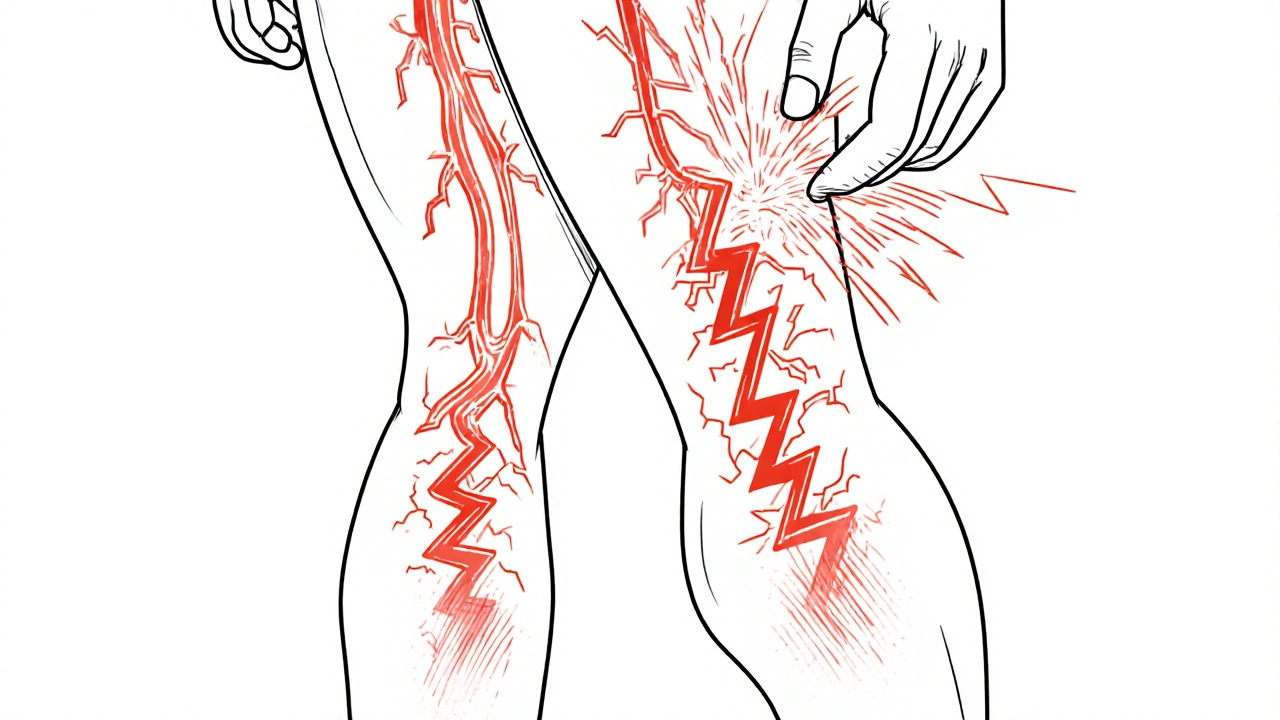
Neuropathic pain isn't just a bad ache. It's the kind of pain that feels like your nerves are on fire, shocked, or buzzing under your skin. You might feel it from something as simple as a light touch - a sheet brushing your leg - or from a tingling that never goes away. About 1 in 10 people live with this kind of pain, often from diabetes, injuries, or surgeries gone wrong. And for many, the first drugs doctors reach for are gabapentin and pregabalin. But they’re not the same. One works faster. The other costs less. One makes you gain weight. The other makes you dizzy. Choosing between them isn’t just about what’s on the prescription pad - it’s about your body, your life, and what you can actually stick with.
What Makes Neuropathic Pain Different?
Normal pain? That’s your body yelling, “I’m hurt!” Neuropathic pain is different. It’s your nerves themselves that are broken. They send wrong signals - like a faulty alarm system that goes off even when there’s no fire. This pain comes from damaged nerves, often from diabetes, shingles, spinal injuries, or even chemotherapy. It doesn’t respond well to regular painkillers like ibuprofen or even opioids. Instead, it needs drugs that calm down overactive nerves. That’s where gabapentin and pregabalin come in.
How Gabapentin Works - And Why It’s Tricky
Gabapentin was originally made for seizures, but doctors noticed it helped with nerve pain too. It works by attaching to a specific part of nerve cells - the alpha-2-delta subunit - and slowing down the flood of signals that cause pain. Sounds simple, right? But here’s the catch: your body doesn’t absorb it well. The more you take, the less your body can process. So you can’t just double the dose and expect double the relief. That’s why doctors start you low - maybe 100mg at night - and creep up slowly over weeks. Most people end up taking 300mg three times a day, totaling 900mg to 3,600mg daily. That’s a lot of pills. And if you miss a dose? The pain can come roaring back because the drug leaves your system in about 6 hours.
Side effects? Dizziness, sleepiness, swelling in the legs, and trouble walking are common. About 1 in 4 people feel dizzy. One in 5 feels so tired they can’t function. But here’s the upside: gabapentin doesn’t usually make you gain weight. In studies, only 3% of users reported noticeable weight gain. And because it’s been generic for years, it costs about $16 for a 90-day supply of 300mg capsules. For people on Medicare or without insurance, that’s a big deal.
Pregabalin - Faster, Stronger, But Heavier
Pregabalin is gabapentin’s bigger, more reliable cousin. It does the same job - binds to the same nerve receptor - but it does it six times more tightly. That means it works faster, more predictably, and you need less of it. You start at 75mg a day, maybe 150mg after a week, and often settle at 300mg daily. That’s just two pills. No need to split doses three times a day. It’s absorbed completely, no matter if you eat or not. Studies show it gives 50% pain relief to about 35% of people with diabetic nerve pain - better than gabapentin’s 30%. And the relief often comes within days, not weeks.
But there’s a trade-off. Pregabalin makes you gain weight. About 1 in 8 people gain 5 to 15 pounds in the first few months. Swelling in the legs and dizziness are even more common than with gabapentin. And because it’s more potent, it’s been classified as a Schedule V controlled substance in the U.S. since 2019. That means pharmacies track your refills, and some doctors are nervous to prescribe it. The cost? Around $28 for 60 capsules of 75mg - nearly double gabapentin’s price. But for many, the faster relief and simpler dosing make it worth it.
Head-to-Head: What the Studies Say
A 2021 analysis of over 4,000 patients found that 300mg of pregabalin worked as well as 3,600mg of gabapentin. That’s a 12-fold difference in dosage. Pregabalin got people to their target dose in just over 8 days. Gabapentin took nearly two weeks. In a 2023 trial with 1,245 patients, 68% of those on pregabalin had their pain cut in half after 12 weeks. For gabapentin, it was 59%. The difference might sound small, but in chronic pain, even 9% matters.
But effectiveness isn’t everything. Patient surveys from 3,842 people on PatientsLikeMe showed pregabalin scored higher on pain relief - 6.2 out of 10 - but lower on tolerability - only 4.8 out of 10. Gabapentin? 5.7 for pain relief, but 5.9 for tolerability. People on gabapentin complained about dizziness and frequent dosing. People on pregabalin complained about weight gain and cost.
One Reddit user wrote: “Pregabalin knocked my pain from 8/10 to 3/10 in 48 hours - but I gained 12 lbs in six weeks. Switched to gabapentin. Took three weeks to work, but no weight gain.” Another said: “Gabapentin made me so dizzy I fell twice. Pregabalin at half the dose? No dizziness. Relief right away.”
Who Gets Which Drug?
Doctors don’t just pick one randomly. They look at your life. If you’re on a tight budget, live in a rural area, or can’t afford to miss a dose because you work two jobs - gabapentin might be the better fit. It’s cheap. It’s available everywhere. And if you can manage the three-times-a-day schedule, it works.
If you’re in an urban clinic, have insurance, struggle with memory or routine, or need fast results - pregabalin wins. The twice-daily dosing is easier. The relief is quicker. And if you’re diabetic, the American Diabetes Association actually recommends pregabalin as the first choice because it’s more consistent in your bloodstream.
But here’s the reality: 35% of people stop gabapentin because the dosing is too complicated. About 28% stop pregabalin because of the cost or weight gain. Neither drug is perfect. That’s why many doctors start with gabapentin, especially if you’re older or have kidney issues. If it doesn’t work after 6 weeks, they switch you to pregabalin.
What About Side Effects and Safety?
Both drugs carry a black box warning from the FDA for suicidal thoughts and mood changes. That’s rare - about 0.4% of users - but serious. Both can cause swelling, dizziness, and trouble concentrating. But pregabalin has a higher risk of weight gain and edema. Gabapentin has a higher risk of falls because of dizziness, especially in older adults.
One big mistake? Stopping either drug suddenly. Both can cause seizures if you quit cold turkey. That’s why doctors make you taper off slowly over weeks. And if you have kidney problems - which many older people do - your dose needs to be lowered. Neither drug is safe at full strength if your kidneys aren’t working well.
The Bigger Picture: Where These Drugs Fit Today
Gabapentin and pregabalin aren’t the only options anymore. Duloxetine, an antidepressant, works well for diabetic nerve pain. Topical lidocaine patches help for localized pain. Newer drugs like cenobamate are coming, but they’re expensive and not yet widely used. Right now, gabapentin and pregabalin are still the most prescribed nerve pain meds in the U.S. - together, they make up over half of all prescriptions.
But the tide is shifting. Pregabalin’s patent expired years ago, and generics are everywhere. Still, brand-name Lyrica still sells for billions because doctors trust it. Gabapentin’s sales are stable because it’s dirt cheap and reliable for people who can handle the dosing. In safety-net hospitals, 68% of patients get gabapentin. In academic medical centers, 57% get pregabalin.
By 2028, experts predict pregabalin’s use will drop a little as newer drugs arrive. Gabapentin? It’s not going anywhere. Not while it costs less than a coffee a day.
What Should You Do?
If you’re starting one of these drugs:
- Start low. Don’t rush the dose. Your body needs time to adjust.
- Track your pain, side effects, and weight. Use a notebook or phone app.
- Don’t stop suddenly. Always talk to your doctor before quitting.
- If gabapentin makes you dizzy or you can’t remember to take it three times a day, ask about pregabalin.
- If pregabalin makes you gain weight or costs too much, ask about switching to gabapentin.
There’s no single right answer. It’s about balance: relief vs. side effects, cost vs. convenience, simplicity vs. effectiveness. The best drug is the one you can take - and stick with - without ruining your life.
Which is better for diabetic nerve pain - gabapentin or pregabalin?
Pregabalin is generally preferred for diabetic neuropathy because it has more consistent absorption, works faster, and requires fewer daily doses. The American Diabetes Association recommends it as a first-line option. However, gabapentin is still effective and often chosen for cost reasons or if weight gain is a concern.
Can I switch from gabapentin to pregabalin?
Yes, but not directly. Because they’re not 1:1 interchangeable, your doctor will likely taper you off gabapentin slowly and start you on a low dose of pregabalin. A common starting point is 75mg of pregabalin daily, adjusted based on your pain and side effects. Never switch on your own - abrupt changes can cause seizures or worsen pain.
Why does pregabalin cause weight gain?
The exact reason isn’t fully understood, but pregabalin appears to increase appetite and may affect how the body stores fat. Studies show about 12% of users gain 5% or more of their body weight within the first few months. This is much higher than with gabapentin, where weight gain affects only about 3% of users.
Is gabapentin safer than pregabalin?
Both have similar safety profiles for serious side effects like suicidal thoughts or angioedema. Gabapentin has no controlled substance status, while pregabalin is Schedule V due to misuse potential. However, gabapentin carries a higher risk of dizziness and falls, especially in older adults. Neither is universally “safer” - it depends on your health, age, and lifestyle.
How long does it take for these drugs to work?
Pregabalin often starts working in 3-7 days, with noticeable relief in about a week. Gabapentin usually takes 2-4 weeks to reach full effect because of slower titration and less predictable absorption. Some people feel better sooner on gabapentin, but it’s less common. Patience is key - both require time to build up in your system.
Can I drink alcohol while taking gabapentin or pregabalin?
No. Alcohol increases dizziness, sleepiness, and the risk of falls. It can also worsen the sedative effects of both drugs. Even one drink can be dangerous, especially when you’re first starting treatment or adjusting your dose. Avoid alcohol entirely unless your doctor says otherwise.
What If It Doesn’t Work?
If neither gabapentin nor pregabalin gives you enough relief after 6-8 weeks, talk to your doctor about alternatives. Duloxetine (Cymbalta) is often next - it’s an antidepressant that works well for nerve pain. Topical treatments like lidocaine patches or capsaicin cream can help if your pain is in one area. For severe cases, nerve blocks or spinal cord stimulators might be options. The goal isn’t to find one magic pill - it’s to find a mix that lets you live without being ruled by pain.


Comments
12 Comments
Liam Strachan
Been on gabapentin for 3 years now for diabetic neuropathy. It’s not glamorous, but it keeps me walking. Dizziness? Yeah, especially when I first started. But I learned to take it with food and nap after the night dose. No weight gain, which matters when you’re already fighting insulin resistance. I get 300mg three times a day - yeah, it’s a pain to remember, but I set phone alarms. Worth it.
Gerald Cheruiyot
Real talk - if you’re not tracking your symptoms, you’re just guessing. I used to think pregabalin was the ‘premium’ option. Turns out, it’s just more expensive. Gabapentin works if you give it time. Your body isn’t a machine that responds to the shiniest pill. It’s a slow burn. Patience > potency.
Michael Fessler
From a clinical pharmacology standpoint, the alpha-2-delta binding affinity of pregabalin is significantly higher (Kd ~15nM) versus gabapentin (Kd ~90nM), which explains the superior bioavailability and pharmacokinetic consistency. However, the CYP450-independent metabolism of both agents means renal clearance dominates - so in CKD patients, dose reduction is non-negotiable. Also, the 12-fold dosage disparity in comparative trials isn’t linear due to saturable absorption kinetics in gabapentin. Bottom line: efficacy is similar at therapeutic doses, but tolerability profiles diverge significantly due to off-target GABAergic modulation.
daniel lopez
They don’t want you to know this, but both drugs were originally designed as sedatives for military use. The weight gain? That’s the government’s way of keeping veterans docile. And the Schedule V status? That’s because Big Pharma realized they could make billions off something that makes you sleepy and hungry. Gabapentin’s cheap because it’s old - but it’s also the only one they didn’t patent into oblivion. Watch out for the ‘neuropathic pain’ diagnosis - it’s become a catch-all for when they don’t know what’s wrong with you.
Nosipho Mbambo
Ugh. I just want my pain to go away. Why does it have to be so complicated? I tried gabapentin - dizzy. Pregabalin - gained 10 lbs. Now I’m on duloxetine, which makes me nauseous. So I’m just… stuck. And now I have to track everything? In a notebook? I can barely remember to take my vitamins. This is exhausting. Can’t we just have one magic pill that doesn’t make you feel like a zombie or a balloon?
Katie Magnus
Okay but… why are we even talking about these two? They’re basically just sedatives with a fancy label. Real healing isn’t about chemical suppression - it’s about yoga, fasting, and energy work. I cured my neuropathy with sound baths and a 30-day lemon water cleanse. These drugs? They’re just bandaids on a bullet wound. And don’t even get me started on how the medical industrial complex profits from keeping people dependent.
King Over
Used both. Gabapentin made me nod off at my desk. Pregabalin made me feel like a marshmallow. I switched to CBD oil. No dizziness. No weight gain. Just quiet. Doctors hate that you can buy it online. Guess they don’t get a cut.
Johannah Lavin
I just want to say - if you’re reading this and you’re struggling with nerve pain, you’re not alone. I’ve been there. The dizziness, the weight gain, the guilt when you can’t keep up with your life - it’s heavy. But you’re still here. That matters. And if gabapentin lets you hug your kid without crying? That’s a win. If pregabalin lets you sleep through the night? That’s a win too. There’s no shame in what works. You’re not failing. You’re fighting.
Ravinder Singh
Bro, I’m from India - gabapentin costs ₹12 for 30 capsules 😎. Pregabalin? ₹800. I started on gabapentin, took 3 months to feel relief, but now I’m stable. No weight gain, no dizziness after I adjusted timing. My tip? Take it with a banana - helps with absorption and reduces stomach upset. Also, don’t skip doses - even if you feel fine. Nerves don’t care if you’re lazy. Stay consistent, stay patient. You got this 💪
Russ Bergeman
Wait - you’re seriously comparing these two? Gabapentin is a junk drug. It’s not even FDA-approved for nerve pain. Pregabalin’s the only one with real data. And you’re telling me people are choosing the one that makes them fall down? That’s not a choice - that’s negligence. And the weight gain? You’re just lazy. Exercise. Stop eating carbs. You want relief? Take responsibility.
Dana Oralkhan
Hey - I read your comment, and I just want to say thank you. I’ve been feeling so alone with this. I’ve been on gabapentin for 8 months. I’m still dizzy sometimes, but I can walk to the mailbox now. That’s huge. I didn’t think anyone else understood how hard it is to just… keep going. You’re right. We’re not failing. We’re surviving. And that’s enough.
Jeremy Samuel
gabapentin is just a placebo with side effects. pregabalin is the same but with a fancy name. the real fix is keto and red light therapy. also, your doctor is lying to you. just saying.
Write a comment