Chronic Alcohol Use Disorder isn't just about drinking too much. It’s a medical condition where your brain and body become so dependent on alcohol that stopping feels impossible-even when it’s destroying your health, relationships, and life. This isn’t weakness. It’s biology. And the good news? It’s treatable.
What Happens to Your Body When You Drink Too Much for Too Long
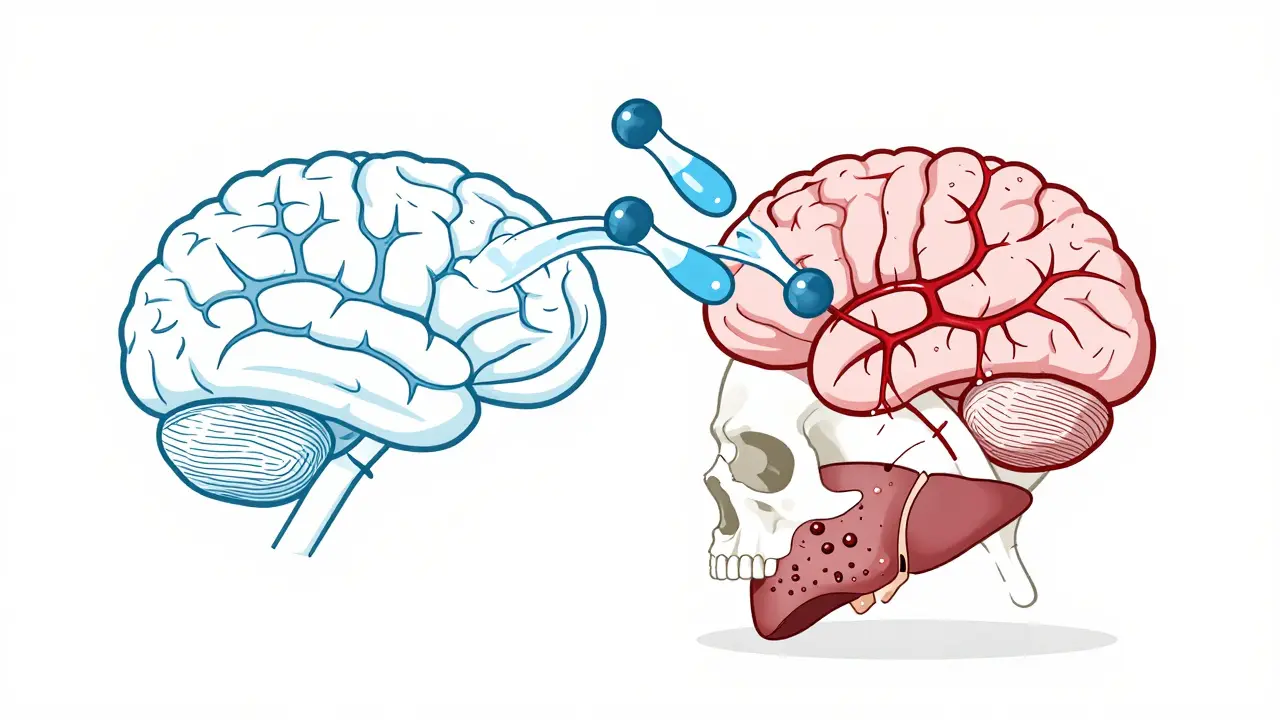
Every time you drink, alcohol hits your brain first. It slows down your nervous system, making you feel relaxed at first. But over time, your brain adapts. You need more alcohol to feel the same effect. That’s tolerance. Then comes dependence: your body starts relying on alcohol just to function normally. Skip a drink, and your system goes into overdrive-shaking, sweating, racing heart, even seizures. This isn’t a bad habit. It’s a neurological rewiring.The liver takes the hardest hit. After years of heavy drinking, 90% of people develop fatty liver. It’s reversible-if you stop drinking. But if you keep going, inflammation sets in. That’s alcoholic hepatitis. Cells die. Scar tissue builds up. Eventually, the liver turns into hard, non-functioning fibrosis-cirrhosis. Once cirrhosis sets in, some damage is permanent. Liver failure becomes a real risk.
It’s not just the liver. Alcohol raises your blood pressure by 16% in heavy drinkers. That means a 34% higher chance of stroke and a 40% higher risk of atrial fibrillation, a dangerous heart rhythm. Your heart muscle weakens. Blood vessels stiffen. You’re more likely to have a heart attack.
Alcohol also wrecks your brain. Long-term use causes memory loss, trouble thinking clearly, and even dementia-like symptoms. Numbness and burning in your hands and feet? That’s nerve damage from vitamin B1 deficiency. Up to 80% of people with severe AUD are deficient. Left untreated, it can lead to Wernicke’s encephalopathy-confusion, loss of coordination, eye movement problems. It’s life-threatening.
And your immune system? It’s broken. Heavy drinkers are 2.7 times more likely to get pneumonia. Your body can’t fight off infections like it used to. You get sick more often. Recovery takes longer.
The Hidden Costs: Mental Health and Social Damage
Alcohol doesn’t just hurt your body-it reshapes your mind. Many people with AUD also struggle with depression or anxiety. It’s not always clear which came first. But the cycle is vicious: you drink to feel better, but alcohol makes depression worse. Over time, your brain’s natural chemicals for happiness and calm get suppressed.Relationships fall apart. Jobs are lost. Finances collapse. People with chronic AUD are more likely to be homeless, unemployed, or in debt. The social isolation that follows makes recovery harder. You stop seeing friends. Family stops trusting you. The shame builds. And the drinking continues.
Alcohol is also linked to cancer. Heavy drinkers have five times the risk of mouth and throat cancer. Breast cancer risk goes up 12% for every drink per day. Liver cancer, bowel cancer-it all climbs with long-term use. The American Cancer Society says alcohol is a known carcinogen. There’s no safe level if you’re drinking daily over years.
How Is Alcohol Use Disorder Diagnosed?
Doctors don’t diagnose AUD based on how many drinks you have per week. They look at behavior. The DSM-5, the standard guide used by mental health professionals, lists 11 criteria. If you meet two or more in a year, you have AUD. The severity depends on how many:- Drinking more or longer than you meant to
- Wanting to cut down but can’t
- Spending a lot of time getting, using, or recovering from alcohol
- Cravings-strong urges to drink
- Drinking interferes with work, school, or family
- Keeping drinking even when it causes relationship problems
- Giving up hobbies or activities because of alcohol
- Using alcohol in dangerous situations-like driving
- Keeping drinking even when it makes you feel depressed or anxious
- Needing more to get the same effect
- Experiencing withdrawal symptoms when you stop
There’s no blood test for AUD. No scan. No X-ray. Diagnosis comes from honest conversation. That’s why so many people go undiagnosed. They don’t recognize the signs. Or they’re too ashamed to talk about it.
Treatment Isn’t One-Size-Fits-All
The first step is detox. If you’ve been drinking heavily for months or years, quitting cold turkey can be deadly. Seizures, hallucinations, delirium tremens-these are real risks. Medically supervised detox in a hospital or clinic keeps you safe. Doctors use medications like benzodiazepines to ease withdrawal symptoms and prevent complications.After detox, recovery begins. Three FDA-approved medications help people stay sober:
- Naltrexone (ReVia, Vivitrol): Blocks the pleasurable effects of alcohol. Reduces cravings.
- Acamprosate (Campral): Helps stabilize brain chemistry after stopping. Eases anxiety and restlessness.
- Disulfiram (Antabuse): Makes you sick if you drink. Nausea, vomiting, pounding heart. It’s a deterrent, not a cure.
Medication alone isn’t enough. Therapy is critical. Cognitive Behavioral Therapy (CBT) works for about 60% of people. It helps you spot triggers-stress, boredom, certain people-and replace drinking with healthier responses. Motivational Enhancement Therapy (MET) helps you find your own reasons to quit. It’s not about being told what to do. It’s about uncovering your own motivation.

Support Groups Work-But Not for Everyone
Alcoholics Anonymous (AA) has helped millions since 1935. The 12-step program gives structure, community, and accountability. Their own data shows 27% of members stay abstinent after one year. But the numbers are self-reported. Some studies question how accurate they are.Not everyone likes AA. Some find the spiritual focus uncomfortable. Others feel judged. That’s okay. There are alternatives:
- SMART Recovery: Science-based, focuses on self-empowerment and cognitive tools.
- Women for Sobriety: Designed for women, addresses emotional and relational triggers.
- LifeRing Secular Recovery: No spiritual elements. Just peer support and personal responsibility.
Group support isn’t mandatory, but it helps. People who attend regularly are more likely to stay sober long-term.
New Treatments Are Changing the Game
Science is catching up. In 2022, a study in JAMA Psychiatry showed transcranial magnetic stimulation (TMS)-a non-invasive brain stimulation technique-led to 50% abstinence rates in heavy drinkers after 12 weeks. It’s not widely available yet, but it’s promising.Digital tools are also helping. The reSET app, approved by the FDA, delivers CBT through your phone. In trials, users were twice as likely to stay sober compared to those getting only standard care. Apps like Sober Grid and Inebriate connect you to real people in recovery 24/7.
And the most powerful combo? Medication + therapy. The MATTERS study found that combining both increased abstinence rates by 24% compared to either alone. That’s huge. Treatment doesn’t have to be all-or-nothing. It can be layered.
Can Your Body Heal?
Yes. And it starts the day you stop.Within days, your liver begins repairing itself. Fatty liver reverses in weeks if you quit. Inflammation from hepatitis drops. Blood pressure starts to normalize. Sleep improves. Mood lifts. Skin clears up. The redness and puffiness on your face? That fades.
Even cirrhosis can stabilize. Some scarring remains, but the liver can still function if you stay sober. The NHS says liver damage from cirrhosis may be reversible-if you stop drinking completely. That’s not a guarantee, but it’s hope.
Brain function improves too. Memory, focus, decision-making-these can recover over months or years. Nerve damage might not fully heal, but pain and numbness often lessen.
Recovery isn’t about perfection. It’s about progress. One day at a time.
Why So Few People Get Help
Only 19.2% of Americans with AUD get treatment. Why? Stigma. Fear. Cost. Lack of access.Many still see AUD as a moral failure-not a medical condition. That’s changing, slowly. But shame keeps people silent. Others can’t afford therapy. Or there’s no provider nearby. In rural areas, treatment options are scarce.
Insurance doesn’t always cover it. Even with the Affordable Care Act, mental health and addiction services are often underfunded. Medications like naltrexone can cost hundreds per month without coverage.
And then there’s the myth: “I can quit anytime.” People believe they’re in control. But AUD rewires the brain. Willpower alone rarely works. That’s why professional help matters.
What to Do If You or Someone You Love Has AUD
If you recognize these signs in yourself or someone else:- Drinking more than intended
- Feeling sick when not drinking
- Ignoring responsibilities because of alcohol
- Trying to quit but failing
Start here:
- Talk to your doctor. Be honest. They’re there to help, not judge.
- Call a helpline. The SAMHSA National Helpline (1-800-662-HELP) is free, confidential, and available 24/7.
- Look into local treatment centers. Many offer sliding scale fees.
- Don’t wait for rock bottom. Recovery works best when you start before things fall apart completely.
You don’t have to do this alone. And you don’t have to be perfect to begin. Just start.
Is alcohol use disorder the same as alcoholism?
Yes. Alcoholism is the older, informal term for what’s now called Alcohol Use Disorder (AUD). The medical community uses AUD because it reflects a spectrum-from mild to severe-rather than labeling someone as an “alcoholic.” It’s a more accurate, less stigmatizing way to describe the condition.
Can you recover from liver damage caused by alcohol?
Yes, if you stop drinking. Fatty liver reverses within weeks. Alcoholic hepatitis can improve significantly. Even early-stage cirrhosis can stabilize. But once scarring becomes advanced, some damage is permanent. The key is stopping before cirrhosis progresses too far. The liver is resilient-but only if you give it a chance.
What’s the most effective treatment for AUD?
The most effective approach combines medication with behavioral therapy. Studies show that using naltrexone or acamprosate along with Cognitive Behavioral Therapy increases abstinence rates by 24% compared to either method alone. Support groups help, but they work best as part of a broader plan-not as the only treatment.
Does quitting alcohol improve mental health?
Absolutely. Many people with AUD also have depression or anxiety. Alcohol worsens both. After 4-8 weeks of sobriety, most report better sleep, clearer thinking, and improved mood. Brain chemistry begins to rebalance. Therapy helps address the root causes of drinking, so mental health improves faster and lasts longer.
How long does it take to feel better after quitting alcohol?
It varies. Withdrawal symptoms peak in 24-72 hours and usually fade within a week. Sleep improves in 1-2 weeks. Energy levels rise in 3-4 weeks. Mood stabilizes around 6-8 weeks. Skin clears up in 4-6 weeks. But full brain and liver recovery can take months or even years. The first 30 days are the hardest-but also the most important.
Are there any new treatments for AUD in 2026?
Yes. Transcranial magnetic stimulation (TMS) is now being tested in clinics for AUD, with 50% abstinence rates in early trials. Digital therapeutics like the reSET app are FDA-approved and widely available. New medications are in Phase 3 trials, including drugs targeting glutamate and dopamine pathways. While not yet mainstream, these options are becoming more accessible through specialized addiction centers.



Comments
10 Comments
Kerry Howarth
Alcohol isn't a vice-it's a neurological hijacking. The fact that we still treat it like a moral failing is why so many people suffer in silence.
Michael Burgess
Bro, I was at 12 drinks a day for 5 years. Liver enzymes were through the roof. Quit cold turkey. 18 months clean. Skin looks like I'm 25 again. Sleep? Like a baby. Brain fog? Gone. It’s not magic. It’s biology resetting. 🙌
Liam Tanner
There’s a lot here, and most of it’s accurate. But I’d add that access to care is still wildly uneven. In rural areas, even if you want help, the nearest detox center might be 200 miles away. And insurance? Good luck getting coverage for acamprosate without a 3-month waiting period.
Palesa Makuru
Oh please. You think AA is the answer? I’ve seen people in those meetings sobbing over their ‘higher power’ while their kids are in foster care. It’s culty, performative, and frankly, a little embarrassing. SMART Recovery is the only thing that treats adults like adults. 🙄
Hank Pannell
The neuroplasticity angle here is fascinating-alcohol doesn’t just impair, it reprograms. The dopaminergic pathways get rewired into dependency loops that mimic Pavlovian conditioning. But here’s the paradox: the same plasticity that creates addiction also enables recovery. The brain isn’t broken-it’s just learned the wrong thing. That’s why CBT + pharmacotherapy works: you’re not fighting biology, you’re redirecting it. And the fact that TMS shows 50% abstinence? That’s not a treatment. That’s a paradigm shift. We’re moving from moral frameworks to neurobiological ones. The stigma? It’s becoming obsolete.
Lori Jackson
Of course you’re ‘recovered’ if you just quit. But what about the people who never even tried? The ones who blame their ‘trauma’ instead of taking responsibility? This post reads like a pep rally for excuses. If you can’t control your drinking, maybe you’re just weak. No amount of science changes that.
Wren Hamley
Went to detox last year. Got naltrexone. Didn’t feel a damn thing. Then I started doing CBT-found out I drank because I was terrified of being alone. No one told me that. The apps? Sober Grid saved my life. Texted someone at 3 a.m. They texted back. That’s the real medicine. Not the pills. Not the meetings. Just someone saying, ‘I’m here.’
Sarah Little
Did you know that 80% of AUD patients are deficient in B1? That’s why they get peripheral neuropathy. Thiamine supplementation should be standard in every detox protocol. It’s not optional. It’s basic neurology. And yet, most outpatient clinics skip it to save money. That’s negligence.
innocent massawe
From Nigeria: I lost my brother to liver failure last year. He drank every day. No one told him it was killing him. He thought it was just ‘stress relief.’ Your post? It’s the kind of thing we need more of. Thank you. 🙏
veronica guillen giles
Wow. So the solution to a disease caused by capitalism, trauma, and loneliness is… more apps and pills? Cute. Meanwhile, the real problem-systemic neglect, poverty, lack of housing-isn’t even mentioned. But hey, at least we can blame the liver.
Write a comment