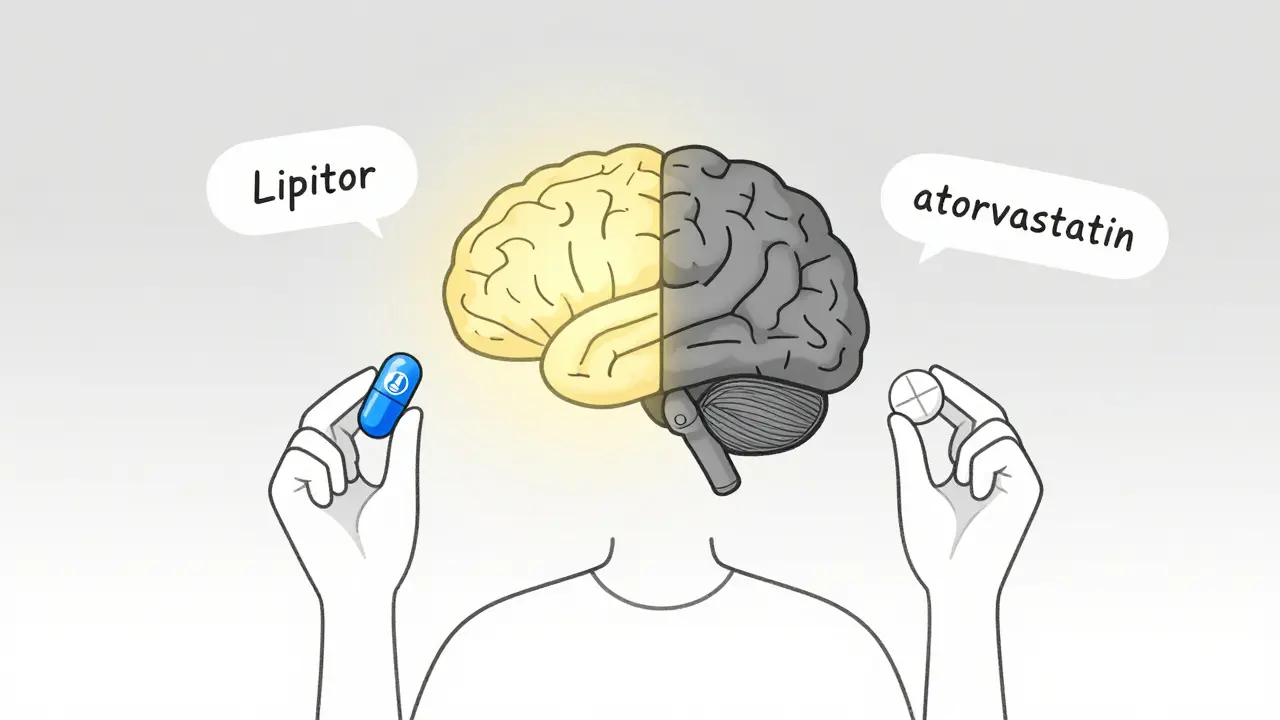
When you switch from a brand-name pill to a generic version, your body doesn’t change-but your brain might. Even if the active ingredient is identical, many people report feeling less relief, more side effects, or just a general sense that the generic isn’t working as well. This isn’t in your head in the way you think. It’s in your head in the way science now understands: placebo effect is real, powerful, and deeply tied to what you believe about your medicine.
Why a Generic Can Feel Different Even When It’s the Same
A generic drug isn’t a copycat. It’s the exact same chemical as the brand-name version, approved by the FDA to work the same way. The difference? The packaging, the color, the shape, and most importantly-the label. A 2014 study showed that when people took a sugar pill labeled as a well-known brand-name painkiller, they felt just as much relief as if they’d taken real ibuprofen. But when the exact same sugar pill was labeled as a generic, the pain relief dropped by nearly 40%. That’s not chemistry. That’s psychology. This isn’t rare. In fact, about 30% of patients still believe generics are less effective-even though 70% know they’re chemically identical. The brain doesn’t care about bioequivalence percentages. It cares about trust. And if you’ve spent years taking a blue pill called "Lipitor," switching to a white pill called "atorvastatin" can feel like losing something even when nothing has changed.The Brain’s Role in How Medicine Works
Your brain doesn’t just passively receive drugs. It actively predicts how they’ll work. When you see a familiar brand name, your brain activates regions linked to expectation and reward-like the dorsolateral prefrontal cortex. Brain scans show this area lights up 27% more when you think you’re taking a brand-name drug, even if it’s just a placebo. That increased activity leads to real, measurable pain reduction. It’s not imagination. It’s neurobiology. The effect is strongest with painkillers, antidepressants, and statins. In one study, patients on generic sertraline were 22% more likely to quit taking it because they felt it "wasn’t working," even though blood tests showed the same levels as the brand name. Another study found that when people were told they were switching to a cheaper generic statin, they reported muscle pain at nearly four times the rate of those who weren’t told. That’s the nocebo effect-the flip side of the placebo effect-where negative expectations make side effects worse.Cost Changes Your Experience
Price matters-even when it shouldn’t. In a famous experiment, healthy volunteers were given fake painkillers. Half were told the pill cost $2.50. The other half were told it cost $0.10. Both pills were identical. The $2.50 pill reduced pain by 64% more than the cheap one. The brain equates price with quality. And in the real world, when a $4.83 brand-name pill becomes a $0.08 generic, your brain doesn’t automatically recalibrate. It wonders: "Why is this so cheap? Is it weaker?" This isn’t just about perception. It’s about behavior. People who switch to generics are 18% less likely to stick with their medication over a year, even when the drug is critical-like for high blood pressure or cholesterol. That drop in adherence leads to more hospital visits, more complications, and higher long-term costs. The irony? The money you save on the pill might cost you more in emergency care.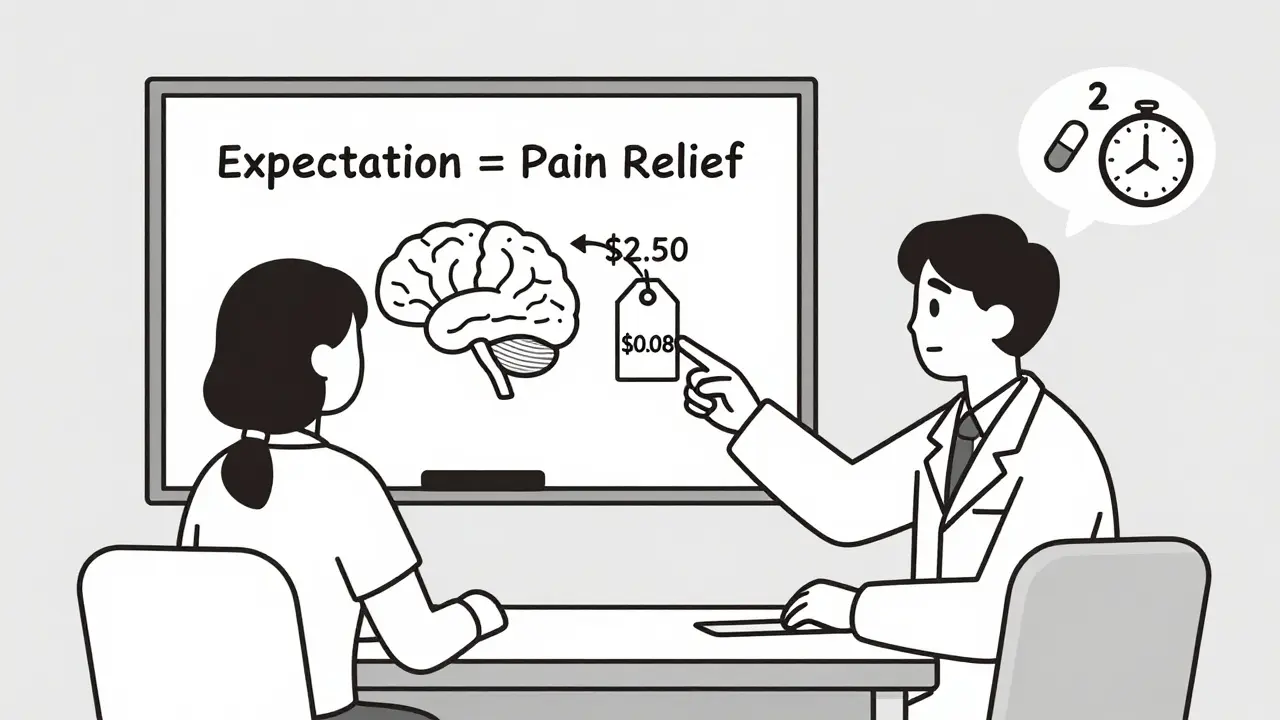
What Doctors and Pharmacies Are Doing About It
Healthcare providers are starting to catch on. A 2021 study showed that a simple three-part conversation before switching to a generic can reduce negative reactions by nearly half. The key points:- "This generic is required by the FDA to work exactly like the brand name. It has the same active ingredient, same dose, same safety profile."
- "Some people say they feel different at first-not because the medicine changed, but because their brain is used to the old pill’s look or name. That’s normal. It usually passes in a couple of weeks."
- "Let’s check in after two weeks. If you still feel off, we’ll figure out what’s going on."
Real Stories, Real Impact
On forums like Reddit and Drugs.com, people share their experiences. One user wrote: "I switched from brand-name levothyroxine to generic. My TSH jumped from 2.1 to 7.8. My doctor said it was fine, but I felt exhausted, cold, and foggy. I switched back-and I’m fine." Another said: "My psychiatrist warned me that generic sertraline might feel different. I was skeptical-but it did. I felt numb. I went back to the brand." But here’s the flip side: many people never know they switched. When pharmacists dispense generics without telling patients, satisfaction rates stay above 80%. The problem isn’t the drug. It’s the message. One case report in the Journal of Clinical Psychopharmacology described a patient who stopped taking generic escitalopram after feeling "worse anxiety." Blood tests confirmed identical drug levels to the brand name. The only difference? The pill looked different. The patient’s brain had already decided it wouldn’t work.
What You Can Do
If you’ve been switched to a generic and feel like it’s not working:- Don’t assume it’s broken. Give it two weeks. Your brain needs time to adjust.
- Check your symptoms. Are you feeling worse physically-or just less confident? Sometimes it’s the latter.
- Talk to your doctor. Say: "I switched to the generic, and I’m not feeling the same. Can we talk about whether this is psychological or physical?"
- Ask if you can try the brand again-just for a short time-to see if your body responds differently.
- Don’t stop cold. Tapering or switching back needs medical guidance.
- Ask for a copy of the FDA’s "Generic Drugs: Same Medicine, Different Price" guide. It’s clear, free, and helps reframe your thinking.
- Request that your pharmacist keep the same pill shape and color if possible.
- Write down how you feel before and after the switch. Numbers help. (Example: "Headaches: 8/10 before, 6/10 after-still better than before I started.")
The Bigger Picture
The U.S. spends $1.4 billion a year on unnecessary brand-name prescriptions because of this psychological gap. That’s billions of dollars that could go toward better care, better access, better outcomes. But it’s not just about money. It’s about trust in medicine. The solution isn’t to hide the switch. It’s to explain it. To normalize the fact that your brain plays a role in how medicine works. To say: "Yes, this pill looks different. Yes, you might feel a little off at first. But it’s the same medicine. Your body just needs a moment to catch up." The future is here. A digital tool called the "Expectation Modulation Protocol"-a 12-minute video and quiz-is currently under FDA review. Early trials show it cuts nocebo responses by over half. Imagine a simple app you open before switching meds. It walks you through what to expect. It tells you: "This is normal. This will pass. You’re not crazy." That’s not magic. That’s medicine catching up with the mind.What’s Next?
The European Union is spending €2.4 million to create standardized patient education for generics across 27 countries. The FDA is piloting stricter rules on pill appearance. Doctors are being trained to talk about expectations-not just doses. But change starts with you. If you’ve ever felt a generic didn’t work, you’re not alone. You’re not wrong. Your experience is real. But now you know why. And you know what to do next.Do generic drugs work the same as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. The FDA requires them to be bioequivalent-meaning they work in the body the same way, with the same absorption rate and effectiveness. The only differences are inactive ingredients (like fillers or dyes), packaging, and price.
Why do I feel different on a generic medication?
You’re not imagining it. The difference is psychological, not chemical. Your brain associates the brand-name pill’s color, shape, or name with effectiveness. When that changes, your brain may lower its expectation of relief-leading to a weaker placebo effect. This is called the nocebo effect. It’s real, measurable, and temporary for most people. Give it two weeks. If symptoms persist, talk to your doctor.
Can the placebo effect make a generic drug actually work better?
Yes. Studies show that when patients believe they’re taking a brand-name drug-even if it’s a placebo-they report stronger pain relief and fewer side effects. This isn’t tricking the body. It’s activating natural pain-relief pathways in the brain. The same mechanism works in reverse: believing you’re on a cheap generic can reduce your body’s natural response to the medicine.
Should I ask my doctor to keep me on the brand-name drug?
If you’ve tried the generic and truly feel worse after two weeks, yes. But don’t assume it’s the drug. Ask your doctor to help you distinguish between a real medical issue and a psychological response. Sometimes, switching back temporarily can help reset your expectations. Many patients find that once they understand the science, they can successfully stay on the generic.
Are there any medications where generics really are different?
For most drugs, no. But for medications with a narrow therapeutic index-like warfarin, levothyroxine, or some seizure drugs-the body is very sensitive to small changes in absorption. Even within the FDA’s acceptable bioequivalence range (80-125%), some patients may respond differently. That’s why doctors sometimes monitor blood levels closely when switching. But even here, the difference is usually small and manageable-not a reason to avoid generics entirely.
How can I avoid the nocebo effect when switching to generics?
First, don’t assume the worst. Ask your pharmacist or doctor to explain the switch before it happens. Request the same pill shape and color if possible. Give yourself two weeks to adjust. Track your symptoms objectively. And remember: if you feel better after switching, that’s not luck-it’s your brain learning to trust the new version.
Managing the psychological side of generics isn’t about convincing people to ignore their feelings. It’s about helping them understand where those feelings come from-and giving them the tools to move past them. The science is clear. The solution is simple. The question is: will we start treating the mind as part of the medicine?




Comments
14 Comments
steve rumsford
i switched to generic lisinopril last year and thought i was gonna die. turned out i just needed to stop staring at the damn pill like it owed me money.
Anastasia Novak
Oh honey. You think this is about psychology? Let me introduce you to the real villain: Big Pharma’s marketing budget. They spent $2 billion last year convincing you that a blue pill is spiritually superior to a white one. The placebo effect? That’s just capitalism wearing a lab coat.
LALITA KUDIYA
i tried generic thyroxine and felt like a zombie for 3 days... then i realized i was just stressed. my brain was screaming "this isn't the pill i know!" but my body was fine 😊
Poppy Newman
this is why i always ask for the exact same generic brand - same color, same shape. my brain needs visual continuity like my coffee needs sugar 🤷♀️
Ayodeji Williams
yo but what if the generic is just bad? like i took some indian generic and my legs went numb. doctor said it was "psychological" but i swear it was the fillers. we dont even know what's in these pills anymore 😭
Kyle King
they're lying. the FDA lets generics be 20% weaker. they just say "bioequivalent" so you don't panic. they're selling you a ghost pill and calling it science. watch the documentary "Pill Shadows" - it's all connected to the vaccine agenda.
Aparna karwande
You people are so obsessed with pills you forget the real truth: the West has brainwashed you into believing a logo is medicine. In India, we’ve been taking generics since the 1970s. We didn’t need a $2.50 placebo to feel better. We had community, discipline, and no corporate branding. Your weakness isn’t biology-it’s consumerism.
Jonathan Larson
The phenomenon described here is not merely psychological; it is neurobiological, epistemological, and sociological in nature. The human organism, conditioned by decades of pharmaceutical branding, has developed a conditioned response to visual and lexical cues associated with efficacy. This is not a flaw-it is an adaptive mechanism that has been hijacked by market forces. The solution, therefore, lies not in suppressing patient perception, but in re-engineering the context of care to align expectation with evidence. A paradigm shift is required.
Vince Nairn
so you're telling me i paid $400 for a blue pill because my brain needed a pep talk? and now i'm supposed to feel guilty for wanting my trust back? lol. sure. i'll just take this white pill and pretend i'm not being scammed. 🙄
Emma Addison Thomas
I’ve been on generics for 12 years. I never noticed a difference. But then again, I don’t stare at my pills. I take them. I live my life. Maybe the problem isn’t the pill-it’s how much attention we give it.
Christine Joy Chicano
The most fascinating part? The brain doesn’t just *expect* relief-it *manufactures* it. Dopamine, endorphins, cortisol modulation-all triggered by belief. This isn’t placebo. It’s psychophysiology. And if we can harness this for generics, imagine what we could do with chronic pain, depression, even autoimmune conditions. The future of medicine isn’t in new molecules-it’s in narrative design.
Mina Murray
You think this is about branding? Look at the patent cliffs. The same companies that make brand-name drugs own the generics. They change the shape just to make you panic so you’ll pay more. It’s a trap. They want you addicted to the *idea* of the pill, not the chemistry. I’ve seen the internal memos. They call it "the placebo profit loop."
Anthony Capunong
This is why America is weak. We cry because our pills changed color. In Russia, they take whatever’s in the vial. No labels. No names. Just medicine. We need to stop treating our bodies like toddlers who need a teddy bear to sleep.
Kamlesh Chauhan
generic sertraline made me feel like a ghost. i went back to brand. doctor said "its all in your head". well yeah. and my head is the only thing keeping me alive. so yeah i'll take the blue one thanks
Write a comment