Ever taken a pill and wondered if it really worked because you ate right after? Or maybe you skipped a meal to follow the label, but still felt off? You’re not alone. Millions of people take medications every day without realizing that what’s on their plate can make the difference between a drug working perfectly or not working at all. The truth is, food-drug interactions aren’t just a footnote on the bottle-they’re a core part of how your body absorbs medicine.
Why Food Changes How Medicines Work
Your digestive system doesn’t just break down food-it also decides how much of your medicine actually gets into your bloodstream. When you eat, your stomach slows down. Gastric emptying, the process that moves things from your stomach to your small intestine (where most drugs are absorbed), can drop by 30% to 50%. That delay changes everything. For some drugs, this delay is harmless. But for others, it can mean your medicine takes twice as long to kick in-or worse, your body absorbs barely half of it. High-fat meals make this even worse. A meal with 50-60 grams of fat can stretch out gastric emptying by 1.5 to 2 hours. That’s why acetaminophen, a common painkiller, reaches peak levels in 45 minutes on an empty stomach-but takes 90 to 120 minutes after a fatty meal. Then there’s solubility. Some drugs dissolve better in fat. Griseofulvin, an antifungal, sees its absorption jump by 200% to 300% when taken with a high-fat meal because bile from the liver helps it dissolve. On the flip side, tetracycline antibiotics bind to calcium in dairy products, reducing absorption by 50% to 75%. That’s why you’re told not to take them with milk, yogurt, or cheese.Empty Stomach: What It Really Means
When a label says “take on an empty stomach,” it doesn’t mean “don’t eat breakfast.” It means: no food for at least one hour before, and two hours after. This is critical for drugs like levothyroxine, used for thyroid conditions. Food can cut its absorption by 30% to 55%. That’s not a small drop-it’s enough to leave you tired, cold, and still hypothyroid, even if you’re taking the right dose. Mount Elizabeth Hospital’s 2022 guidelines say levothyroxine should be taken with plain water, at least 30 minutes before your first bite of food. Many people think “empty stomach” means “before coffee.” But coffee, even black, can interfere. So can calcium-fortified orange juice, fiber supplements, or antacids. All of them can block absorption. A Reddit user, u/ThyroidWarrior, shared how their recurring UTI didn’t clear up until they stopped taking doxycycline with their morning yogurt. Two hours apart, and the infection vanished. That’s the kind of real-life fix that doesn’t show up in textbooks-it shows up in patient stories.Take With Food: When Eating Helps
Not all drugs hate food. Some need it to work. Nitrofurantoin, an antibiotic for urinary tract infections, absorbs 40% better with food. Cefpodoxime, another antibiotic, sees a 50% to 60% boost in absorption when taken with a meal. Sulfonylureas like glipizide, used for type 2 diabetes, must be taken 30 minutes before eating. If you take them on an empty stomach, your blood sugar can crash below 70 mg/dL-dangerously low. The American Diabetes Association found that 23% of patients on these drugs who skipped meals ended up in the ER with hypoglycemia. Even NSAIDs like ibuprofen benefit from food. While enteric-coated versions are less irritating, regular ibuprofen can cause stomach pain or bleeding. Taking it with food cuts stomach problems from 42% of users down to just 12%, according to a GoodRx survey of 5,000 people. But here’s the catch: not all “with food” means the same thing. For some antiretrovirals, a small snack of 200-300 calories is enough. For others, you need a full meal. Most patients don’t know the difference-and that’s where mistakes happen.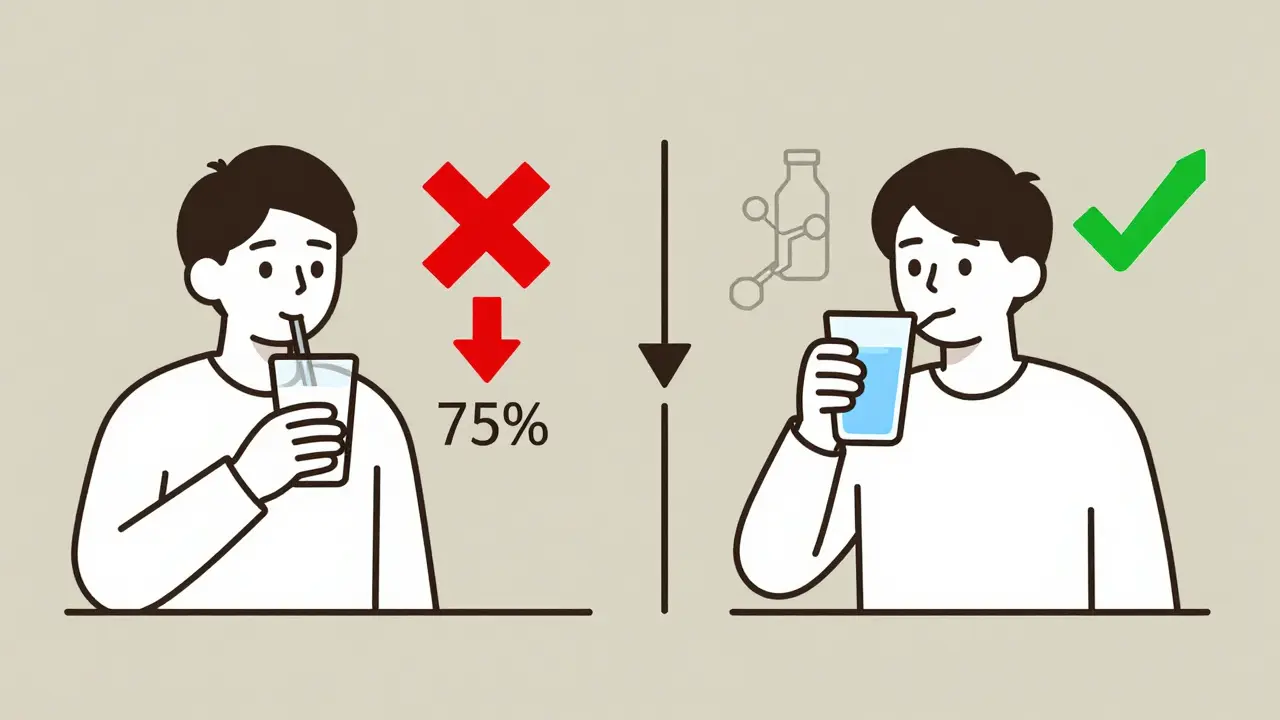
Timing Matters More Than You Think
It’s not just about whether you eat. It’s about when you eat. Semaglutide, a popular weight-loss and diabetes drug, loses 44% of its absorption if taken within 30 minutes of eating. That’s why Novo Nordisk’s clinical trials recommend waiting at least 30 minutes after taking it before you eat. Yet, many patients take it right before breakfast because it’s convenient. The result? Less weight loss, less blood sugar control. Even the time of day matters. New research in Nature Medicine (March 2024) shows that taking certain medications at specific times of day-aligned with your body’s natural rhythms-can boost effectiveness by up to 30%. Combine that with food timing, and you’re not just improving absorption-you’re optimizing your whole treatment.What the Experts Say
The Australian Prescriber (2023) points out that for most chronic medications, a slight delay in absorption doesn’t matter-as long as the total amount absorbed stays the same. But for others, like thyroid meds or antibiotics, timing is non-negotiable. The Mayo Clinic’s 2022 consensus, signed by 12 pharmacology experts, says: “Timing matters significantly for about 25% of commonly prescribed drugs.” That’s one in four. And the FDA confirms that 35% of new drugs approved between 2015 and 2022 came with specific food-effect instructions. Even the advice on NSAIDs is mixed. myDr.com.au says take them with food to protect your stomach. The American College of Gastroenterology says enteric-coated versions don’t need it. This confusion is why patients get it wrong-and why pharmacists are so important.Real People, Real Mistakes
On Drugs.com, 62% of users taking levothyroxine admit they struggle with the empty stomach rule. Nearly 30% say they still feel symptoms-even though they’re taking their pill “correctly.” Why? Because they had coffee, a multivitamin, or a bowl of oatmeal within an hour of taking it. Express Scripts’ 2023 report found that 45% of patients misunderstand “take with food.” Some think it means a full three-course meal. Others think it means “as long as you ate today.” But for drugs like atazanavir (an HIV medication), you only need a snack of 200-300 calories. Too little, and absorption drops. Too much, and it’s delayed. The most dangerous error? Taking diabetes pills on an empty stomach. It’s not just inconvenient-it’s life-threatening. And it’s common.
How to Get It Right
Here’s how to avoid the most common mistakes:- For empty stomach meds: Take them first thing in the morning, with a full glass of water. Wait 60 minutes before eating or drinking anything else. Set a phone alarm if you need to.
- For meds that need food: Take them with a regular meal-not a snack, unless specified. Consistency matters more than perfection.
- For calcium or iron blockers: Avoid dairy, antacids, or supplements within two hours of tetracycline, ciprofloxacin, or levothyroxine.
- For high-fat meals: Don’t assume they help. They delay absorption for some drugs and boost it for others. Check your label.
- Use apps: Medisafe and MyTherapy now have food-timing reminders. Users who turn them on see 27% fewer timing errors.
When in Doubt, Ask Your Pharmacist
Pharmacists are your best resource. A 2022 study by the American Pharmacists Association found that patients who got specific food-timing advice when they first started a new medication had 35% higher adherence after 90 days. Don’t just read the label. Ask: “Should I take this before, with, or after food? And what counts as food?” Even small changes-like moving your pill from 7:30 a.m. to 7:00 a.m., or swapping your yogurt for a banana-can make your treatment work better.The Bigger Picture
Food-drug interactions cost the U.S. healthcare system an estimated $300 billion a year. About 8% of that-$24 billion-is tied to improper timing with meals. That’s not just money. It’s hospital visits, failed treatments, and avoidable suffering. As people age and take more medications-by 2030, over half of adults over 65 will be on five or more drugs-this problem will only grow. New tools are emerging: ingestible sensors that track gastric pH, breath tests to measure how fast your stomach empties, and digital health systems that sync with your calendar to remind you when to eat and when to take your pill. But the simplest tool is still the most powerful: knowing your medicine. Not just the name. Not just the dose. But when and how to take it. Your body doesn’t just process medicine-it processes it alongside your food. And that’s not a coincidence. It’s biology. Pay attention to it.Can I take my medication with coffee or juice?
It depends on the drug. Coffee can interfere with thyroid meds like levothyroxine and some antibiotics. Calcium-fortified orange juice blocks absorption of tetracycline and other antibiotics. Even grapefruit juice can dangerously increase levels of certain blood pressure and cholesterol drugs. When in doubt, take your medication with plain water.
What if I forget to take my pill on an empty stomach?
If you realize within an hour of eating, wait until your stomach is empty again-usually two hours after your last bite-then take it. If it’s been longer than that, skip the dose and take your next one at the regular time. Don’t double up unless your doctor says to. For most drugs, missing one dose won’t ruin your treatment, but taking it with food regularly can.
Does it matter if I eat a big meal vs. a small snack?
Yes. For drugs that need food to absorb better (like some antifungals or HIV meds), a small snack of 200-300 calories is often enough. But for others, like certain antibiotics, a full meal is required. High-fat meals delay gastric emptying, which can slow absorption for some drugs. Always check the label or ask your pharmacist what kind of food is recommended.
Why do some drugs need to be taken with food and others don’t?
It comes down to chemistry. Drugs that are fat-soluble (like griseofulvin) absorb better with fat. Drugs that are sensitive to stomach acid (like itraconazole) need an acidic environment, which food can reduce. Others, like NSAIDs, irritate the stomach lining-food acts as a buffer. And some, like levothyroxine, are easily blocked by minerals in food. Each drug has its own rules based on how it’s made and how your body handles it.
Are there any apps that help me remember when to take my meds with food?
Yes. Apps like Medisafe and MyTherapy let you set reminders for both medication timing and meals. Users who activate food-timing features see a 27% drop in missed or incorrectly timed doses. Some even sync with your calendar to remind you to eat before taking your pill-or wait after.
If you’re on more than three medications, keep a simple list: drug name, dose, and whether to take it before, with, or after food. Carry it with you. Show it to your pharmacist every time you refill. It’s not extra work-it’s your safety.



Comments
12 Comments
Arlene Mathison
OMG I just realized I’ve been taking my levothyroxine with my morning coffee for YEARS 😳 I switched to water and waited 45 mins-my energy is already better. Why isn’t this taught in med school??
Emily Leigh
So… you’re telling me food isn’t just ‘background noise’ for pills? Like, shocker. Next you’ll say breathing affects oxygen absorption. 🙄
Carolyn Rose Meszaros
This is SO helpful!! 🙌 I’ve been taking my antibiotics with yogurt because ‘it’s good for gut health’… now I know why I kept getting sick. Going to print this out and tape it to my pill organizer. 💊❤️
Greg Robertson
Good stuff. I’ve been taking my ibuprofen with peanut butter toast for years-never had a stomach ache. Just makes sense to me. Always thought food was a buffer, but didn’t know the science behind it.
Renee Stringer
People need to stop treating their bodies like vending machines. If you can’t follow basic instructions on a pill bottle, maybe you shouldn’t be taking pills at all.
Crystal August
Another ‘science’ article that blames patients for not being perfect. What about people who work two jobs and can’t wait two hours after eating to take their meds? This isn’t a lifestyle blog-it’s real life.
Nadia Watson
Thank you for this comprehensive overview. As a long-term caregiver for elderly patients on polypharmacy, I’ve witnessed firsthand the consequences of mis-timed dosing. The 35% adherence increase with pharmacist guidance is not surprising-clear, consistent communication is the cornerstone of safe medication use. Please encourage patients to ask pharmacists, not Google. 🙏
Courtney Carra
It’s funny how we treat our bodies like machines with input/output protocols… but then we ignore the fact that we’re biological systems shaped by evolution. Maybe the real issue isn’t food-drug interactions-it’s that we’ve detached from our own biology. 🤔
thomas wall
One cannot help but observe the alarming negligence exhibited by the general populace in adhering to pharmaceutical guidelines. The $24 billion annual cost is not merely a fiscal concern-it is a moral failure of public health literacy. This is not a suggestion. It is a demand for accountability.
Shane McGriff
Just had a patient come in last week who was taking doxycycline with her protein shake-she had a full-blown UTI because of it. I showed her this article and she cried. We need more of this. Not just info-actionable, compassionate, clear guidance. Pharmacist advice isn’t a luxury-it’s a lifeline.
Jacob Cathro
bro i took my glipizide with a donut once and passed out. now i know why. also, why is everyone so shocked that food affects drugs? like… it’s called digestion. we’re not robots. also, why is this 10 pages long? 🤡
Paul Barnes
Correction: The FDA states that 35% of new drugs approved between 2015 and 2022 had food-effect labeling-not that they were ‘designed’ with it in mind. Precision matters.
Write a comment