When you take a pill to stop frequent bathroom trips, ease Parkinson’s tremors, or help you sleep, you might not think about what it’s doing to your brain. But for millions of older adults using common medications like oxybutynin, diphenhydramine, or amitriptyline, the hidden cost could be memory loss, confusion, and even faster brain shrinkage. These drugs belong to a class called anticholinergics, and while they work well for their intended purposes, their side effects are far more serious than most people realize.
What Are Anticholinergics and How Do They Work?
Anticholinergics block acetylcholine, a chemical messenger in your body that helps control muscle movement, heart rate, digestion, and memory. These drugs were developed over a century ago, starting with atropine from the deadly nightshade plant. Today, they’re used for overactive bladder, Parkinson’s, allergies, depression, and even motion sickness.
But here’s the catch: acetylcholine isn’t just about muscles. It’s critical for thinking and remembering. When you block it in the brain-especially over months or years-you’re not just treating a symptom. You’re slowly turning down the volume on your own cognitive function.
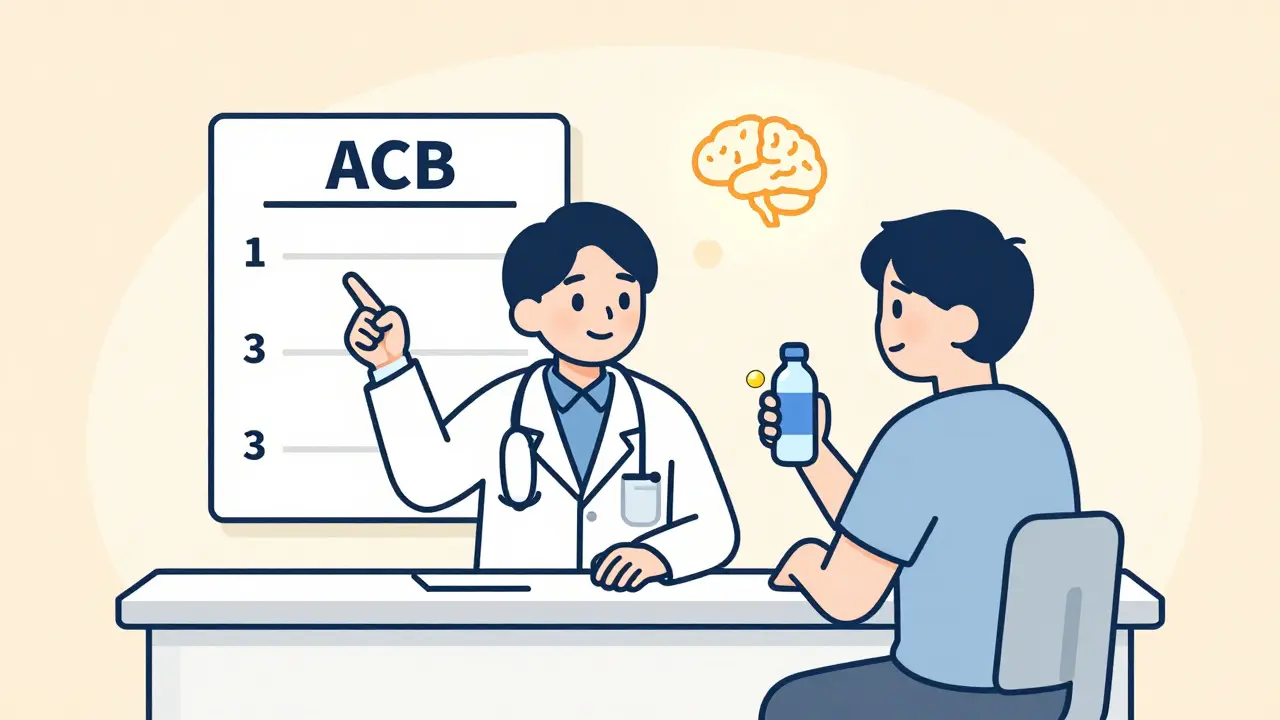
Doctors use something called the Anticholinergic Cognitive Burden (ACB) scale to rate how strong this effect is. A score of 0 means no effect. A score of 3 means high risk. Drugs like scopolamine and diphenhydramine (Benadryl) hit a 3. Oxybutynin? It’s a 2 or 3. But others like tolterodine or glycopyrrolate? They’re only a 1-and even those carry some risk if used long-term.
The Brain Changes No One Talks About
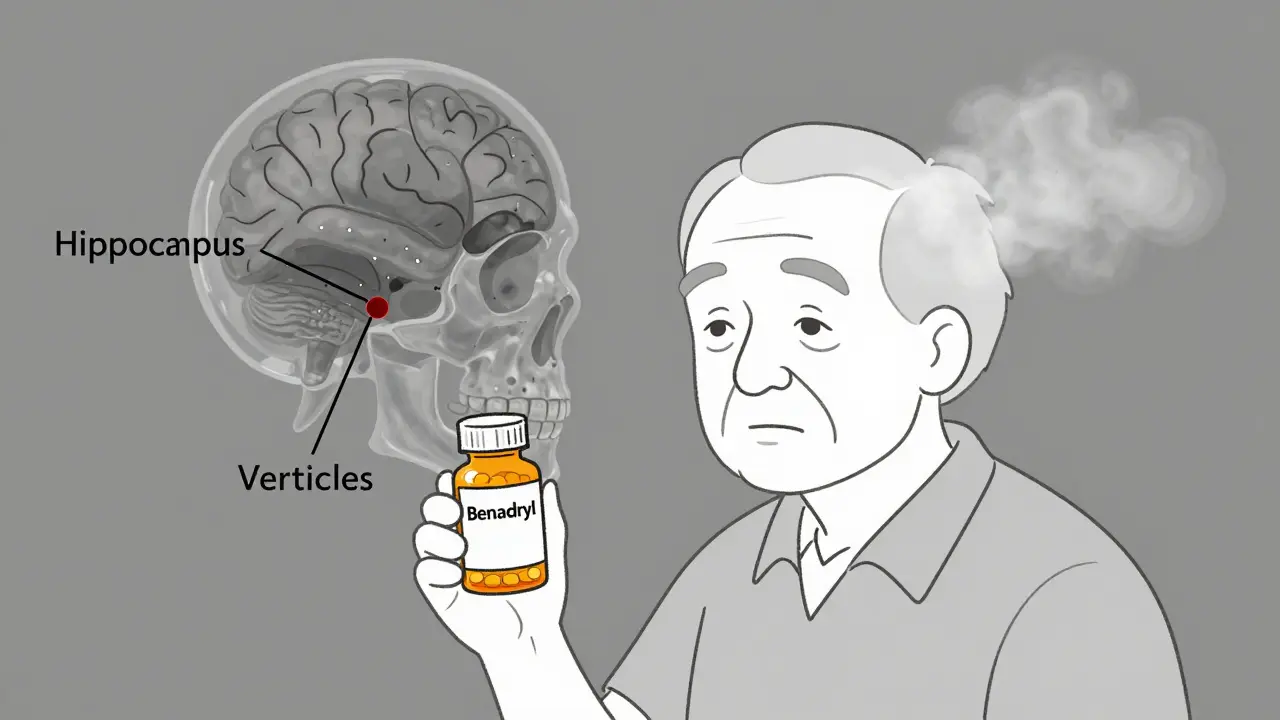
It’s not just about feeling foggy. Brain scans show real, measurable damage. A 2016 study in JAMA Neurology followed 451 older adults over several years. Those taking high-ACB medications lost 0.5% to 1.2% more brain tissue each year than those who didn’t. That’s not a little bit. That’s the equivalent of aging your brain 2-3 extra years in just five years.
Glucose metabolism-the brain’s fuel-dropped by 8-14% in the hippocampus, the area responsible for forming new memories. Ventricles, the fluid-filled spaces in the brain, grew 10-15% larger. That’s not normal aging. That’s brain shrinkage.
Memory tests showed users performed 23-32% worse on immediate recall tasks. Executive function-planning, organizing, switching tasks-was 18-27% slower. And it got worse with every extra point on the ACB scale. Each additional point meant 0.3% more brain shrinkage per year.
Dr. Shannon Risacher, who led that study, said it clearly: “These findings provide us with a much better understanding of how this class of drugs may act upon the brain in ways that might raise the risk of cognitive impairment and dementia.”
Who’s Most at Risk?
It’s not just the elderly. But they’re the most vulnerable. About 20-30% of older adults in the U.S. are on at least one anticholinergic drug. Many don’t even realize they’re taking one. Diphenhydramine is in sleep aids, allergy pills, and even some cold medicines. Amitriptyline is prescribed for nerve pain, depression, and migraines. Oxybutynin is common for bladder control.
And the damage adds up. A 2015 study in the BMJ tracked over 48,000 people. Those who took high-ACB drugs for three or more years had double the risk of developing dementia. The American Geriatrics Society updated its Beers Criteria in 2023 to list 56 medications as “potentially inappropriate” for seniors. That includes diphenhydramine, oxybutynin, and amitriptyline. They don’t just warn against them-they say: avoid them if you can.
Dry Mouth Is Just the Tip of the Iceberg
Everyone knows about dry mouth. It’s the most common side effect. Eighty-two percent of users on Drugs.com complain about it. One Reddit user wrote, “I drink 3 liters of water a day and still feel like my throat is sandpaper.” Another said, “I can’t talk without clearing my throat every 10 seconds.”
But dry mouth isn’t just annoying. It’s a sign something deeper is happening. Saliva isn’t just for comfort-it protects your teeth, helps you swallow, and even starts digestion. Chronic dry mouth increases risk of cavities, gum disease, and swallowing problems.
And it’s not just the mouth. Anticholinergics can cause constipation, urinary retention, blurred vision, and even overheating because your body can’t sweat properly. For older adults, these aren’t minor inconveniences. They can lead to falls, hospitalizations, and worse.
Not All Anticholinergics Are Created Equal
Here’s the good news: not every drug in this class is equally dangerous. The difference between oxybutynin and tolterodine isn’t just marketing-it’s brain health.
Compare these:
| Drug | ACB Score | Common Use | Cognitive Risk |
|---|---|---|---|
| Scopolamine | 3 | Motion sickness | Very High |
| Diphenhydramine (Benadryl) | 3 | Allergies, sleep | Very High |
| Oxybutynin | 2-3 | Overactive bladder | High |
| Amitriptyline | 3 | Depression, nerve pain | Very High |
| Tolterodine | 1-2 | Overactive bladder | Moderate |
| Glycopyrrolate | 1 | Peptic ulcers, excessive sweating | Low |
| Trospium | 1 | Overactive bladder | Low |
| Mirabegron | 0 | Overactive bladder | None |
Notice something? Mirabegron-a beta-3 agonist-has no anticholinergic activity. It works just as well as oxybutynin for bladder control, without touching your brain. A 2017 NEJM trial showed it was equally effective. But because it costs $350 a month versus $15 for generic oxybutynin, doctors rarely prescribe it.
And then there’s trospium. A 2023 study found it has 70% less penetration into the brain than oxybutynin. That’s why it’s now called a “cognitive-sparing” option. It’s not perfect-but it’s a big step forward.
What Should You Do?
If you or a loved one is on one of these drugs, don’t panic. But do ask questions.
Start with this:
- Ask your doctor: “What’s the ACB score of this medication?”
- Ask: “Is there a non-anticholinergic alternative?”
- Ask: “Can we try a lower dose or shorter duration?”
- Ask: “Should we monitor my memory with a MoCA test every 6 months?”
For overactive bladder, behavioral therapy-like timed bathroom trips or pelvic floor exercises-is just as effective as drugs for many people. And it has zero cognitive risk.
If you’re on diphenhydramine for sleep, try melatonin, better sleep hygiene, or even a low-dose trazodone. If you’re on amitriptyline for nerve pain, ask about gabapentin or duloxetine. There are options.
And if you’re stuck with an anticholinergic? Manage the dry mouth. Sugar-free gum can boost saliva by 30-40%. Prescription sprays like Xerolube help. Pilocarpine (5mg three times a day) increases saliva by over 50%. Talk to your pharmacist. These aren’t luxury items-they’re essential.
Why Isn’t This Common Knowledge?
Here’s the uncomfortable truth: doctors don’t always know. A 2020 study in JAMA Internal Medicine found only 32% of primary care doctors could correctly identify high-ACB drugs from a list. Most patients don’t know their meds carry this risk. Pharmacies don’t warn them. Insurance companies push the cheapest option.
But change is coming. The FDA updated labels in 2022 to include stronger dementia warnings. The UK’s NICE now recommends deprescribing anticholinergics in 68% of long-term users over 65. Medicare prescriptions for oxybutynin dropped 32% from 2015 to 2022. Mirabegron prescriptions jumped from 1.8 million to 7.3 million in the same period.
AI tools like MedAware are now screening prescriptions in real time, flagging risky combinations. One study predicts this could prevent 200,000-300,000 dementia cases in the U.S. over five years.
Final Thoughts
Anticholinergics aren’t evil drugs. They’ve helped millions. But we’ve ignored their long-term cost for too long. Cognitive decline doesn’t happen overnight. It creeps in slowly-like forgetting where you put your keys, struggling to find words, or losing focus mid-sentence. By the time it’s obvious, the damage is done.
Don’t wait for a diagnosis. Ask for alternatives. Ask for testing. Ask for a plan. Your brain doesn’t ask for much-but it deserves better than a cheap pill with a hidden price tag.
Can anticholinergics cause dementia?
Yes, long-term use of high-ACB anticholinergics (score 2-3) is linked to a doubled risk of dementia after three or more years of use, according to a 2015 BMJ study of 48,000 patients. Brain imaging shows structural changes like hippocampal shrinkage and increased ventricular volume, which are early signs of neurodegeneration. The American Geriatrics Society now lists several anticholinergics as potentially inappropriate for older adults due to this risk.
Which anticholinergic drugs are safest for the brain?
Drugs with an ACB score of 1 or lower carry much lower risk. These include glycopyrrolate, trospium, tolterodine, darifenacin, fesoterodine, tiotropium, and ipratropium. Among bladder medications, mirabegron has no anticholinergic activity and is considered the safest alternative. Always check the ACB score before starting or continuing a medication.
Is dry mouth from anticholinergics dangerous?
Yes. Chronic dry mouth increases risk of tooth decay, gum disease, difficulty swallowing, and even aspiration pneumonia. It’s also a red flag that the drug is affecting your nervous system system-wide. Management includes sugar-free gum, prescription saliva substitutes like Xerolube, or pilocarpine-which can increase saliva flow by 50-70%. Ignoring it can lead to serious health complications.
Can I stop taking anticholinergics cold turkey?
No. Abruptly stopping anticholinergics-especially for Parkinson’s or severe depression-can cause dangerous rebound symptoms like worsening tremors, hallucinations, or withdrawal seizures. Always work with your doctor to taper slowly. For bladder medications, switching to mirabegron or behavioral therapy is often safer than quitting cold turkey.
Are there new drugs that avoid these side effects?
Yes. Newer drugs like trospium chloride XR have 70% less brain penetration than older options like oxybutynin. Researchers are also developing M1 receptor-selective agents that target only the brain areas needed for treatment, avoiding peripheral side effects. Karuna Therapeutics’ xanomeline, currently in Phase III trials, reduces dry mouth by 40% compared to traditional antipsychotics. AI-driven prescribing tools are also being rolled out to flag risky combinations before they’re written.
How can I check if my medication is anticholinergic?
Use the Anticholinergic Cognitive Burden (ACB) scale. Many hospitals and pharmacies now have online tools or apps that let you enter your medication and get an ACB score. You can also ask your pharmacist or doctor directly. Common high-risk drugs include Benadryl, oxybutynin, amitriptyline, and scopolamine. Lower-risk options include glycopyrrolate, tolterodine, and mirabegron.
Next steps: If you’re on an anticholinergic, request your ACB score. Ask about alternatives. Schedule a cognitive check-up with your doctor. Your memory isn’t something you can afford to gamble with.