Medication Side Effect Reduction Calculator
How Your Lifestyle Impacts Medications
Small changes can cut side effects in half. Based on studies from Harvard Medical School and Mayo Clinic, this tool shows potential reductions in side effects for common medications.
Enter your medication type and activity level to see potential side effect reduction.
Warning: Results are based on published studies. Individual outcomes may vary. This tool is for informational purposes only and does not replace medical advice.
Medications work better when your lifestyle supports them
You’re taking your pills every day. You follow the instructions. But still, you feel tired, nauseous, or gain weight without understanding why. It’s not just bad luck. It’s not your fault. The truth is, your daily habits - what you eat, how you move, how you sleep - can make your medications work better or worse. And the good news? Small, smart changes can cut side effects in half.
Studies show that 6.7% of hospital visits are caused by medication side effects. Many of those could be avoided with simple lifestyle tweaks. The American College of Lifestyle Medicine, Harvard Medical School, and the Mayo Clinic all agree: lifestyle isn’t a backup plan. It’s part of the treatment.
Move more - even if you’re on blood pressure or diabetes meds
If you’re on blood pressure medication, walking 30 minutes a day, five days a week, can drop your systolic pressure by 5 to 8 mmHg. That’s the same drop you’d get from adding another pill - without the extra side effects. The American Heart Association says this level of activity helps your body respond better to meds like ACE inhibitors or beta-blockers.
For people on metformin for diabetes, moving regularly reduces stomach upset by 37%. You don’t need to run a marathon. Start with 10 minutes after lunch. Build up slowly. A 2022 study in Diabetes Care found that people who walked after meals had fewer bloating and diarrhea issues - and better blood sugar control.
Even if you’re on beta-blockers and feel sluggish, exercise helps. A 2022 study showed that people who started with just 10 minutes of walking twice a day, then slowly increased to 30 minutes five days a week, saw a 41% boost in energy within eight weeks. Movement helps your body use the medication more efficiently.
What you eat changes how your drugs work
Food isn’t just fuel - it’s a partner to your meds. Some foods boost effectiveness. Others fight them.
Take warfarin, a blood thinner. If you suddenly eat a lot of kale, spinach, or broccoli - all high in vitamin K - your blood may clot more easily. That’s because vitamin K reverses warfarin’s effect. One cup of cooked spinach has over 1,000 mcg of vitamin K. You don’t need to quit greens. Just keep your intake steady. Eat the same amount every day. That way, your dose stays balanced.
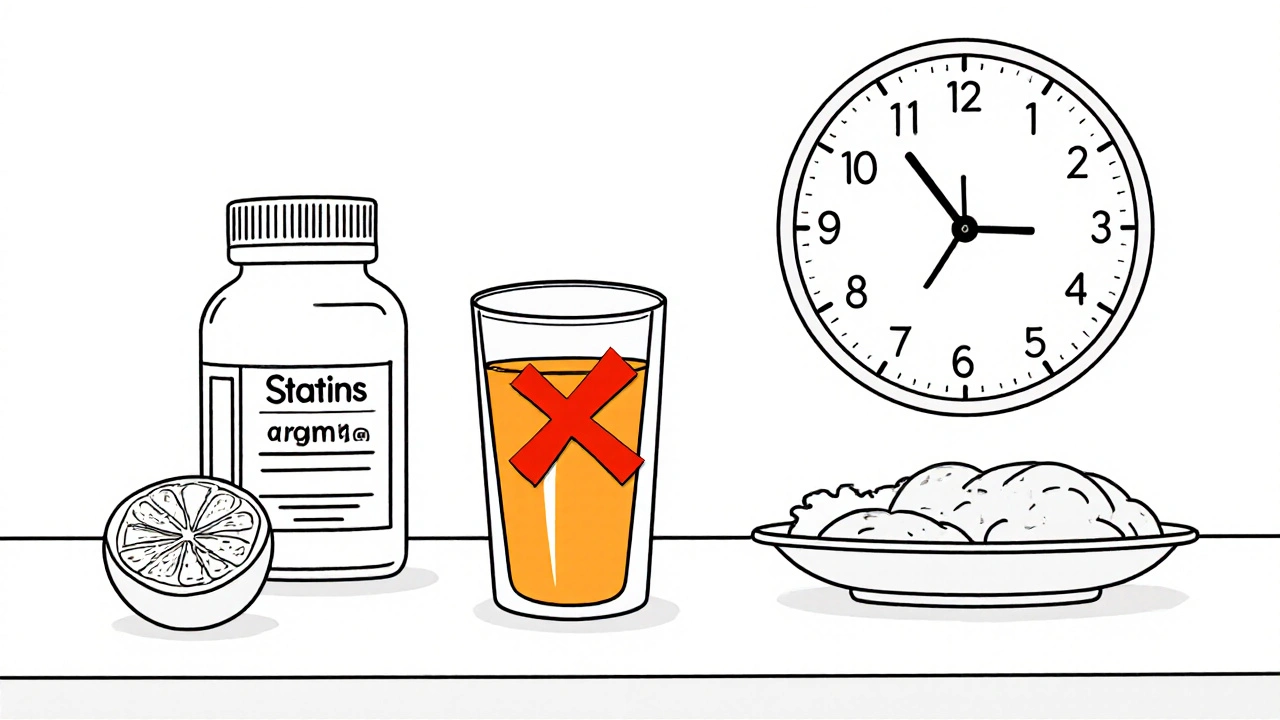
Grapefruit juice is another big one. If you’re on statins for cholesterol, even one glass a day can spike drug levels by 15 to 50%. That raises your risk of muscle pain and liver stress. The same goes for some blood pressure pills and anti-anxiety meds. Check your medication guide. If it says “avoid grapefruit,” skip it.
For GLP-1 agonists like semaglutide (Ozempic, Wegovy), nausea is common - up to 73% of people feel it when starting. But eating slowly (20 to 30 minutes per meal), choosing bland foods, avoiding spicy or greasy meals, and never eating within three hours of bedtime cuts nausea to 29%. Hydration matters too: women should drink 2.2 liters, men 3 liters daily. Water helps your body process the drug without irritation.
Sleep isn’t just rest - it’s medicine
Your liver doesn’t rest when you sleep. It’s busy breaking down drugs. If you’re sleeping less than 7 hours a night, your liver enzymes don’t work as well. That means meds like statins, antidepressants, or painkillers can build up in your blood - leading to more side effects.
A 2021 study from the National Sleep Foundation found that people who got 7 to 9 hours of quality sleep processed medications 22% more efficiently. That’s especially true for drugs broken down by the CYP3A4 enzyme - which includes many statins, antifungals, and some antidepressants.
Try this: Go to bed and wake up at the same time every day, even on weekends. Keep your room cool (65°F is ideal). Avoid screens an hour before bed. If you’re on antidepressants, poor sleep can make weight gain worse. Fix your sleep, and you might not need to adjust your dose.
Stress makes side effects worse - here’s how to fix it
Chronic stress raises cortisol. High cortisol makes your body less responsive to antidepressants. It also increases cravings for sugar and carbs, which leads to weight gain - a common side effect of many psychiatric meds.
A 2021 JAMA Psychiatry study showed that 30 minutes of mindfulness meditation daily lowered cortisol by 27%. That translated to a 31% improvement in how well antidepressants worked - and less weight gain. You don’t need to sit cross-legged for an hour. Try this: Sit quietly, close your eyes, and focus on your breath for 10 minutes, twice a day. Use a free app like Insight Timer if you need guidance.
For people on antipsychotics, weight gain can be severe - up to 7.8 pounds in a year. But a 2023 National Institute of Mental Health protocol found that combining daily exercise (45 minutes at moderate intensity) with protein-rich meals (30g per meal) cut that gain to just 2.1 pounds. Protein keeps you full. Exercise burns fat. Together, they help your body handle the drug better.
Supplements can help - but only if you know which ones
Some supplements aren’t just helpful - they’re backed by science for reducing side effects.
If you’re on statins and get muscle pain, coenzyme Q10 (CoQ10) may help. A 2021 study in the Journal of the American College of Cardiology found that 200mg of CoQ10 daily, combined with light resistance training (two sets of 10 reps, twice a week), cut muscle pain from 29% to 11%. Statins lower CoQ10 in your body - so replacing it makes sense.
For people on metformin, vitamin B12 deficiency is common. Long-term use can drop B12 levels by up to 30%. That can cause fatigue or nerve tingling. Ask your doctor for a blood test. If you’re low, a daily 1,000mcg B12 supplement fixes it.
Don’t take supplements blindly. Some can interfere with meds. Always check with your doctor or pharmacist before starting anything new.

When to talk to your doctor - and what to say
Don’t stop or change your meds on your own. That’s dangerous. But you don’t have to just suffer through side effects either.
Before your next appointment, write down:
- What side effects you’re having
- When they started
- What you changed in your routine (sleep, diet, exercise)
- How often you’re taking your meds exactly as prescribed
Then say this: “I’ve been working on improving my diet, sleep, and movement. I’ve noticed some changes in how I feel. Could we look at whether my lifestyle changes might let us adjust my dose?”
Doctors are more open to this than you think. A 2023 Medscape survey found 87% of physicians now discuss lifestyle changes with patients on meds. But only 38% of visits actually include a structured check-in. Be the one who brings it up.
What doesn’t work - and why
Some people think if they eat healthy and exercise, they can stop their meds. That’s not true. Lifestyle changes help your meds work better - they don’t replace them. Stopping a blood pressure or diabetes med without supervision can cause dangerous spikes.
Also, “natural” doesn’t mean safe. Herbal teas, detoxes, or unregulated supplements can interact with your prescriptions. St. John’s Wort, for example, can make antidepressants, birth control, or blood thinners less effective.
And don’t expect overnight results. The University of North Carolina’s Medication Optimization Program found it takes 8 to 12 weeks for lifestyle changes to show real effects on side effects. Be patient. Track your progress. Small wins add up.
Start with one change - not five
You don’t need to overhaul your life tomorrow. Pick one thing. Just one.
- Drink a glass of water with every pill.
- Walk for 10 minutes after dinner.
- Stop eating 3 hours before bed.
- Swap your morning grapefruit juice for orange juice.
- Set a phone reminder to go to bed at the same time.
Do that for two weeks. Notice how you feel. Then pick another. Slow, steady progress beats big, unsustainable changes.
Medications are tools. Lifestyle is the foundation. When they work together, you feel better - and you need less of the drugs that make you feel worse.
Can lifestyle changes really reduce the need for medication?
Yes - but only under medical supervision. Lifestyle changes like exercise, better sleep, and diet improvements can improve how your body responds to medication. For example, walking 150 minutes a week can lower blood pressure enough to allow a 30-40% dose reduction for some patients. But never stop or lower your dose without talking to your doctor. Rebound effects like high blood pressure or blood sugar spikes can be dangerous.
What foods should I avoid with my meds?
It depends on your medication. Grapefruit juice can dangerously increase levels of statins, blood pressure meds, and some antidepressants. High vitamin K foods like kale and spinach can reduce warfarin’s effect. Salt can make blood pressure meds less effective. Always check your medication guide or ask your pharmacist. Keep your diet consistent - sudden changes are riskier than moderate ones.
How long does it take for lifestyle changes to help with side effects?
Most people start noticing improvements in 4 to 8 weeks. For example, reduced nausea from GLP-1 agonists or better sleep from improved routines often show up within a month. Full benefits - like lower blood pressure or better cholesterol - usually take 8 to 12 weeks. Consistency matters more than intensity.
Can I take supplements to reduce side effects?
Some can help, but only if used correctly. Coenzyme Q10 (200mg daily) reduces statin-related muscle pain. Vitamin B12 (1,000mcg daily) helps if you’re on long-term metformin. But many supplements interfere with medications. Always check with your doctor or pharmacist before starting any new supplement.
Why do I feel more tired on my blood pressure meds?
Beta-blockers and some other blood pressure meds slow your heart rate, which can cause fatigue. But lack of movement makes it worse. Starting with short walks (10 minutes twice a day) and building up to 30 minutes five days a week can improve energy levels by 41% in eight weeks. Exercise helps your body use the medication more efficiently - and boosts natural energy.
Should I track my lifestyle habits?
Yes. Tracking helps you and your doctor see what’s working. Use a simple notebook or phone app to log sleep hours, exercise minutes, meals, and side effects. After two weeks, patterns will appear. Maybe you feel worse after eating pizza at night. Or you sleep better when you turn off screens at 9 p.m. That data turns guesswork into action.





Comments
9 Comments
william volcoff
I've been on metformin for 5 years. Started walking 10 min after dinner and switched from soda to sparkling water. Nausea cut in half. No magic, just consistency.
Also stopped eating pizza at midnight. Game changer.
Freddy Lopez
The notion that lifestyle is part of the treatment, not an add-on, is philosophically profound. We treat medicine as a mechanical intervention, yet the body is a dynamic system. When we align our rhythms with the pharmacology, we don't just reduce side effects-we restore harmony. This isn't compliance. It's collaboration with biology.
Brad Samuels
I used to think sleep was just rest. Then I started tracking my hours and noticed my antidepressant side effects got worse when I slept under 6 hours. Started setting a 10:30 PM alarm to turn off screens. Now I feel like I'm finally getting the full benefit. No more brain fog by 3 PM. Just small things, you know?
Mary Follero
Just wanted to say thank you for this. I'm 68 and on three meds. I was ready to quit because of the fatigue and weight gain. Did the 10-minute walk after lunch and drank more water. Two weeks in, my doctor said my BP is better and asked if I changed something. I didn't even tell him yet. Small wins matter. Keep going, everyone. You got this.
Will Phillips
Lifestyle changes my ass. Big Pharma doesn't want you to know this. They make billions off side effects. They pump money into studies that say 'walk more' so you don't sue them. CoQ10? That's a scam. Your liver doesn't need 'help'-it needs to stop being poisoned by pills. Stop taking them. Go primal. Eat meat. Sleep in the dark. The system is rigged.
Arun Mohan
Honestly, I find it mildly amusing that people think walking after dinner is some kind of biohack. In my country, we've been eating light and sleeping early for centuries. You don't need a Harvard study to know grapefruit juice and statins don't mix. This feels like reinventing the wheel while wearing designer sneakers.
Tyrone Luton
The real issue isn't lifestyle. It's that we've outsourced responsibility for health to doctors and pills. We let the system make us passive. You don't need to 'optimize' your sleep-you need to reclaim your autonomy. That's the deeper truth here. The meds are symptoms of a broken relationship with your own body. Fix that first. Everything else follows.
Jeff Moeller
I tried the 10 minute walk after dinner. Didn't feel anything at first. Kept going. Week 3, I realized I wasn't yawning at my desk anymore. No big epiphany. Just... less tired. Weird how something so simple works when you stop overthinking it.
Herbert Scheffknecht
I used to think supplements were a scam until I started taking CoQ10 with my statin. Muscle pain went from constant to occasional. Then I added two sets of 10 reps twice a week. Not because I wanted to get big. Just to move. And now I'm not dreading my doctor visits anymore. I'm not cured. But I'm not just surviving either. That's enough for now.
Write a comment