Handwritten prescriptions are still killing people - and it’s not just a old problem
Imagine you’re a pharmacist. You hold a prescription in your hand. The doctor’s writing? Barely legible. Is that hydrocodone or hydromorphone? Is the dose 5 mg or 50 mg? Is it meant to be taken twice daily or twice weekly? You call the clinic. The doctor’s assistant says, ‘Oh, it’s 5 mg, twice a day.’ But you’re not sure. You’ve done this 12 times this morning. And you’re not the only one.
In the U.S. alone, pharmacists make 150 million calls per year just to clarify handwriting on prescriptions. That’s not inefficiency - that’s a patient safety crisis. And it’s not just pharmacists. Nurses spend an average of 12.7 minutes per illegible prescription tracking down details. Medical students admit they’ve ignored unclear handwriting because they were too rushed. That’s not negligence - it’s a system failure.
Here’s the hard truth: illegible handwriting on prescriptions causes thousands of preventable deaths every year. The Institute of Medicine estimates that 7,000 people die annually in the U.S. alone because of errors tied to poor handwriting. That’s more than traffic accidents in some years. And it’s not just about misreading letters - it’s about missing critical details: wrong dosage, wrong route, wrong patient, no prescriber ID. These aren’t typos. These are life-or-death mistakes.
Why handwritten prescriptions still exist - and why they shouldn’t
It’s 2026. We have self-driving cars, AI that writes poetry, and apps that order groceries with a voice command. But in hospitals and clinics across the world, doctors are still scribbling prescriptions by hand.
Why? Time. Pressure. Habit. A 2017 study found that 68% of medical trainees believed improving their handwriting would take too much time during patient visits. They’re not lazy - they’re overwhelmed. A single doctor might see 30 patients in a day, each needing notes, orders, and follow-ups. Writing legibly takes extra seconds. In a packed schedule, those seconds vanish.
But here’s the catch: those seconds cost lives. A 2005 study in a British hospital found that only 24% of handwritten operative notes were rated as ‘excellent’ or ‘good’ for legibility. Nearly 40% were deemed ‘poor’ by nurses, physiotherapists, and medical officers. That’s not a rare case - it’s standard practice in many places.
Even worse, some healthcare workers admit they just guess. One study found that 22% of medical staff would ignore unclear handwriting rather than take the time to clarify. That’s not a personal failure - it’s a systemic one. When the system rewards speed over safety, people will choose speed. Every time.
Electronic prescribing isn’t just better - it’s dramatically safer
The solution isn’t better pens or handwriting classes. It’s not training doctors to write neater. It’s replacing handwritten prescriptions with electronic ones.
The data doesn’t lie. A 2025 study in JMIR found that 80.8% of electronic prescriptions met all safety criteria. Compare that to just 8.5% for handwritten ones. That’s a 900% improvement. Even manually typed e-prescriptions - ones without templates or auto-fill - were 56% accurate. That’s still more than six times safer than scribbled paper.
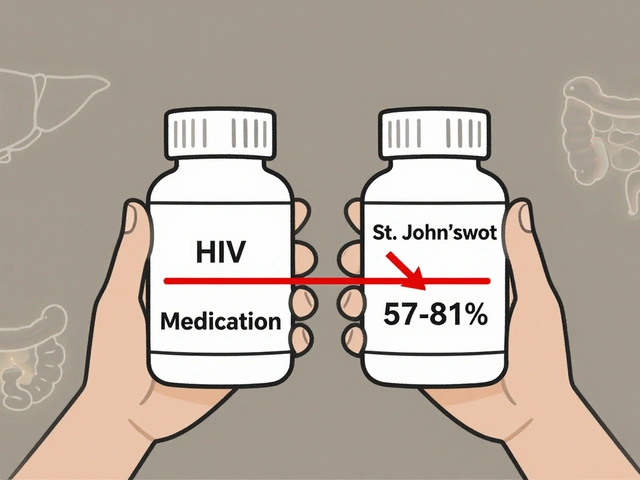
E-prescribing cuts errors from illegibility by 97%. No more guessing if ‘S’ is ‘5’ or ‘S’ is ‘S’. No more confusion between ‘q.d.’ (once daily) and ‘q.i.d.’ (four times daily). The system auto-fills the drug name, dosage, frequency, route, and prescriber info. It flags dangerous interactions. It blocks duplicate orders. It tells you if the patient is allergic.
Dr. Cheryl Reifsnyder from Veradigm says e-prescribing has ‘absolutely’ lived up to expectations. And she’s right. In places where e-prescribing is standard - like most U.S. outpatient clinics - medication errors have dropped sharply. The number of calls from pharmacists has fallen. Nurses aren’t wasting hours tracking down orders. Patients get the right meds, on time, every time.

The hidden costs of going digital - and how to fix them
But it’s not perfect. Switching to e-prescribing isn’t like flipping a switch. It’s expensive. Setting up a full system can cost $15,000 to $25,000 per provider. Training staff takes 8 to 12 hours. Integrating with existing electronic health records? That’s a technical nightmare for small clinics.
And new problems pop up. Alert fatigue. Clinicians get so many pop-up warnings - ‘This drug interacts with that one!’ ‘This dose is too high!’ - that they start ignoring them. Some studies show doctors override safety alerts up to 90% of the time. That’s not because they’re careless. It’s because the system is noisy. Too many warnings = no warnings.
Then there’s reliability. What if the system crashes? What if the internet goes down? What if the software updates break something? These aren’t theoretical fears. They’ve happened. And when they do, clinics are left scrambling - sometimes falling back to paper, which brings back the old risks.
The fix? Better design. Smart alerts. Fewer, smarter warnings. Backup protocols. Systems that work offline and sync later. Training that doesn’t just teach how to click buttons - but why safety matters. It’s not about tech. It’s about building systems that support people, not frustrate them.
What if your clinic can’t afford e-prescribing?
Not every clinic in the world can afford a $20,000 system. Rural hospitals. Low-income countries. Busy urgent cares. For them, paper is still the only option.
But that doesn’t mean you’re stuck with dangerous prescriptions. There are five simple rules that can slash errors - even on paper:
- Print, don’t write in cursive. Block letters are easier to read. Even if your handwriting isn’t perfect, printed letters reduce confusion.
- Avoid dangerous abbreviations. Never write ‘U’ for units - it looks like a zero. Never use ‘qd’ or ‘qod’ - spell out ‘daily’ or ‘every other day.’ The Joint Commission’s ‘Do Not Use’ list exists for a reason.
- Write the full drug name. Don’t write ‘Lunesta’ - write ‘eszopiclone.’ Don’t abbreviate ‘metformin’ as ‘Met.’ Spell it out.
- Include every detail. Patient name, drug, dose, route (oral, IV, etc.), frequency, duration, and your initials. No shortcuts.
- Use numbers, not words. Write ‘5 mg’ not ‘five milligrams.’ ‘2x daily’ not ‘twice a day.’ Numbers are less ambiguous.
And here’s a pro tip: use a checklist. A 15-item form that both the prescriber and pharmacist can use to verify each detail. One study showed this simple step reduced errors by nearly half - even without going digital.

The future is clear: handwritten prescriptions are dying
Back in 2000, Dr. Lucian Leape and Dr. Donald Berwick called handwritten prescriptions a ‘dinosaur long overdue for extinction.’ They were right. And today, the evidence is overwhelming.
By 2019, 80% of U.S. office-based providers were using e-prescribing. The market is projected to hit $4.2 billion by 2027. Governments are pushing it - Medicare rewards clinics that adopt it. The 21st Century Cures Act demands interoperability. The writing is on the wall.
Even in places where tech is limited, AI is stepping in. New tools can scan handwritten prescriptions and interpret them with 85-92% accuracy. They flag ambiguous terms, suggest corrections, and auto-fill digital records. It’s not perfect - but it’s better than guessing.
By 2030, handwritten prescriptions will be rare in developed countries. Not because doctors hate paper - but because they’ve seen the data. They’ve seen patients die because of a sloppy ‘S’ or a missing decimal point. And they’ve seen how technology can stop it.
The question isn’t whether to switch. It’s when. And how fast you can make the change - before someone else becomes another statistic.
What happens if nothing changes?
Let’s be blunt. If we keep letting doctors scribble prescriptions, more people will die. Not because they’re bad doctors. Not because they’re careless. Because the system lets them be.
Preventable medication errors cost the U.S. healthcare system $20 billion a year. That’s not just money. It’s hospital stays. Emergency visits. Lost work. Families shattered. And every single one of those costs could be reduced - maybe even eliminated - by replacing paper with digital.
Healthcare isn’t just about treating illness. It’s about preventing harm. And the simplest, most proven way to prevent harm from prescriptions? Stop writing them by hand.


Comments
14 Comments
Katherine Carlock
I used to work in a pharmacy and let me tell you, those handwritten scripts were nightmares. I once spent 45 minutes trying to figure out if it was 'hydroxyzine' or 'hydrocodone'. Turned out it was neither-it was 'hydralazine' and the patient was on dialysis. Scary stuff. I'm so glad e-prescribing is finally catching on.
Sona Chandra
This is why India should NEVER copy American healthcare. We have our own system and it works fine. Paper prescriptions are cultural. You people are too obsessed with tech. My uncle is a doctor in Pune and he writes by hand and no one dies. Stop pretending your way is better.
Jennifer Phelps
I think the real issue is alert fatigue and nobody talks about it enough like why do we get 20 pop ups for every prescription and half of them are dumb like 'this drug might cause nausea' duh its a painkiller and also the interface is so clunky i swear some of my coworkers just click through everything because its faster than reading the warnings
Lelia Battle
There's a deeper philosophical question here: when we outsource human judgment to algorithms, do we lose the capacity for care? E-prescribing eliminates errors, yes-but it also removes the quiet moment between doctor and patient where a handwritten note carries intention. The system may be safer, but is it more humane? I wonder if we're trading presence for precision.
Rinky Tandon
The fact that you're even discussing this in 2026 is absurd. We have AI that can read handwriting with 90% accuracy now. Why are you still talking about 'printing block letters'? That's like using a typewriter because your laptop is too expensive. You're clinging to analog solutions like a toddler to a pacifier. The future is here and you're still arguing about pen grip.
Ben Kono
I've seen clinics go digital and then the whole system crashes during flu season and everyone's scrambling with paper again and half the prescriptions get lost or misread anyway so whats the point really
Cassie Widders
My mum’s GP in Cornwall still uses paper. She’s 82. He writes in tiny cursive. I read it for her. It’s not about tech. It’s about trust. He knows her meds, her history, her allergies. The system doesn’t. Sometimes the old way feels safer.
Konika Choudhury
America thinks it can fix everything with apps. In India we have 1.4 billion people and 1 doctor per 1400. We don't have time for your fancy software. We use paper because we have to. And we survive. You think your digital system is better? Tell that to the 10000 people who die from app glitches every year
Darryl Perry
The 7000 deaths stat is inflated. It conflates all medication errors with handwriting. Most are dosing mistakes or drug interactions, not illegibility. Stop using fear to push tech. The real issue is training and oversight, not pens vs pixels.
jordan shiyangeni
Let’s be precise: the Institute of Medicine’s 7,000 annual deaths are an estimate based on extrapolated data from a 2006 study, and subsequent peer-reviewed analyses have revised that figure downward to approximately 2,300–3,100 when controlling for confounding variables. Furthermore, e-prescribing systems exhibit significant variability in error reduction depending on implementation quality, and many are plagued by interoperability failures and vendor lock-in. To claim a 900% improvement is not just misleading-it’s pseudoscientific rhetoric designed to justify corporate procurement budgets, not patient outcomes.
Abner San Diego
I work in a rural clinic. We tried e-prescribing. Cost $22k. Staff hated it. Got hacked once. Got a virus. Took 3 days to fix. We went back to paper. Patients are fine. Doctors are less stressed. The system didn’t save lives-it just made everyone miserable. So yeah, I’m not buying the hype.
Monica Puglia
I love that you mentioned the 5 simple rules 🙌 My grandma’s doctor started using them and she hasn’t had a med error in 2 years. No fancy tech needed. Just care. And maybe a checklist. 💙
Cecelia Alta
Okay but let’s be real-how many of these 'e-prescribing success stories' are just pharma companies pushing their own EHR software? The whole thing feels like a money grab. And don’t get me started on the 'smart alerts'-I’ve seen a doctor ignore 17 warnings because one said 'this might cause drowsiness' and the patient was on a 12-hour shift. We’re automating compliance, not safety. And now we’ve got a generation of docs who can’t even read their own handwriting because they never had to write it anymore. What’s next? AI writes the whole script?
steve ker
Paper prescriptions are inefficient. E-prescribing is the only rational choice. Your resistance is emotional. Not intellectual. You are clinging to outdated paradigms because you lack the cognitive capacity to adapt. The data is clear. Your anecdote is irrelevant.
Write a comment