in eight weeks. Regular walking, yoga, or therapy aren’t luxuries - they’re part of your treatment plan. Patients who practiced stress-reduction techniques saw at least a 30% drop in flare frequency within six months.
Infections: When Your Body’s Defense System Turns Against Itself
Strep throat. A bad cold. Even the flu. These aren’t just temporary illnesses - they can trigger psoriasis flares, especially in children and young adults.
The connection is strongest with streptococcal infections. When your body fights strep bacteria, it produces antibodies that sometimes mistake your skin cells for the invaders. This is called guttate psoriasis - small, drop-like spots that spread quickly after an infection. It’s not rare. In fact, up to 25% of childhood psoriasis cases start this way.
But it’s not just strep. Viruses like the common cold or even COVID-19 can also trigger flares. How? Your immune system has sensors - like RIG-I - that detect viruses. When activated, they signal immune cells to release IL-23, which kicks off the psoriasis cascade in people with the right genetic background.
Even HIV, which destroys immune cells, can worsen psoriasis - a paradox that still puzzles doctors. It shows how complex this disease is. Your immune system doesn’t just get stronger or weaker. It gets confused.
That’s why prevention matters. Get your flu shot. Wash your hands. Avoid close contact with sick people during cold and flu season. One study found that seasonal flu vaccination reduced infection-triggered flares by 35% in psoriasis patients. That’s not a small win. It’s a game-changer.
And if you do get sick? Don’t panic. Treat the infection early. Keep your skin moisturized. And talk to your doctor. Sometimes, a short course of gentle topical treatment can stop a flare before it spreads.

How a Broken Skin Barrier Turns Minor Irritations Into Major Flares
Your skin isn’t just a covering - it’s a living shield. It holds in moisture, blocks germs, and keeps your immune system calm. When that shield breaks, psoriasis follows.
This is called the Koebner phenomenon. Any skin injury - a sunburn, a bug bite, a scratch, even a tattoo - can cause a psoriasis patch to form right at the spot. That’s not just bad luck. It’s your immune system overreacting to damage.
Research shows that even tiny injuries go unnoticed. One dermatology practice tracked 200 patients and found that 45% of new plaques started at sites of minor trauma - like an unnoticed insect bite or a friction rub from a tight collar. People often don’t remember the injury because it was so small.
But the damage isn’t just physical. Dry air, harsh soaps, and hot showers strip away your skin’s natural oils and proteins. That’s when the real problem begins. A damaged barrier lets bacteria in, which triggers inflammation. At the same time, moisture escapes, making skin crack and itch - which leads to more scratching, more damage, and more flares.
The fix isn’t complicated, but it’s consistent:
- Use fragrance-free moisturizers with ceramides at least twice a day - morning and night. Ceramides are the glue that holds skin cells together.
- Avoid soaps with a pH above 5.5. Most bar soaps are around 9-10. That’s like pouring battery acid on your skin. Use gentle, acidic cleansers instead.
- Keep indoor humidity between 40-60%. A simple humidifier can cut dryness-related flares by half.
- Don’t scratch. Use a cold compress or a gentle tap instead. Scratching isn’t just annoying - it’s a trigger.
One study on mice with damaged skin showed that applying topical antibiotics reduced psoriasis-like inflammation by blocking the bacterial response. That’s why keeping your skin clean and intact isn’t just about comfort - it’s about stopping the flare before it starts.
What You Can Do Today to Reduce Flares
You don’t need to overhaul your life. Small, consistent changes make the biggest difference.
Start with these three actions:
- Protect your skin barrier: Apply a ceramide-rich moisturizer right after showering, while your skin is still damp. Do this every single day - no exceptions.
- Manage stress daily: Set a 10-minute alarm for deep breathing or a short walk. Do it before lunch, not when you’re overwhelmed. Consistency beats intensity.
- Prevent infections: Wash your hands for 20 seconds with plain soap. Get your flu shot. Avoid sharing towels or razors.
Track your flares for two weeks. Write down what you did, how you felt, and what happened. You might be surprised. Maybe your worst flare came after a sleepless night and a cold. Or maybe it followed a sunburn you didn’t think was serious.
Pattern recognition is power. Once you see your triggers, you can plan around them.

What Doesn’t Work - And Why
There’s a lot of noise out there. “Cut out dairy.” “Try this miracle oil.” “Just relax more.”
Some of it helps - but not for everyone. A 2022 survey of over 1,200 psoriasis patients found that 32% thought dairy triggered flares, 25% blamed gluten, and 18% pointed to nightshades. But when tested in controlled studies, eliminating these foods didn’t consistently improve psoriasis. That doesn’t mean they’re harmless - just that they’re not universal triggers.
Same with “just relax.” Stress isn’t the root cause. It’s a fuel. You can’t fix psoriasis by thinking happy thoughts. You need to manage the biological response - through sleep, movement, skin care, and medical treatment.
And don’t wait for a flare to act. Prevention is easier than treatment. If you wait until your skin is burning and cracked, you’re already behind.
What’s Next for Psoriasis Treatment
The science is moving fast. New biologic drugs target IL-23, the key immune signal behind psoriasis flares. In clinical trials, 89% of patients using one of these drugs saw 90% or more improvement in their skin within four months.
Researchers are also looking at the gut-skin connection. Early data shows probiotics can reduce flare frequency by 22% in people with gut microbiome imbalances.
And in the next five years, wearable stress monitors and AI apps that track your symptoms, sleep, and skin condition will become standard. These tools will help you predict flares before they happen - not just react to them.
But no matter how advanced the medicine gets, the basics won’t change: protect your skin, manage stress, avoid infections. These are the pillars. Everything else builds on them.
Can stress cause psoriasis or just make it worse?
Stress doesn’t cause psoriasis by itself - you need the right genes. But it can trigger your first flare if you’re genetically prone. For people who already have psoriasis, stress is one of the most common reasons flares get worse. It activates immune cells that attack the skin, making plaques grow faster and itch more.
Do I need to avoid all infections to prevent psoriasis flares?
No - you don’t need to live in a bubble. But you should take smart steps: wash your hands often, get vaccinated (especially for flu and pneumonia), and treat infections early. Streptococcal throat infections are the biggest known trigger, so if you have a persistent sore throat, see a doctor. Don’t wait for a flare to happen.
What moisturizer ingredients should I look for?
Look for ceramides, hyaluronic acid, glycerin, and fatty acids. Avoid products with alcohol, fragrance, or sulfates. Ceramides are especially important - they rebuild the skin’s natural barrier. Apply moisturizer within 3 minutes after bathing to lock in moisture.
Can weather affect my psoriasis?
Yes. Cold, dry air is a major trigger - it dries out your skin and weakens the barrier. About 68% of people with psoriasis say their symptoms worsen in winter. Hot, humid weather helps most people, but 8% have photosensitive psoriasis that gets worse in the sun. Use sunscreen and keep skin moisturized year-round.
Is there a way to predict when my next flare will happen?
Not perfectly - yet. But many people notice patterns: flares after stress, illness, or dry skin. Start tracking your symptoms, sleep, stress levels, and skin care routine for two weeks. You’ll likely see your personal triggers. In the next few years, apps and wearables will help predict flares using this data - but right now, awareness is your best tool.
Final Thought: You’re Not Fighting Your Skin - You’re Supporting It
Psoriasis isn’t your fault. You didn’t cause it. But you can learn how to calm it down.
Stress, infection, and skin damage aren’t enemies to eliminate. They’re signals to pay attention to. When you protect your barrier, manage your stress, and prevent infections, you’re not just treating psoriasis - you’re giving your body the environment it needs to heal.
It’s not about perfection. It’s about consistency. One moisturized morning. One deep breath. One handwashing. One small choice - repeated every day - is how you take back control.



Comments
14 Comments
Justin Daniel
I used to think psoriasis was just "dry skin" until I saw my cousin go from zero to full-body plaques after his dad died. Stress isn't just in your head-it's in your skin. This post nailed it.
Melvina Zelee
ok but like… i’ve been using ceramides for 3 months and my skin still looks like a map of mars. why is it so hard to just *fix* this? i’m not lazy, i’m just tired.
steve o'connor
I’m from Ireland and we don’t have much sun here, so winter is brutal. I swear by humidifiers and moisturizing right after the shower. No magic, just consistency. Also, avoid the cheap soap at the gas station. Trust me.
ann smith
This is so important. 🌱 Small steps > perfection. I started with just 5 minutes of breathing before bed-and now I don’t reach for the steroid cream as often. You’ve got this. 💪
Julie Pulvino
I used to scratch until I bled. Then I started wearing cotton gloves to bed. It sounds silly, but it broke the itch-scratch cycle. Also, oatmeal baths. Don’t knock it till you try it.
Danny Nicholls
bro i got psoriasis after i got mono in college 😭 i thought it was just a rash but nope. now i wash my hands like i’m in a hospital and i carry ceramide cream everywhere. even to the gym. no shame.
Robin Johnson
If you’re not moisturizing within 3 minutes of getting out of the shower, you’re wasting your time. This isn’t optional. It’s non-negotiable. Do it. Every. Single. Day. No excuses.
Latonya Elarms-Radford
Let me just say… this whole psoriasis thing? It’s not just a skin condition. It’s a metaphysical mirror of your soul’s unresolved trauma. The plaques? They’re your body screaming, "I’m not safe!" The barrier breakdown? That’s your ego crumbling under societal pressure. And stress? Honey, that’s the collective unconscious projecting its anxiety onto your dermis. You’re not broken-you’re awakening. 🌌✨
Mark Williams
The IL-23/Th17 axis is the central driver here. The Koebner phenomenon is a direct result of innate immune activation via DAMPs. Topical ceramides restore lipid lamellae integrity, reducing TLR2/4 signaling. This is why barrier repair is foundational-not cosmetic.
Ravi Kumar Gupta
In India, we have this saying: 'Jab daudh raha hai, tab khaana kha le'-when the fire is burning, eat first. Psoriasis flare? Moisturize. Stress? Breathe. Infection? Wash hands. Don’t wait for the perfect moment. Just start. Simple. No drama.
Rahul Kanakarajan
So you’re telling me I have to wash my hands and moisturize? What, no miracle tea? No 14-day detox? This is why people don’t trust doctors. If it’s that simple, why isn’t it on TV?
New Yorkers
I live in Manhattan. My skin’s been dry since 2017. I don’t have time for 'ceramides' or 'mindfulness.' I have a meeting at 9. My skin’s on fire. What’s the quick fix? Tell me the truth.
David Cunningham
Used to think it was just me being weird. Then I met another bloke with plaques at a BBQ. We didn’t even talk about it. Just nodded. That’s the club you don’t want to join.
luke young
This post made me feel less alone. Thanks for writing it. I’m going to start the 10-minute walk thing tomorrow. No pressure. Just one day at a time.
Write a comment