St. John's Wort Safety Checker
Check Your St. John's Wort Safety
This tool helps determine if your St. John's Wort product is safe to take with HIV protease inhibitors based on hyperforin content.
Imagine taking your HIV meds exactly as prescribed-no missed doses, no shortcuts. Then you start a herbal supplement for your mood, thinking it’s harmless. Within weeks, your viral load spikes. Your treatment fails. Not because you didn’t follow the rules, but because something you thought was safe quietly sabotaged your medicine. This isn’t a hypothetical. It’s happening to real people. And the culprit? St. John’s Wort.
What’s Really Going On Between St. John’s Wort and HIV Meds?
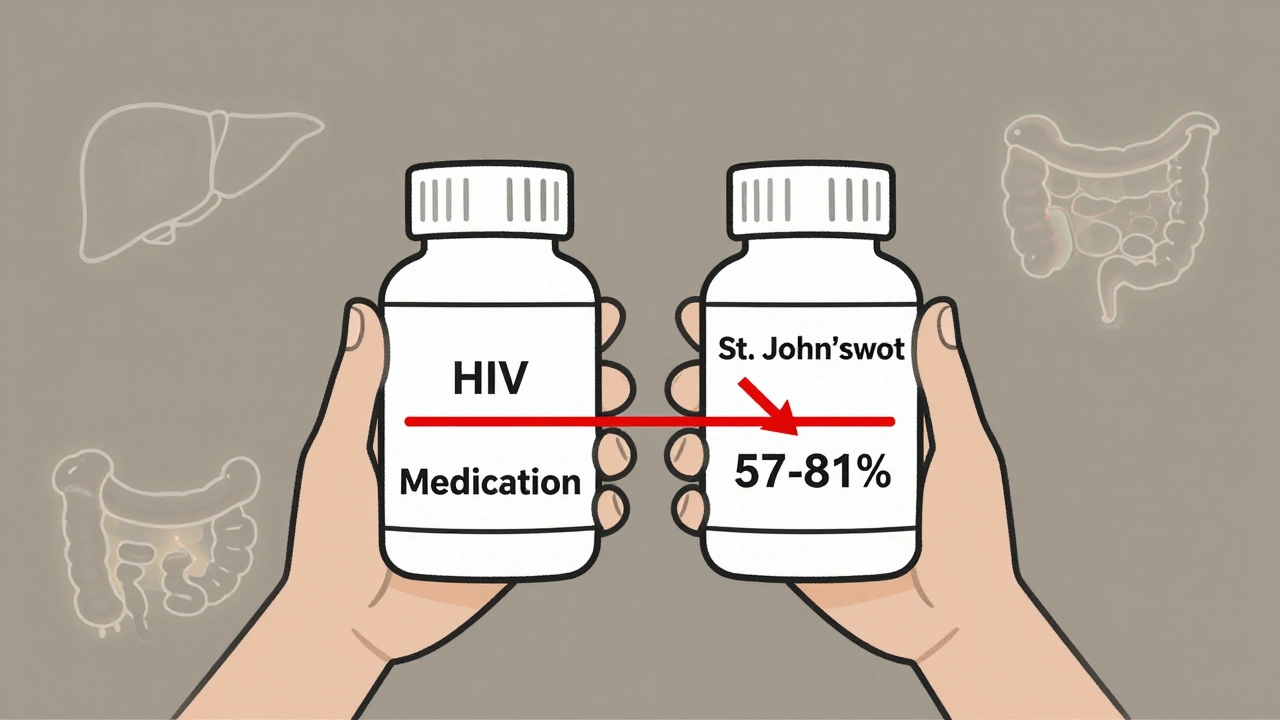
St. John’s Wort is one of the most popular herbal remedies for mild depression. It’s sold over the counter, often labeled as “natural” or “gentle.” But when it meets protease inhibitors-key drugs like lopinavir, ritonavir, or darunavir-that’s when things go wrong. These HIV medications rely on being absorbed properly and staying in your bloodstream long enough to suppress the virus. St. John’s Wort doesn’t just interfere-it actively breaks them down before they can do their job. The reason? Hyperforin. That’s the active ingredient in St. John’s Wort, and it’s a powerful enzyme inducer. It flips a switch in your liver and gut, turning up the production of CYP3A4 and P-glycoprotein. These are the body’s natural cleanup crews. Normally, they help remove toxins. But when they’re overworked by hyperforin, they start chewing up your HIV meds too fast. Plasma levels of protease inhibitors can drop by 40% to over 80%. That’s not a small tweak. That’s a crash. A 2004 study published in Drug Safety showed that just 900 mg of St. John’s Wort daily slashed indinavir levels by 57% in healthy volunteers. Another study found the maximum concentration in the blood dropped by 81%. That’s not just a warning. That’s a red alert. If your drug levels fall below the threshold needed to stop HIV replication, the virus doesn’t just bounce back-it mutates. And once it mutates, the whole class of protease inhibitors might stop working. Forever.It’s Not Just One Drug-It’s the Whole Class
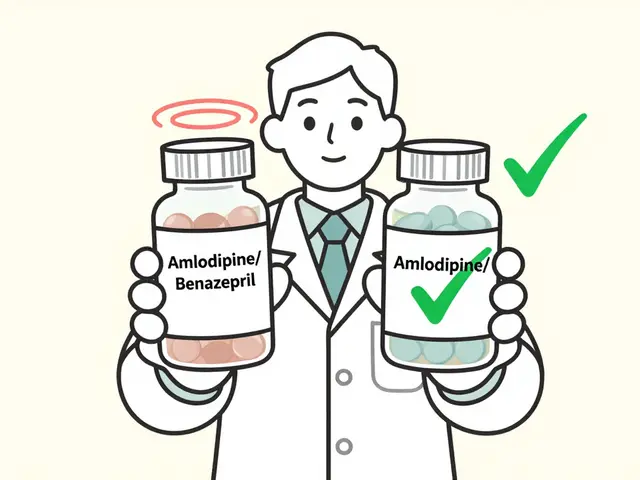
Some people think, “I’m on darunavir, not lopinavir. Maybe I’m safe.” Not true. The interaction affects nearly all protease inhibitors. The University of Liverpool’s HIV Drug Interactions Database, updated in October 2025, lists this as a “Do Not Coadminister” interaction for every major protease inhibitor used in HIV treatment. Why? Because they all share the same metabolic pathway. CYP3A4 is the common target. Once hyperforin turns it on, it doesn’t discriminate. The FDA has required black box warnings on every protease inhibitor label since 2004. That’s the strongest warning they give. It means: “This combination can kill you.” The European Medicines Agency followed suit in 2005. These aren’t bureaucratic footnotes. They’re life-or-death notices backed by years of clinical evidence. Even worse, the damage doesn’t stop when you quit St. John’s Wort. The enzyme induction lasts for at least two weeks after you stop taking it. So if you quit the herb today, your meds still won’t work properly for the next 14 days. That’s a dangerous blind spot. Patients often think, “I stopped the herb, so I’m fine.” But their viral load could be rising during that window.Real Consequences: Virologic Failure Is Not Rare
This isn’t theoretical. In 2021, researchers at the University of North Carolina studied 2,450 HIV patients on protease inhibitors. They found that 8.3% had detectable levels of hyperforin in their blood-meaning they were still taking St. John’s Wort. Of those, 3.1% experienced virologic failure directly linked to the interaction. That’s over 27,000 cases of treatment failure per year in the U.S. alone. Virologic failure doesn’t mean “my cold didn’t go away.” It means your HIV is replicating again. Your CD4 count drops. Your risk of AIDS-related illness climbs. You might need a more complex, more toxic regimen. And if resistance develops, you lose options. Some patients end up on regimens they can’t tolerate. Others face hospitalization. All because they took a supplement they thought was safe. The American Herbal Products Association found that only 22% of St. John’s Wort products warned about HIV interactions in 2000. By 2022, that number jumped to 68%. Progress? Yes. But still, over a third of bottles don’t say a word. And even among those that do, many don’t mention hyperforin-the real trigger.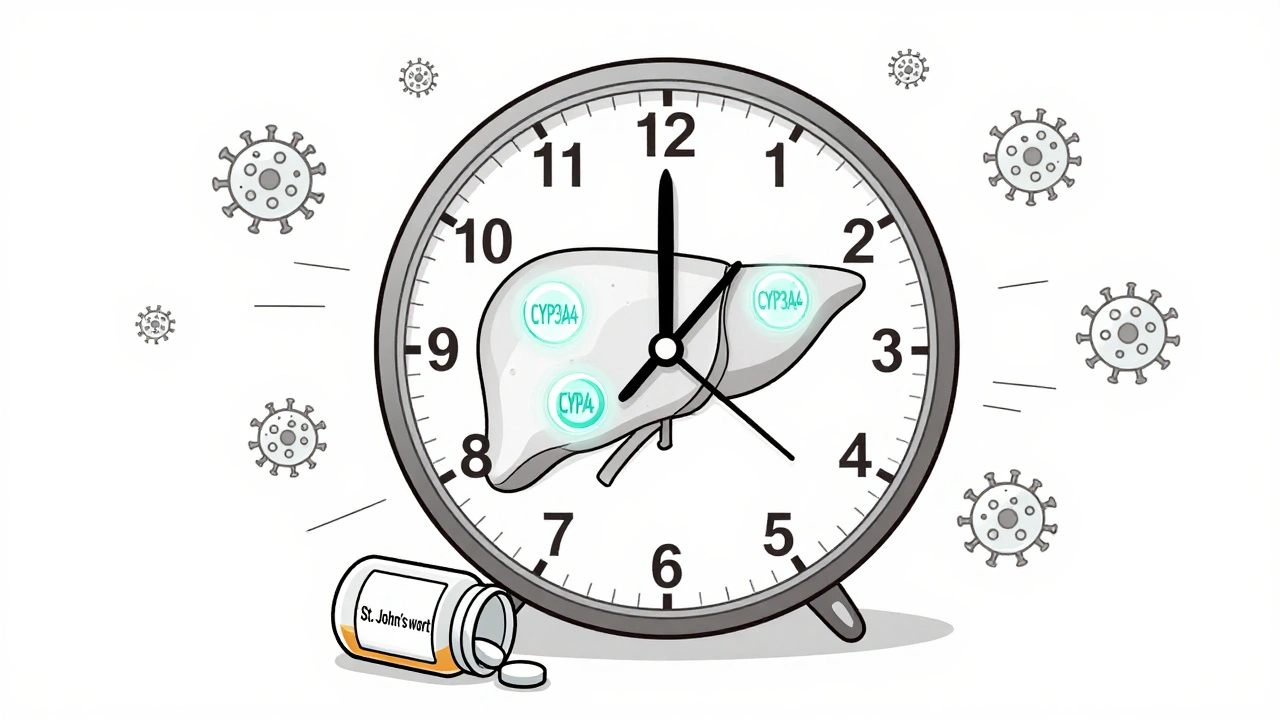
The New Twist: Not All St. John’s Wort Is the Same
Here’s where things get complicated. In 2021, researchers discovered something unexpected: not all St. John’s Wort is dangerous. Low-hyperforin formulations-those with 1 mg or less of hyperforin per day-don’t cause the same drop in drug levels. A 2023 study showed these versions reduced lopinavir levels by only 12.3%, which is within acceptable limits. This changed the game. The University of Liverpool’s database now says: “Coadministration may be considered with St. John’s Wort formulations that clearly state the hyperforin content and which have a total daily hyperforin dose of 1 mg or less.” But here’s the catch: the FDA’s 2022 Dietary Supplement Database found that only 37% of St. John’s Wort products on the market actually list hyperforin content. Most labels just say “standardized extract” or “300 mg, three times daily.” That tells you nothing about hyperforin. You could be taking a safe product-or you could be taking one that’s poisoning your HIV treatment. If you’re considering St. John’s Wort, you need more than a label. You need the exact hyperforin content per capsule. You need to calculate your daily dose. And you need to talk to your HIV provider before even opening the bottle.What Should You Do Instead?
If you’re living with HIV and struggling with depression, you’re not alone. But St. John’s Wort is not your answer. There are safer, proven options. Selective serotonin reuptake inhibitors (SSRIs) like sertraline or escitalopram have been studied extensively in HIV patients and show no dangerous interactions with protease inhibitors. Cognitive behavioral therapy (CBT) works just as well for mild depression and carries zero drug interaction risk. Even regular exercise has been shown to improve mood in people with HIV. The Mayo Clinic and Medsafe New Zealand both recommend talking to your doctor before combining any supplement with HIV meds. Not “maybe.” Not “if you feel like it.” Always. Even if you’ve been taking St. John’s Wort for years. Even if your friend swears by it. Even if your pharmacist didn’t mention it. Your provider needs to know everything you’re taking-vitamins, herbs, teas, over-the-counter sleep aids. Because the hidden risks are everywhere. St. John’s Wort isn’t the only offender. But it’s one of the most dangerous.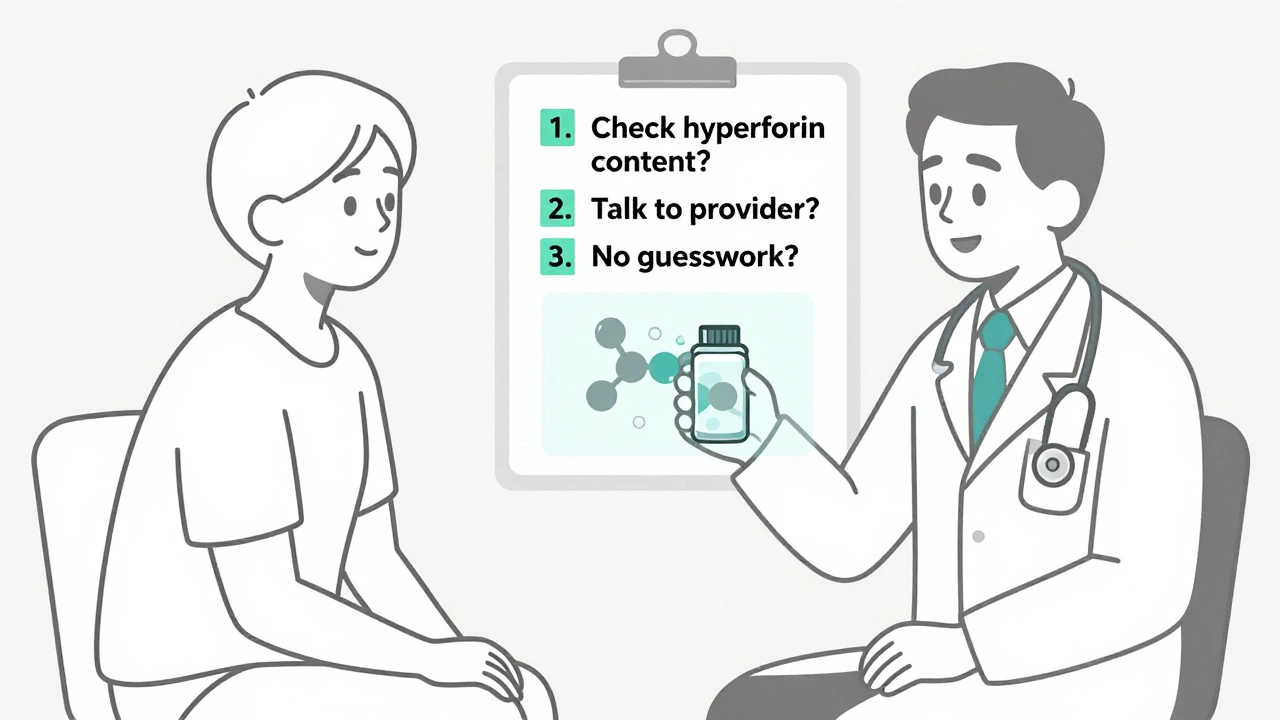
What If You’ve Already Taken Both?
If you’ve been using St. John’s Wort while on protease inhibitors, stop it immediately. Don’t wait. Don’t taper. Stop. Then contact your HIV clinic. Ask for a viral load test. Ask if your drug levels need to be checked. Your provider may need to adjust your dose temporarily while your body clears the enzyme-inducing effects. It can take up to two weeks for CYP3A4 to return to normal. During that time, your meds are still compromised. Don’t assume you’re fine just because you feel okay. HIV doesn’t wait for symptoms. It doesn’t care how you feel. It only cares if your drug levels are high enough to kill it. And if they’re not, it’s already multiplying.How to Protect Yourself Going Forward
Here’s what you need to do, every single time:- Always tell your HIV provider about every supplement, herb, or OTC drug you take-even if you think it’s “just a little.”
- Never start a new supplement without checking the HIV Drug Interactions Database or asking your pharmacist.
- If you see St. John’s Wort on a label, ask: “What’s the hyperforin content per dose?” If they don’t know, don’t take it.
- Use only products that clearly state hyperforin content on the label. If it’s not there, assume it’s dangerous.
- Remember: “Natural” doesn’t mean safe. Especially when you’re on life-saving medication.
There’s no room for guesswork. Your treatment isn’t a suggestion. It’s your lifeline. And St. John’s Wort? It’s not helping. It’s risking everything.
Can I take St. John’s Wort with my HIV meds if I take a low dose?
Only if the product clearly states it contains 1 mg or less of hyperforin per day. Most brands don’t list this information. Without knowing the exact hyperforin content, you cannot assume it’s safe. Even low doses from unknown sources can be risky. Always verify with your HIV provider before using any St. John’s Wort product.
How long does it take for St. John’s Wort to affect my HIV meds?
Effects can begin within days. Studies show significant drops in protease inhibitor levels after just one week of daily use. The enzyme-inducing effect peaks around 10-14 days. That’s why you don’t need to take it for months to cause harm. A few weeks is enough to trigger treatment failure.
What happens if I stop St. John’s Wort-will my meds work again?
Yes, but not right away. The enzyme induction lasts for at least two weeks after you stop taking St. John’s Wort. During that time, your HIV meds are still being broken down too quickly. You need a viral load test after stopping to confirm your treatment is working again. Your provider may need to adjust your dose temporarily.
Are there any herbal alternatives to St. John’s Wort for depression that are safe with HIV meds?
There are no herbal alternatives proven safe with protease inhibitors. Instead, focus on FDA-approved antidepressants like sertraline or escitalopram, which have been studied in HIV patients and show no dangerous interactions. Therapy, exercise, and sleep hygiene are also effective, non-drug options with zero risk.
Why don’t pharmacists always warn me about this?
Many pharmacists aren’t trained to check herbal supplements against HIV drug databases. Also, many St. John’s Wort products don’t list hyperforin content, making it impossible to assess risk. You can’t rely on a pharmacist to catch this. You must proactively ask your HIV provider and verify product labels yourself.
Every time you take a supplement without checking, you’re gambling with your health. HIV treatment works-when it’s not interrupted. Don’t let a bottle of herbs undo everything you’ve worked for.



Comments
11 Comments
Emily Haworth
I KNEW IT!! 🤯 They've been hiding this for DECADES! St. John’s Wort is just a cover-up for Big Pharma to sell more antidepressants!! 🧪💉 My cousin took it with her HIV meds and suddenly she was 'cured'... but then they gave her some new pills and now she's 'sick' again. Coincidence? I THINK NOT. 🌿💀 #ChemtrailsInMyPills
Yatendra S
The universe speaks in biochemical pathways, and hyperforin is just another karmic ripple in the vast ocean of human ignorance. We seek solace in nature, yet poison ourselves with misplaced faith in the 'natural'-as if the earth doesn't also birth venom and plague. 🌱☯️
Himmat Singh
It is an incontrovertible fact that the conflation of herbal supplementation with pharmaceutical regimens constitutes a gross violation of pharmacological protocol. The assertion that 'natural' implies safety is not only fallacious, but egregiously dangerous. One must exercise the utmost diligence when interfacing with bioactive compounds, regardless of their origin.
Alvin Montanez
Look, I get it-people want quick fixes. They want to believe that a little leaf in a bottle can fix their sadness without the 'stigma' of real medicine. But here’s the cold, hard truth: if you’re on HIV meds, you’re not just a person-you’re a walking biological system that’s been fine-tuned by science. And you think a $12 bottle of tea from Whole Foods is going to play nice? That’s not optimism. That’s negligence. You’re not just risking your life-you’re risking the lives of everyone you come into contact with. HIV doesn’t care if you 'feel better.' It only cares if your drug levels are below the threshold. And if they are? Congrats. You just became a walking mutation factory. And no, your 'spiritual journey' doesn’t get a pass. This isn’t yoga class. This is survival.
Lara Tobin
I’m so glad someone finally put this out there. I used to take St. John’s Wort for anxiety, and I had no idea it could mess with my meds. I’m so relieved I found this before it was too late. 💙 You’re not alone if you’ve done this-just know it’s never too late to stop and ask for help.
Jamie Clark
The fact that this even needs to be explained is a testament to how deeply we’ve surrendered our autonomy to corporate wellness culture. We’ve been conditioned to believe that 'natural' equals 'good' and 'pharmaceutical' equals 'evil.' But biology doesn’t care about your feelings. It cares about enzyme kinetics. It cares about CYP3A4 induction. It cares about half-lives and plasma concentrations. You don’t get to opt out of biochemistry because you’re 'spiritual.' If you’re taking anything with your HIV meds, you owe it to yourself to understand the molecular dance happening inside your liver-not just pray it works out.
nithin Kuntumadugu
LMAO so now even herbs are 'dangerous'?? 😂 Like, I'm supposed to believe that a plant from the mountains of Europe is secretly working for Pfizer? 🤡 I took SJW for 3 years with my ARVs and my viral load was undetectable. So either the science is fake or the study was funded by Big Pharma. Either way... 🤷♂️ #NaturalIsBetter #SJWisLife
John Fred
This is GOLD. 🙌 Seriously, if you're on protease inhibitors and you're thinking about any herb, pause. Breathe. Go to the Liverpool database. Check the hyperforin content. If it's not listed? Walk away. You’ve got a lifeline here-don’t let a trendy supplement yank the plug. Your CD4 count will thank you. 💪🩺 #HIVWarrior #KnowYourInteractions
Harriet Wollaston
This hit me right in the feels. I’ve been on HIV meds for 12 years and I took St. John’s Wort for a year thinking it was 'just a tea.' I didn’t know until I read this. I’m so grateful. I’m going to my doctor tomorrow. You’re doing important work. 💕
Lauren Scrima
So... you’re telling me that 'natural' doesn’t mean 'safe'? Shocking. 🙃 I’ll just go tell my 87-year-old aunt who takes ginkgo, turmeric, and 12 vitamins that she’s basically doing a chemistry experiment on her kidneys.
sharon soila
Your health is not a gamble. Every pill you take is a promise-to yourself, to your loved ones, to your future. If you are living with HIV, you have already shown incredible strength. Don’t let a bottle of herbs undo that courage. Talk to your provider. Ask questions. Demand transparency. You deserve to live well, not just survive. And you are not alone in this journey. I believe in you.
Write a comment