INR Elevation Calculator
Warfarin & Antibiotic Interaction Calculator
This tool estimates how certain antibiotics may affect your INR while taking warfarin. Remember: INR values above 4.0 increase bleeding risk significantly.
Result
When you’re on warfarin, even a simple antibiotic can turn dangerous. Trimethoprim-sulfamethoxazole - commonly sold as Bactrim or Septra - is one of the most common antibiotics prescribed for urinary tract infections, bronchitis, and sinus infections. But if you’re taking warfarin for atrial fibrillation, a mechanical heart valve, or deep vein thrombosis, this combo can spike your INR dangerously high - and put you at risk for internal bleeding you won’t see coming.
Why This Interaction Is So Dangerous
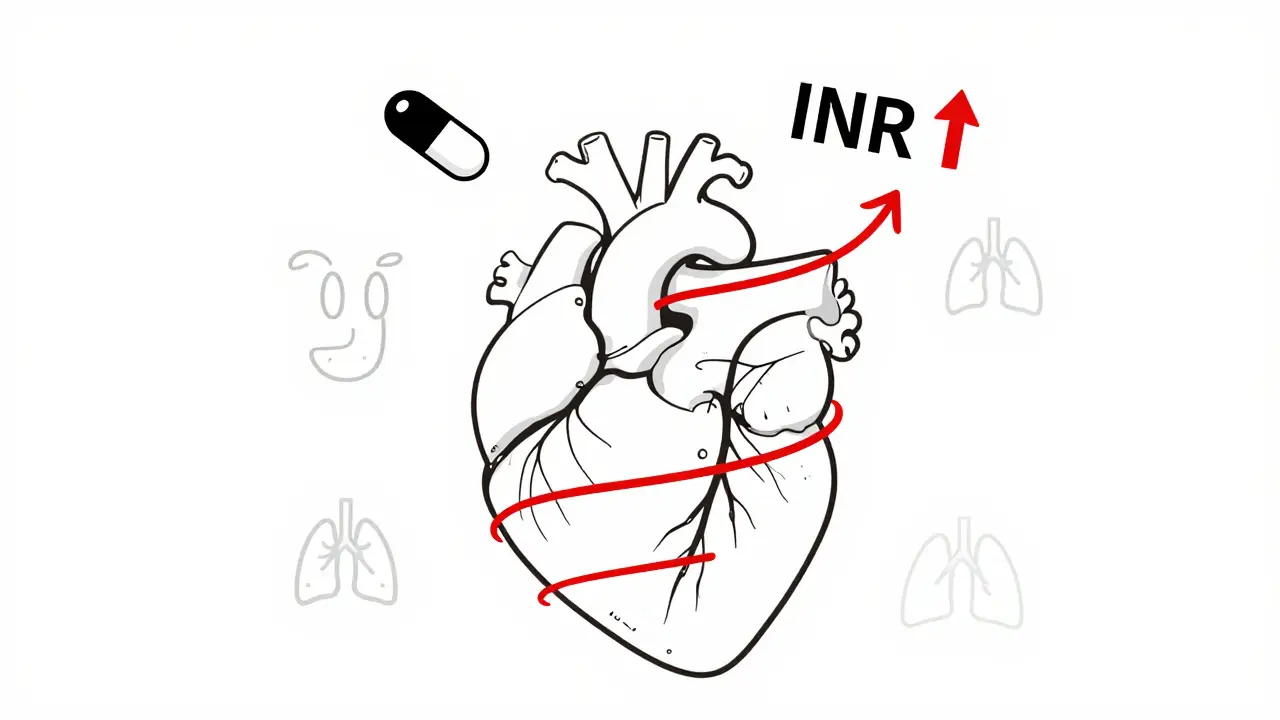
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a narrow therapeutic drug - meaning the difference between a safe dose and a dangerous one is small. Your INR (International Normalized Ratio) tells doctors how long it takes your blood to clot. For most people on warfarin, the target is between 2.0 and 3.0. Go above 4.0, and your bleeding risk starts climbing fast. Above 5.0? That’s a red zone. Trimethoprim-sulfamethoxazole doesn’t just interfere with warfarin - it attacks it from multiple angles. First, it displaces warfarin from proteins in your blood. Warfarin is 97-99% bound to albumin, so even a small shift can send more free warfarin circulating, making it more active. Second, trimethoprim blocks the CYP2C9 enzyme, the main pathway your liver uses to break down the most powerful form of warfarin (S-warfarin). That means warfarin builds up in your system. Third, sulfamethoxazole can kill off gut bacteria that make vitamin K. Less vitamin K? Warfarin works even harder. The result? INR jumps. Studies show an average increase of 1.8 units within 36 to 72 hours of starting TMP-SMX. That’s not a small blip. If your INR was 2.8, it could hit 4.6 - no warning, no symptoms, just a silent climb toward bleeding.Real Cases, Real Consequences
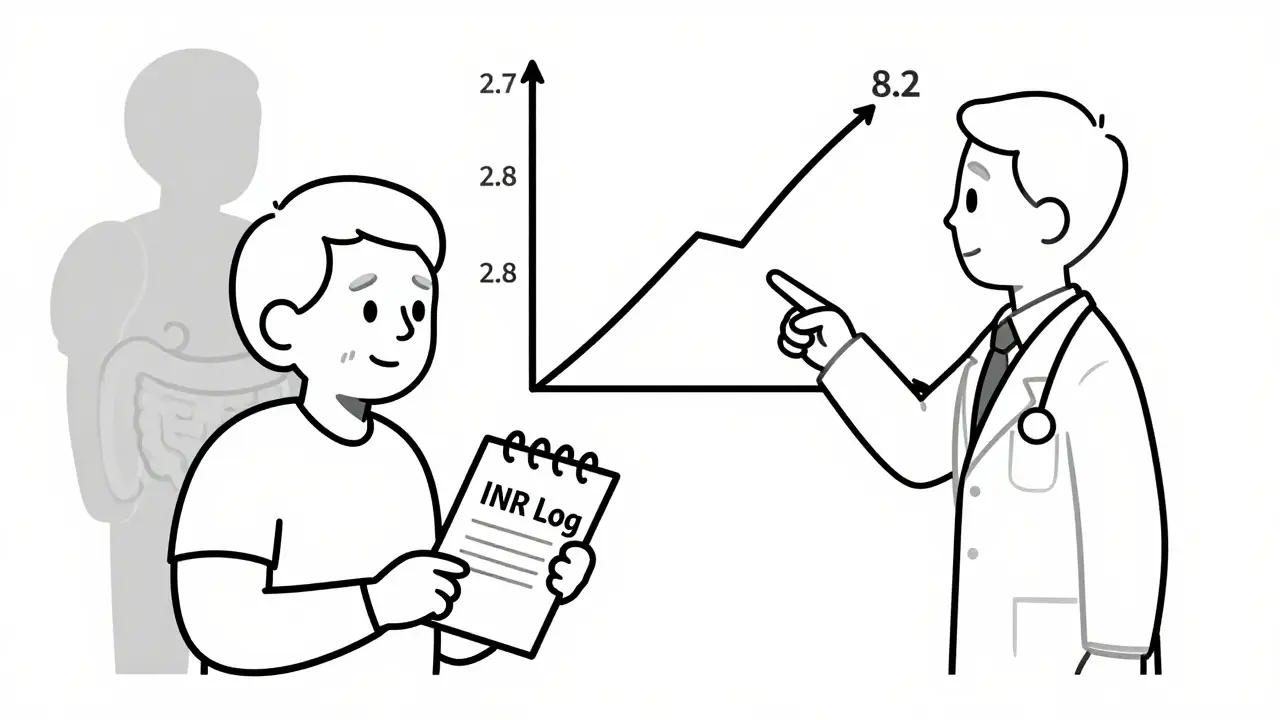
A 78-year-old man with a mechanical aortic valve was prescribed Bactrim for a suspected UTI. His INR was stable at 2.6. Three days later, it shot to 8.2. He developed bruising, blood in his urine, and dizziness. He ended up in the ER needing vitamin K and fresh frozen plasma. He survived - but barely. That’s not rare. FDA data from 2018 to 2023 shows over 1,800 reports of INR elevation linked to TMP-SMX. Nearly half led to hospitalization. Almost 4% - 68 cases - were fatal. These aren’t outliers. They’re predictable. On patient forums, stories repeat: a grandmother on warfarin for AFib, given Bactrim for a bladder infection, ends up in the ER with a GI bleed. A 65-year-old man with a history of DVT, on a steady warfarin dose for years, takes Bactrim for pneumonia - and wakes up with black, tarry stools. His INR? 9.1. These aren’t mistakes. They’re consequences of a well-documented interaction that still happens far too often.Not All Antibiotics Are the Same
If you need an antibiotic while on warfarin, not all options are equally risky. TMP-SMX is one of the worst. Here’s how it stacks up:| Antibiotic | Average INR Increase | Risk Level |
|---|---|---|
| Trimethoprim-Sulfamethoxazole | 1.8 units | High |
| Ciprofloxacin | 0.9 units | Moderate |
| Amoxicillin | 0.4 units | Low |
| Nitrofurantoin | 0.2 units | Low |
| Metronidazole | 1.2 units | Moderate-High |
Who’s at Highest Risk?
Not everyone on warfarin who takes TMP-SMX will have a spike. But some people are far more vulnerable:- People over 75 - their livers clear drugs slower
- Those with heart failure - reduced blood flow affects drug metabolism
- Patients with poor nutrition or liver disease - less vitamin K, less enzyme activity
- Men - studies show males are 9% more likely to experience dangerous INR rises than women
- Those with CYP2C9 gene variants - slower metabolizers are at higher risk
What Doctors Should Do
If a patient on warfarin needs an antibiotic, here’s the protocol:- Check INR before starting TMP-SMX
- Reduce warfarin dose by 20-30% preemptively - especially in high-risk patients
- Check INR again within 48-72 hours of starting the antibiotic
- Check every 3-4 days while on therapy
- Switch to a safer antibiotic if possible - nitrofurantoin for UTIs, amoxicillin for sinus or lung infections
What Patients Should Do
You’re not powerless. If you’re on warfarin:- Always tell every doctor, pharmacist, and ER staff you’re on warfarin - even if it’s for a cold
- Ask: “Is this antibiotic safe with warfarin?” If they say “probably,” push back. Say: “I’ve heard Bactrim can raise my INR. Is there another option?”
- Know your baseline INR. Keep a log - even a simple notebook helps
- Watch for signs of bleeding: unusual bruising, nosebleeds, pink or red urine, dark stools, headaches, dizziness
- Get your INR checked sooner if you start any new medication - even OTC
What About Newer Blood Thinners?
DOACs - like apixaban, rivaroxaban, dabigatran - don’t interact with TMP-SMX the same way. That’s why they’ve replaced warfarin for many patients. But not everyone can use them. People with mechanical heart valves still need warfarin. Those with severe kidney disease may not qualify for DOACs. Older adults on multiple meds may still be on warfarin because it’s cheaper, or because their doctor isn’t familiar with the newer options. In 2022, over 2.6 million Americans were still prescribed warfarin. And TMP-SMX remains one of the top 50 most prescribed antibiotics in the U.S. That means this interaction isn’t fading - it’s still a daily risk in clinics and hospitals.The Bottom Line
Trimethoprim-sulfamethoxazole and warfarin don’t mix. Not safely. Not reliably. Not even for a few days. This isn’t a theoretical concern. It’s a real, documented, preventable danger that kills people every year. Whether you’re a patient or a provider, don’t assume “it’ll be fine.” Check the INR. Switch the antibiotic. Use vitamin K if needed. Don’t wait for bleeding to start. There are safer options. Use them.Can I take Bactrim if I’m on warfarin?
Bactrim (trimethoprim-sulfamethoxazole) should be avoided if possible when taking warfarin. It can cause your INR to spike dangerously high, increasing your risk of serious or fatal bleeding. If no other antibiotic works for your infection, your doctor may prescribe it - but only after checking your INR before and within 48 hours of starting it, reducing your warfarin dose, and monitoring you closely.
How quickly does INR rise after taking Bactrim?
INR typically starts rising within 24 to 36 hours after starting Bactrim, with the peak effect occurring between 48 and 72 hours. This is why it’s critical to check your INR within 48 hours of beginning the antibiotic - waiting longer could mean missing the warning signs before bleeding starts.
What antibiotics are safe with warfarin?
Amoxicillin and nitrofurantoin are generally considered low-risk for warfarin interactions. Azithromycin and penicillin are also safer options. Ciprofloxacin and metronidazole can raise INR moderately and should be used with caution. Always confirm with your doctor or pharmacist before starting any new antibiotic.
What should I do if my INR goes above 5.0?
If your INR is above 5.0 and you have no bleeding, your doctor may recommend skipping 1-2 warfarin doses and giving you 1-2.5 mg of oral vitamin K. If your INR is above 10.0 or you’re bleeding (bruising, blood in urine, black stools, headache), you need immediate medical care - IV vitamin K and 4-factor prothrombin complex concentrate may be required. Never wait to treat a high INR.
Why do some people not have an INR spike with Bactrim?
Everyone’s body handles drugs differently. Genetics, liver function, diet, age, and other medications all play a role. Some people have faster CYP2C9 enzyme activity, meaning they break down warfarin more quickly. Others have more vitamin K from their diet or gut bacteria. That’s why some patients can take Bactrim without issue - but you can’t assume you’re one of them. Always assume risk until proven otherwise.



Comments
8 Comments
Alexandra Enns
Oh please, another alarmist post about Bactrim. I’ve been on warfarin for 12 years and took Bactrim three times-no issues. Your INR didn’t spike because you didn’t monitor it. Stop scaring people with cherry-picked FDA data. Canada’s got better healthcare than your panic-driven US clinics, and we don’t treat every antibiotic like a death sentence.
Marie-Pier D.
Thank you for writing this. 💙 I’m a nurse in Ontario and I’ve seen too many elderly patients end up in the ER because their GP prescribed Bactrim without checking INR. One lady, 81, with a mechanical mitral valve-got Bactrim for a UTI, INR hit 9.2, woke up with a subdural hematoma. She’s fine now, but barely. Please, if you’re on warfarin, tell every provider-even the pharmacist-before they write anything. You’re not being difficult, you’re being smart. 🙏
Shelby Marcel
wait so bactrim = bad? but i just got it for my sinus thing and im on warfarin… is it too late?? my inr was 2.4 last week… i hope i dont die lmao
blackbelt security
It’s not about fear. It’s about protocol. If you’re on warfarin, you’re already managing a high-risk condition. Adding an antibiotic that’s known to interfere isn’t a gamble-it’s negligence. The data’s clear. The guidelines exist. Follow them. Your life isn’t a demo.
venkatesh karumanchi
This is so important! I’m from India and we don’t have easy access to DOACs here-warfarin is all most people can afford. But doctors here still prescribe Bactrim like it’s water. I’ve told my uncle to always ask for amoxicillin instead. He’s 76, on warfarin for AFib, and he’s still here because he listened. Knowledge is power, folks. Share this with your family.
Jenna Allison
Let me break this down simply: TMP-SMX = CYP2C9 inhibition + protein displacement + gut flora disruption = triple threat to warfarin clearance. INR spikes aren’t random-they’re pharmacokinetic inevitabilities. For patients: if your doc says "it’s fine," ask for the evidence. For providers: if you’re prescribing Bactrim to someone on warfarin without a 48-hour INR check, you’re not practicing medicine-you’re gambling. Nitrofurantoin for UTIs, amoxicillin for sinusitis-these are low-risk, high-reward choices. Stop the unnecessary risk.
Darren Links
Yeah, but what if you’re in rural Texas and the only pharmacy that has antibiotics in stock is the one that only carries Bactrim? You think the ER docs are sitting around reading journals? They’re triaging 12 patients at once. This post is great for the 1% who have access to specialists. For the rest of us? It’s just guilt-tripping people who are already stressed.
Kevin Waters
Great breakdown. I’m a pharmacist in Ohio and I see this every week. I always ask patients: "Are you on warfarin?" If they say yes, I say: "Let me check if we can swap this for amoxicillin or azithromycin-it’s safer, and your doctor will thank you." Most don’t even know to ask. If you’re reading this and you’re on warfarin, carry a card in your wallet that says: "I take warfarin. Do not prescribe Bactrim or metronidazole." It’s saved me from 3 near-misses this year alone. Small steps save lives.
Write a comment