When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version-and you expect it to be safe. But what happens after that pill hits the market? The FDA doesn’t just approve generics and walk away. It keeps watching-closely, continuously, and with advanced tools most people never hear about.
Why Post-Approval Monitoring Matters
Generic drugs make up 90% of all prescriptions filled in the U.S. They save patients and the healthcare system billions every year. But here’s the catch: before approval, generic drugs are tested in small groups-usually 24 to 36 healthy adults. That’s enough to prove they deliver the same amount of active ingredient as the brand-name drug. But it’s not enough to catch rare side effects, long-term risks, or reactions in people with multiple health conditions.The FDA admits it: it’s impossible to have complete safety information at the time of approval. The real picture emerges only after thousands, sometimes millions, of people take the drug in real life. That’s why post-approval monitoring isn’t optional-it’s essential.
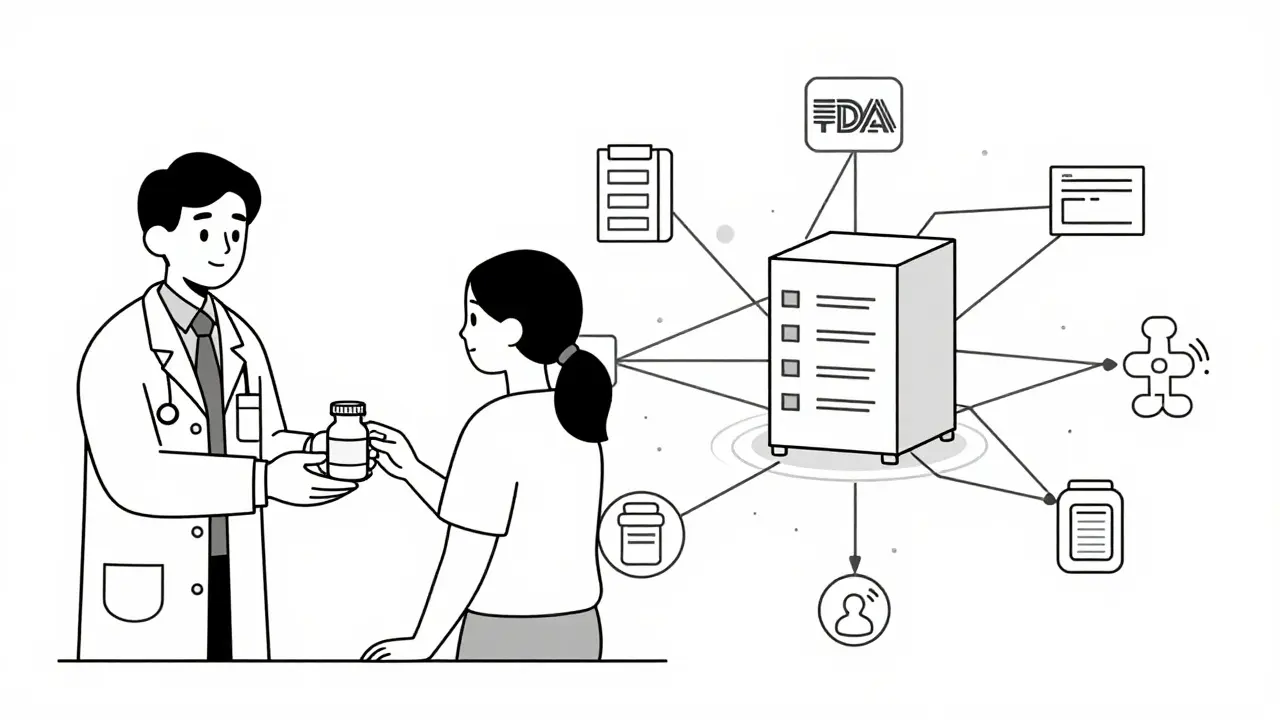
How the FDA Tracks Problems After Approval
The FDA doesn’t rely on guesswork. It uses a network of systems that collect, analyze, and act on safety data from across the country.The main tool is the FDA Adverse Event Reporting System (FAERS). Every year, it collects about 2 million reports of side effects, allergic reactions, or unexpected outcomes. These come from doctors, pharmacists, patients, and drugmakers themselves. When a spike in reports shows up-for example, a sudden rise in liver problems linked to a specific generic blood pressure med-the FDA digs in.
Behind the scenes, a team of epidemiologists, pharmacologists, and physicians in the Office of Generic Drugs reviews these signals. They don’t just look at the numbers. They check patient histories, compare the generic to the brand-name version, and look for patterns tied to specific manufacturers or batches.
The Sentinel Initiative: Real-Time Surveillance
One of the biggest leaps in safety monitoring came with the Sentinel Initiative. Launched in 2008 and expanded under the 21st Century Cures Act, Sentinel taps into electronic health records from over 100 million Americans. That’s not just reports-it’s actual medical data from hospitals, clinics, and insurers.Imagine this: a generic statin is approved. Within weeks, Sentinel notices that patients taking this version have a slightly higher rate of muscle pain than those on the brand-name version. Even if no one filed a formal report, the system flags it. That’s real-time surveillance. It catches problems before they become epidemics.
Manufacturing Isn’t Just About Ingredients-It’s About Safety
A generic drug isn’t just the active ingredient. It also has fillers, coatings, and binders-called inactive ingredients. These don’t treat your condition, but they can affect how the drug is absorbed or trigger reactions in sensitive people.The FDA’s Office of Pharmaceutical Quality (OPQ) inspects over 1,800 drug manufacturing sites every year-1,200 in the U.S. and 600 overseas. These aren’t scheduled visits. Many are unannounced. Inspectors check everything: how raw materials are stored, whether equipment is clean, if lab tests are accurate.
One recent case involved a generic version of a diabetes drug. After reports of inconsistent blood sugar control, an inspection found the manufacturer had changed the coating without notifying the FDA. The coating altered how quickly the drug dissolved. The product was pulled from shelves.
What Happens When Something Goes Wrong?
When the FDA finds a safety issue, it doesn’t wait. It acts fast.- If a batch is contaminated, the company is ordered to recall it.
- If a side effect is confirmed but not life-threatening, the FDA requires a label update-adding a warning about dizziness or liver risk, for example.
- In rare cases, if the risks outweigh the benefits, the drug is pulled from the market entirely.
Since 2012, over 30 generic drugs have been subject to label changes due to post-approval safety findings. None have been withdrawn for safety reasons alone-but several were recalled for manufacturing defects that could lead to harm.
The Hidden Gaps: Why Some Problems Slip Through
Despite all the tools, the system isn’t perfect.One big problem: underreporting. Experts estimate only 1% to 10% of adverse events are ever reported to the FDA. Most patients don’t know how to report. Doctors are busy. Pharmacies don’t always track.
Another issue: complex generics. Inhalers, injectables, and topical creams are harder to copy exactly. Small differences in how they’re made can change how the drug works in the body. The FDA is improving its methods for these, but monitoring them is still a work in progress.
Also, the system relies heavily on data from the U.S. If a side effect only shows up in older patients with kidney disease-and those patients aren’t well-represented in U.S. databases-it might take years to detect.
Who Pays for All This?
You might think taxpayers foot the bill. They don’t. Since 2012, the Generic Drug User Fee Amendments (GDUFA) require generic manufacturers to pay fees to fund the FDA’s review and monitoring work. In 2023, these fees brought in over $65 million annually.That money pays for staff, software, inspections, and data analysis. It’s not charity-it’s a system where those who profit from selling generics help pay to keep them safe.
What You Can Do
You’re not just a passive patient. You can help keep the system strong.- If you have a strange side effect, report it. Go to MedWatch-it’s free and takes five minutes.
- If you notice your generic pill looks different or seems to work differently, talk to your pharmacist. It might be a new batch or a different manufacturer.
- Keep a simple log: what drug you took, when, and how you felt. That info can be crucial if problems arise.
The FDA doesn’t monitor generics because it distrusts them. It monitors them because it trusts them enough to know they’re used by millions-and because even the safest medicine can have hidden risks once it’s out in the real world.
Generic drugs are one of the most successful public health innovations in modern medicine. But safety doesn’t end at approval. It’s a lifelong job-and the FDA is still on the clock.



Comments
8 Comments
Phil Kemling
It’s wild to think that the same system that approves a pill based on 36 people’s bloodwork is then expected to catch rare side effects in millions. We treat drugs like they’re static objects, but they’re dynamic systems interacting with bodies, lifestyles, diets, genetics. The FDA’s tools are impressive, but they’re still reactive. We’re always chasing the past, never predicting the next hidden risk. Maybe we need to shift from monitoring to modeling-simulating how drugs behave across diverse populations before they’re even released.
Elisha Muwanga
Let’s be real-this whole system is a corporate shell game. Generic manufacturers pay the FDA to monitor themselves. The ‘unannounced inspections’? More like scheduled tours with a warning text. And don’t get me started on how they let foreign factories off the hook. We’re trusting Chinese and Indian labs with our lives while our own workers get laid off. This isn’t safety-it’s cost-cutting with a fancy name.
Catherine Scutt
my pharmacist just switched my generic blood pressure med last month and i swear i felt like i was on a different drug. dizzy, tired, weird heart palpitations. didn’t think to report it till now. thanks for the reminder. i’m filing a medwatch thing right after this comment.
Darren McGuff
People don’t realize how revolutionary Sentinel is. We’re talking about real-time health data from over 100 million Americans-EHRs, insurance claims, lab results-all stitched together with privacy safeguards. This isn’t just passive reporting; it’s predictive surveillance. When a new generic statin causes a subtle spike in rhabdomyolysis cases across 12 states before a single formal report is filed? That’s science working. And it’s happening right now, quietly, without fanfare. We should be celebrating this, not doubting it.
Aron Veldhuizen
You say the FDA ‘trusts’ generics enough to monitor them. That’s not trust-that’s institutional necessity. If they didn’t monitor, they’d be legally liable for every death caused by a contaminated batch. The entire system is built on fear, not faith. And let’s not pretend the user fee model is altruistic-it’s regulatory capture disguised as public-private partnership. The manufacturers fund the watchdog, then lobby to keep the leash long. The only thing that’s truly ‘on the clock’ is the FDA’s credibility.
Heather Wilson
The underreporting issue is not just a statistical gap-it’s a systemic failure of patient education and healthcare infrastructure. Patients don’t report because they’re told ‘it’s probably nothing,’ doctors don’t report because EMRs don’t prompt them, and pharmacies don’t track because they’re paid per script, not per outcome. This isn’t a technical problem. It’s a cultural one. And until we incentivize reporting as a core clinical duty-not an optional extra-we’re just rearranging deck chairs on the Titanic.
Jeffrey Hu
Wait, so the FDA inspects 1,800 sites a year? That’s like 5 per day, every day. Most of those are overseas. Do you really think they can inspect a factory in India thoroughly in a single day? And the ‘unannounced’ visits? I’ve read reports-companies get tipped off via local distributors. They clean up, fake records, and the inspectors leave satisfied. It’s theater. The system looks good on paper, but the reality? It’s a game of Whac-A-Mole with counterfeit pills and unapproved excipients.
Jenci Spradlin
just wanted to say-i work in a pharmacy and we get new generic batches all the time. sometimes the pills look totally different but still have the same name. if you notice your meds feel weird after a refill, ask your doc or pharmacist if it’s the same maker. i’ve seen people get sick from switching to a new batch without knowing. report it. it matters.
Write a comment