After a colonoscopy finds and removes polyps, many people wonder: when do I need another one? It’s not a one-size-fits-all answer. The timing depends on what kind of polyps were found, how many, how big they were, and even how well the bowel was cleaned before the procedure. Getting a repeat colonoscopy too soon wastes resources and adds unnecessary stress. Waiting too long could miss a dangerous growth. The good news? Modern guidelines have made this much clearer - if you know what to look for.
What Counts as Low-Risk Polyps?
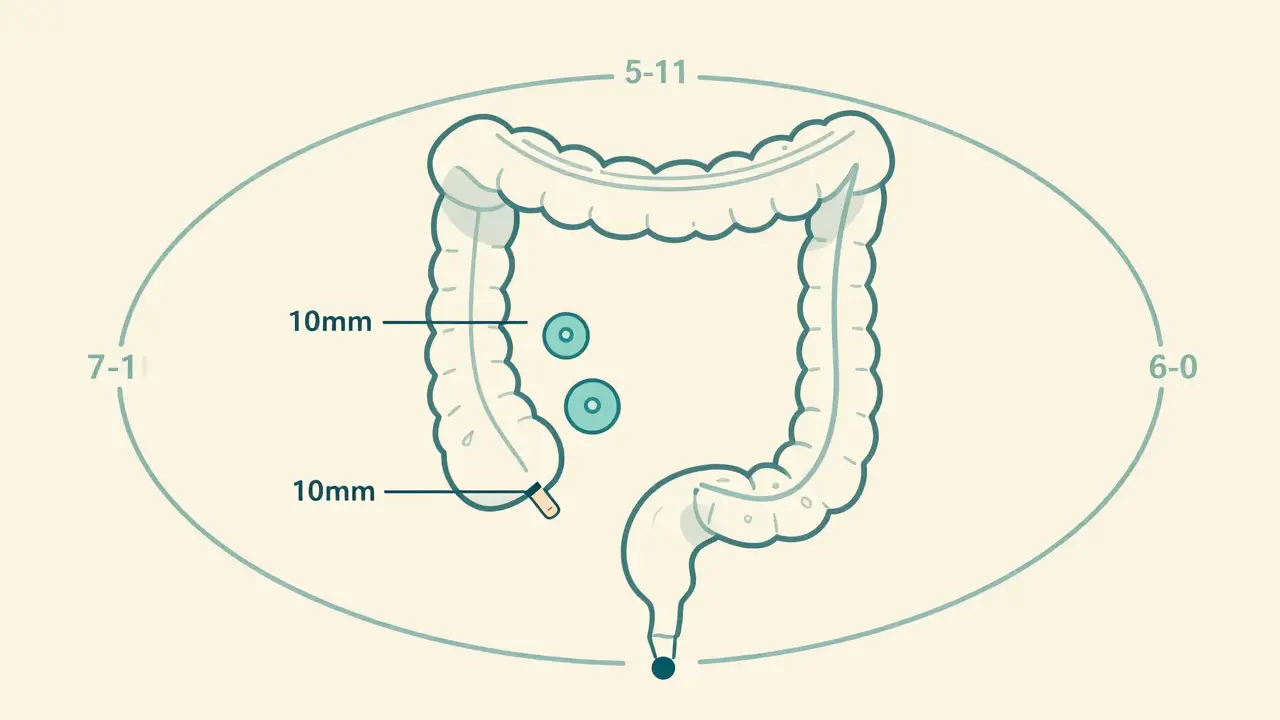
Not all polyps are the same. The most common type found during screening is the adenoma, a benign growth that can slowly turn into cancer over 10-15 years. But not all adenomas carry the same risk. A 2020 update from the US Multi-Society Task Force on Colorectal Cancer changed the game by extending surveillance intervals for low-risk cases. Now, if you have one or two adenomas smaller than 10 mm, you likely don’t need another colonoscopy for 7 to 10 years. That’s a big shift from the old 5-year rule.What makes a polyp low-risk? Size matters. Polyps under 10 mm are considered small. Histology matters too - tubular adenomas are less concerning than villous or tubulovillous types. And if the polyp was removed completely in one piece (en bloc resection), that’s a good sign. If you have only one or two of these small, low-risk adenomas, your cancer risk is almost the same as someone with a completely normal colon. Studies show 98.7% of people in this group remain cancer-free after 10 years.
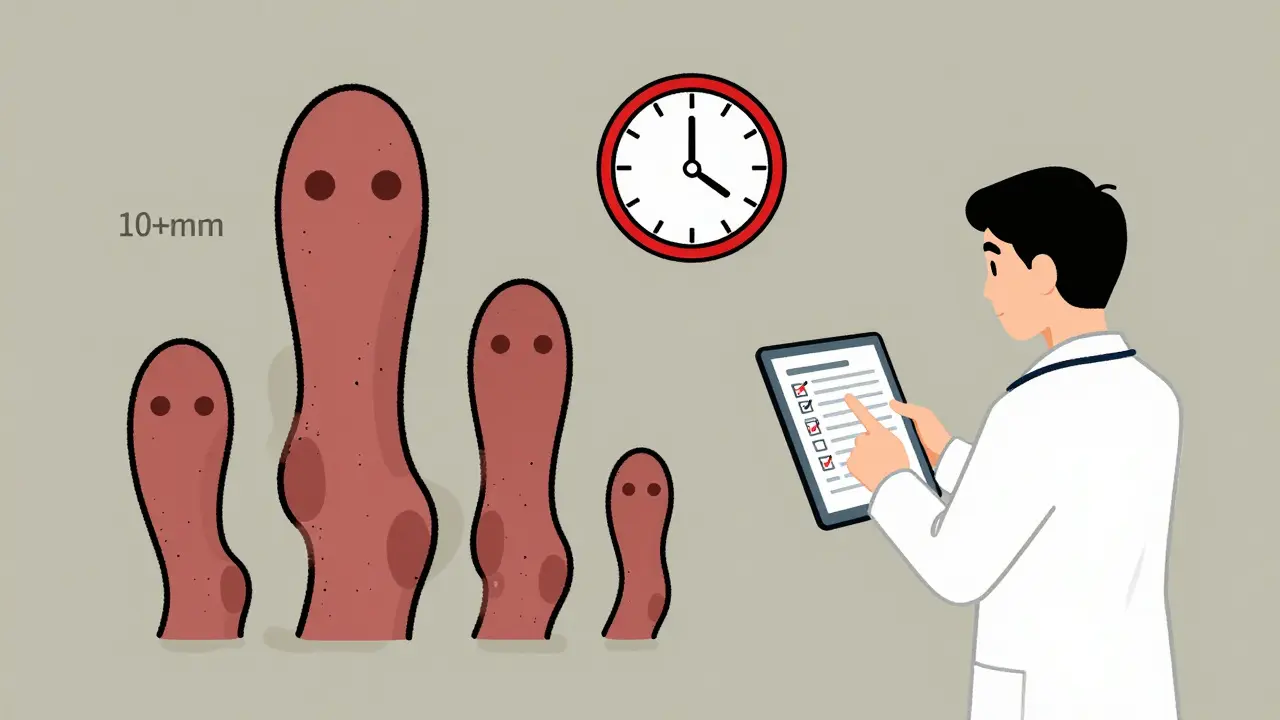
When You Need a Repeat Colonoscopy Sooner
If your polyps were bigger, more numerous, or had high-risk features, the clock resets faster. Here’s when you’ll need a follow-up sooner:- Three or four adenomas under 10 mm → Repeat in 3 to 5 years
- Five or more adenomas of any size → Repeat in 3 years
- Any adenoma 10 mm or larger → Repeat in 3 years
- Villous or high-grade dysplasia → Repeat in 3 years
- Traditional serrated adenoma → Repeat in 3 years
These are not arbitrary numbers. They’re based on data showing that polyps with these features are more likely to come back or develop into cancer within a few years. Missing a follow-up at this stage increases your risk significantly.
Serrated Polyps Are Different - And Often Overlooked
Serrated polyps, especially sessile serrated lesions (SSLs), are tricky. They don’t look like traditional adenomas. They’re flat, pale, and often hidden in the right side of the colon. But they’re just as dangerous - and they can turn into cancer faster than adenomas.For one or two SSLs smaller than 10 mm, the recommendation is now 5 to 10 years. But if you have three to four, go back in 3 to 5 years. Five or more? Back in 3 years. The catch? Many doctors still confuse SSLs with hyperplastic polyps (HPs), which are usually harmless. If there’s any doubt - especially if the bowel prep was poor or the polyp wasn’t fully removed - play it safe and schedule a repeat colonoscopy in 3 to 5 years.
Hyperplastic polyps over 10 mm are also a red flag. Even though most HPs are benign, large ones can be hard to tell apart from SSLs. So if you have one larger than 1 cm, plan on a repeat colonoscopy in 3 to 5 years.
What If the Polyp Was Removed in Pieces?
Sometimes, large polyps - especially those over 20 mm - can’t be removed in one piece. When that happens, there’s a higher chance some tissue was left behind. That’s why follow-up timing changes dramatically.In the UK, guidelines from the British Society of Gastroenterology (BSG) and colleagues recommend two follow-ups: one at 2 to 6 months to check for leftover tissue, and another at 18 months to confirm everything is clear. In the US, the standard is a single repeat at 6 months. Both approaches aim to catch any regrowth early.
Some European guidelines suggest a window of 3 to 6 months, giving doctors flexibility based on how confident they are about the resection. But if you’re in the US or following US guidelines, expect that 6-month mark. Don’t skip it. Residual tissue can turn into cancer within a year if left unchecked.
What About Serrated Polyposis Syndrome?
This rare condition means you have a lot of serrated polyps scattered throughout your colon - often more than 20. People with this syndrome have a very high lifetime risk of colorectal cancer, sometimes over 70%. Surveillance here is intense.In the UK, guidelines recommend a colonoscopy every 1 to 2 years until age 75. If you go through two consecutive exams with no polyps larger than 10 mm, your doctor might stretch the interval to 2 years. In Japan, annual colonoscopies are standard. This isn’t about being overly cautious - it’s about survival. Missing a check-up in this group can be deadly.
Why Are So Many People Getting Colonoscopies Too Soon?
Despite clear guidelines, most patients are getting colonoscopies way too early. A 2020 study at a Veterans Affairs hospital found that only 18.6% of doctors followed the updated 7-10 year rule for low-risk adenomas. Over 80% still recommended 5-year intervals - even though they knew the new guidelines.Why? Fear. Fear of missing something. Fear of lawsuits. Fear that patients will complain if they’re told to wait longer. There’s also confusion. Many primary care doctors, who handle follow-up care, don’t know the latest rules. A 2022 survey found only 37% of gastroenterologists could correctly identify all the risk categories. For serrated polyps? Only 28% got it right.
And it’s expensive. In the US alone, 15 million colonoscopies are done each year. If even a third of those are unnecessary due to outdated advice, that’s hundreds of millions of dollars wasted - and thousands of people subjected to avoidable procedures.
What Tools Are Helping Doctors Get It Right?
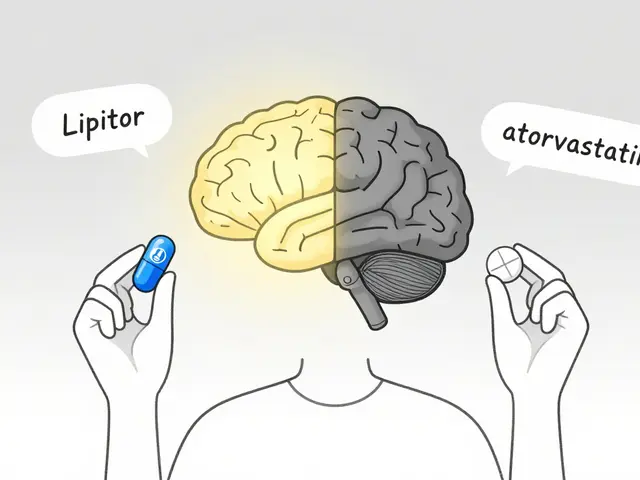
Technology is stepping in. Apps like Polyp.app, developed by gastroenterologists at Massachusetts General Hospital, let doctors input polyp details and instantly get the correct surveillance interval. As of 2023, over 12,400 clinicians use it. Electronic health record systems like Epic and Cerner now have built-in prompts that remind doctors to recommend the right follow-up based on what was found.But tools aren’t enough. The real fix is education. Patients need to understand why they’re being told to wait 10 years - and doctors need to feel confident enough to say it. When patients are given clear, evidence-based reasons, they’re more likely to follow through. One study showed that when patients were told, “Your risk is almost the same as someone with no polyps,” 92% agreed to wait 10 years.

What’s Next? Personalized Surveillance
The future of colonoscopy surveillance isn’t just about counting polyps. Researchers are now testing blood and stool tests that look for DNA changes linked to cancer risk. If a patient has a polyp with a certain molecular signature, their follow-up might be shortened - even if the polyp looked small and harmless.Trials are underway to see if these biomarkers can replace or refine current rules. Dr. Samir Gupta, one of the authors of the 2020 guidelines, says we’re moving toward a future where your surveillance schedule is tailored to your biology - not just your polyp count.
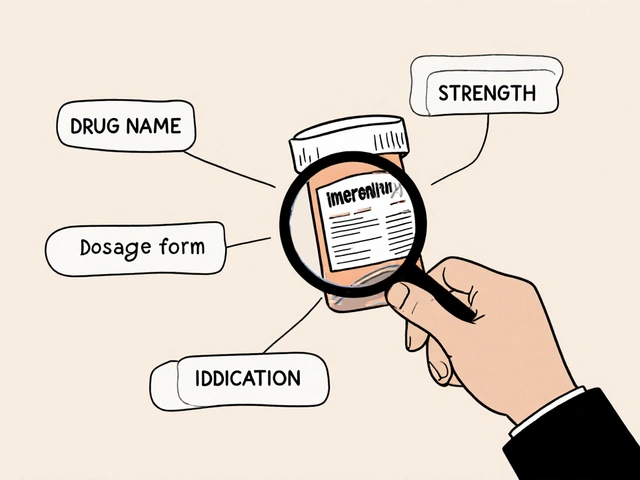
For now, though, stick to the numbers. Know what was found. Ask your doctor: “What kind of polyps were removed? How big were they? Was the resection complete?” Write it down. Then, based on that, you’ll know exactly when to schedule your next colonoscopy.
What If I Can’t Remember What Was Found?
If you don’t have your pathology report or aren’t sure what type of polyps were removed, don’t guess. Call your endoscopist’s office. Request a copy of your colonoscopy report and pathology results. Most clinics can email or mail them to you within a few days. If you had the procedure at a hospital, you can often access it through your patient portal.If you truly can’t get the details, play it safe. Assume the worst-case scenario - that you had larger or more numerous polyps - and schedule a colonoscopy in 3 years. It’s better to be cautious than to risk missing something.
How long should I wait for my next colonoscopy after removing one small adenoma?
If you had one or two adenomas smaller than 10 mm and they were completely removed, you should wait 7 to 10 years for your next colonoscopy. This is based on the 2020 US guidelines, which show your cancer risk is nearly the same as someone with no polyps. Don’t assume you need one every 5 years - that’s outdated advice.
Do serrated polyps require more frequent follow-up than adenomas?
Yes, but it depends. Small sessile serrated lesions (SSLs) under 10 mm with no dysplasia follow the same 5-10 year rule as low-risk adenomas. But if you have three or more SSLs, or any SSL larger than 10 mm, you need a repeat colonoscopy in 3-5 years. SSLs can turn into cancer faster than adenomas, and they’re often missed during screening - so follow-up timing matters more.
What if my polyp was removed in pieces?
If a polyp larger than 20 mm was removed in pieces (piecemeal resection), you need a follow-up colonoscopy in 6 months. This is to make sure no tissue was left behind. In the UK, guidelines suggest a second check at 18 months. Skipping this step increases the risk of cancer developing from leftover cells.
Why do some doctors still recommend a 5-year interval?
Many doctors stick to the old 5-year rule out of habit, fear of liability, or because they’re not up to date. Studies show over 80% of US gastroenterologists still recommend 5-year intervals for low-risk adenomas, even though guidelines changed in 2020. It’s not that they’re wrong - they’re just behind the science. Always ask for the reasoning behind your recommendation.
Can I skip my next colonoscopy if I feel fine?
No. Colorectal cancer often has no symptoms until it’s advanced. Polyps that turn cancerous grow silently. Even if you feel perfectly healthy, skipping your scheduled colonoscopy based on how you feel is risky. The goal of surveillance is prevention - not symptom detection.

Comments
15 Comments
Siobhan K.
I still can't believe some doctors are pushing 5-year follow-ups for small adenomas. The 2020 guidelines are clear, and yet here we are, stuck in 2015. It's not just outdated-it's wasteful and anxiety-inducing for patients who don't need to be scared every other year.
My GI told me 10 years after two 6mm tubular adenomas. I almost cried I was so relieved. No more annual panic about bowel prep.
Brian Furnell
The distinction between tubular adenomas and sessile serrated lesions is critically underappreciated in primary care settings. Serrated lesions, particularly those with BRAF mutations and CpG island methylator phenotype (CIMP), demonstrate accelerated carcinogenesis via the serrated neoplasia pathway-distinct from the traditional adenoma-carcinoma sequence.
Moreover, the diagnostic accuracy of endoscopists in differentiating SSLs from hyperplastic polyps remains suboptimal, with interobserver variability exceeding 30% in some studies. This necessitates not only better training but also mandatory pathology review for any right-sided diminutive polyp.
Jason Silva
They're lying to you. 😒 The real reason they want you back in 5 years? $$$
Colonoscopies are a cash cow. Hospitals make $2k+ per procedure. The guidelines changed because they got caught. Now they're pretending to be 'evidence-based' while still pushing unnecessary scans. I got mine at 45. Next one? 2040. I'm not falling for it.
mukesh matav
I had one small polyp removed last year. Doctor said 10 years. I just nodded and didn't ask questions. I trust him. If he says it's fine, I believe it. No need to overthink.
Peggy Adams
Ugh. I just had my third colonoscopy in 8 years. First one found a tiny polyp. Second one was 'just to be safe'. Third one? They found nothing. I'm done. If I feel fine, why am I getting poked with a camera every 3 years? I'm not a lab rat.
Sarah Williams
You got this. Seriously. If you have small, low-risk polyps, you're in the 98.7% club. Don't let fear or outdated advice scare you into unnecessary procedures. Your body isn't broken. You're just human. And humans don't need colonoscopies every 5 years like clockwork.
Theo Newbold
The data is cherry-picked. The 7-10 year interval assumes perfect resection, perfect prep, perfect endoscopist skill, and zero confounding variables. In real-world practice, bowel prep is often inadequate, polyps are missed, and resection margins are unclear. The 5-year rule isn't outdated-it's a safety buffer for a broken system.
Jackie Be
I had a polyp removed and they said 10 years and I was like YAS QUEEN 😍 I felt like I won the lottery
then my mom called and said she had hers every 5 and she's still alive so I started doubting everything
now I'm just waiting for the universe to send me a sign
John Hay
I'm not a doctor but I read the guidelines. If you have one or two small adenomas, 7 to 10 years is correct. If your doctor says 5, ask why. If they can't explain it with the 2020 guidelines, they're not keeping up. Don't be afraid to push back.
Jon Paramore
The real issue isn't the interval-it's the diagnostic inconsistency. Endoscopists misclassify 15-20% of SSLs as hyperplastic polyps, especially when they're flat or in the proximal colon. This leads to under-surveillance. The 5-year rule persists not because it's right, but because it's a fail-safe against misdiagnosis.
Swapneel Mehta
I live in India and we don't have access to this level of care. Most people get colonoscopies only when they're in pain. I'm lucky I got mine done at a private clinic. I don't know if my polyp was small or big. I just hope I did the right thing.
Stacey Smith
This is why America is falling apart. We're so obsessed with over-testing that we're wasting billions. In Europe, they wait 10 years and still have lower cancer rates. We need to stop being scared of everything and start trusting science, not fear.
Ben Warren
The current paradigm of colonoscopic surveillance is predicated upon a flawed epistemological framework that privileges categorical classification over probabilistic risk stratification. The reliance upon polyp count, size, and histology as deterministic predictors of malignant transformation neglects the dynamic interplay of genetic, epigenetic, and environmental factors that modulate carcinogenesis.
Moreover, the dissemination of guidelines by professional societies, while ostensibly evidence-based, often reflects institutional inertia and conflicts of interest, particularly in relation to procedural revenue streams. The 7- to 10-year interval for low-risk adenomas, while statistically sound in controlled cohorts, lacks external validity in heterogeneous, real-world populations where confounders such as microbiome dysbiosis, dietary fiber intake, and metabolic syndrome remain unaccounted for.
Teya Derksen Friesen
I appreciate the clarity of these guidelines. As a healthcare administrator, I've seen firsthand how inconsistent follow-up protocols lead to inefficiencies and patient anxiety. Implementing standardized electronic prompts in EHRs has reduced unnecessary colonoscopies by 22% in our network. Education works-when it's systemic.
Sandy Crux
You're all missing the point. The real problem is that colonoscopy is a blunt instrument. We're treating a complex, multifactorial disease with a single, invasive, expensive, and imperfect tool. What about stool DNA tests? Blood biomarkers? AI-enhanced imaging? We're clinging to a 1980s diagnostic method because it's profitable and familiar. The 7-year rule is just a placebo for our collective denial.
Write a comment