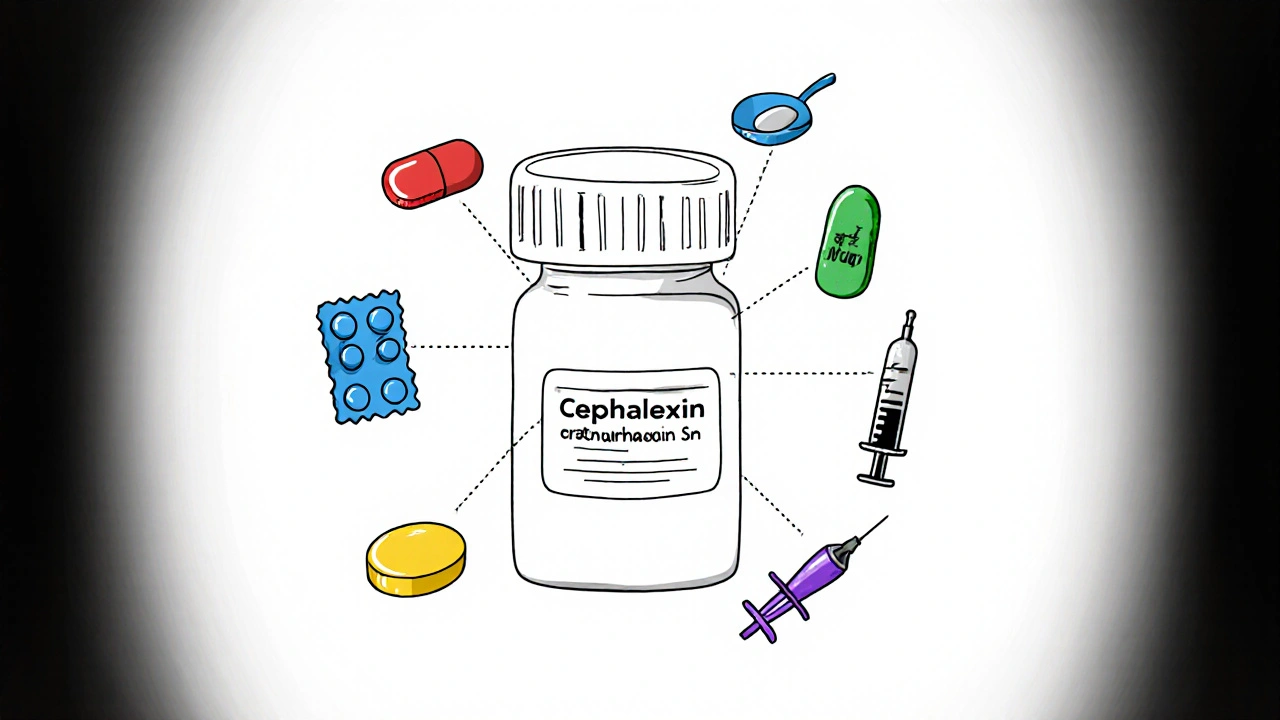
Cephalexin is a first‑generation beta‑lactam antibiotic used to treat skin, ear, bone and urinary‑tract infections. While it’s generally well‑tolerated, cephalexin interactions can turn a routine prescription into a safety issue if you’re also taking certain other drugs.
Key Takeaways
- Warfarin, oral contraceptives, and certain antacids can change how cephalexin works in your body.
- Live vaccines may become less effective when you’re on this antibiotic.
- Timing matters - space out some meds by at least two hours.
- Always tell your prescriber about supplements, over‑the‑counter meds, and alcohol use.
- Monitoring blood tests (e.g., INR for warfarin) can catch problems early.
How Cephalexin Works
Cephalexin halts bacterial growth by binding to penicillin‑binding proteins, which disrupts cell‑wall synthesis. Because it’s a beta‑lactam, it shares metabolic pathways with other penicillins and cephalosporins, making cross‑reactivity a key consideration when you’re on multiple drugs.
Medication Classes That Often Interact
The most common culprits fall into a few groups: anticoagulants, hormonal contraceptives, diabetes meds, antacids, and certain vaccines. Below we dive into each, explain what the interaction looks like, and give practical advice.
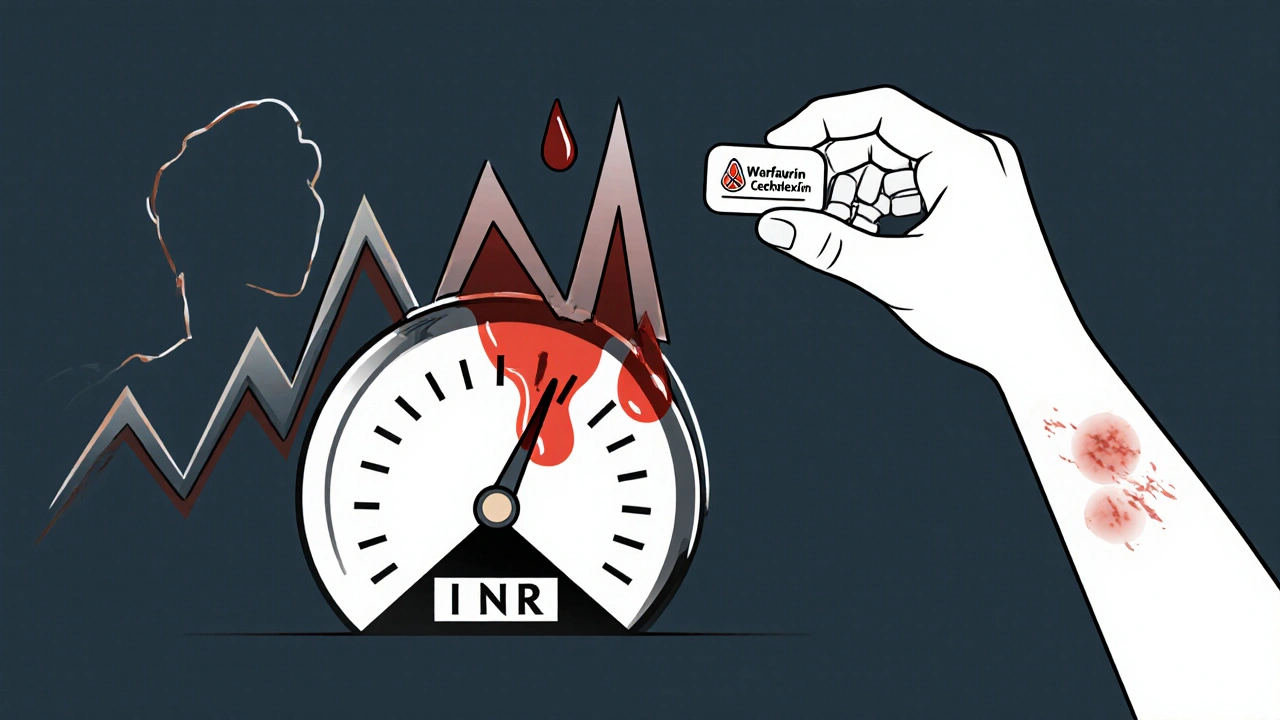
Warfarin (Blood Thinner)
Warfarin is an oral anticoagulant that works by inhibiting vitamin K‑dependent clotting factors can become more potent when taken with cephalexin. The antibiotic may reduce gut flora that normally produce vitamin K, raising the International Normalized Ratio (INR) and increasing bleeding risk.
- Watch for bruising, nosebleeds, or unusually dark urine.
- Ask your doctor to check INR more frequently during the first week of therapy.
- If INR spikes, dosage adjustments of warfarin may be needed.
Oral Contraceptives
Oral contraceptives contain estrogen and/or progestin to prevent ovulation rely on entero‑hepatic recirculation. Cephalexin can interrupt this loop by altering gut bacteria, potentially lowering hormone levels and raising the chance of an unintended pregnancy.
- Use a backup method (condoms, diaphragm) for at least 7 days after starting cephalexin.
- Consider non‑hormonal birth control options if you anticipate long‑term antibiotic use.
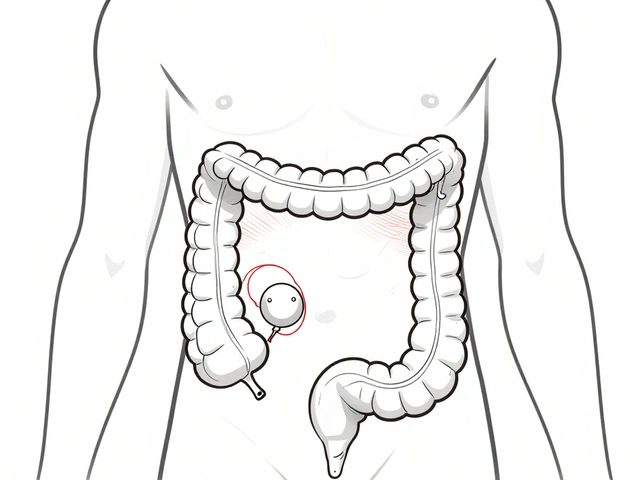
Metformin (Diabetes Medication)
Metformin is a first‑line oral agent for type 2 diabetes that lowers hepatic glucose production is cleared by the kidneys. Cephalexin can cause a modest rise in serum creatinine, which may reduce metformin clearance and increase the risk of lactic acidosis.
- Check kidney function before starting cephalexin if you’re on metformin.
- Temporarily hold metformin on the day of a high‑dose IV cephalexin or if you develop severe diarrhea.
Antacids Containing Aluminum or Magnesium
Antacids such as Maalox or Mylanta bind to cephalexin in the stomach, lowering its absorption by up to 30 %.
- Take cephalexin at least two hours before or after an antacid.
- Consider a calcium‑based antacid, which has less impact on absorption.
Probenecid (Uric Acid‑Lowering Agent)
Probenecid inhibits renal tubular secretion of organic acids, raising plasma levels of certain antibiotics was historically used to boost penicillin levels. With cephalexin, it can increase drug concentrations, potentially leading to toxicity (e.g., seizure risk).
- Avoid concurrent use unless specifically ordered for a short‑term boost.
- If needed, a dose‑reduction of cephalexi n is recommended.
Live Vaccines
Cephalexin’s antibacterial activity can blunt the immune response to live vaccines such as measles‑mumps‑rubella (MMR) or yellow fever. The vaccine may not generate sufficient antibodies, leaving you unprotected.
- Schedule vaccinations at least two weeks before starting the antibiotic, or postpone the vaccine until after finishing the course.
Alcohol
There’s no direct pharmacokinetic clash, but both cephalexin and alcohol can irritate the stomach lining. Mixing them often leads to nausea, vomiting, and reduced adherence to the antibiotic regimen.
- Limit alcohol intake while completing the prescription to avoid gastrointestinal upset.
Non‑Steroidal Anti‑Inflammatory Drugs (NSAIDs) - Example: Ibuprofen
Ibuprofen is an NSAID that reduces inflammation and pain by inhibiting cyclooxygenase enzymes and other NSAIDs can amplify the risk of kidney injury when paired with cephalexin, especially in dehydration or pre‑existing renal disease.
- Stay well‑hydrated and monitor urine output.
- Consider acetaminophen for mild pain if kidney function is a concern.
Quick Reference Table of Common Interactions
| Medication | Interaction Type | Potential Effect | Management |
|---|---|---|---|
| Warfarin | Pharmacodynamic ↑ INR | Bleeding | Frequent INR checks; dose adjustment |
| Oral contraceptives | Reduced entero‑hepatic recirculation | Contraceptive failure | Use backup barrier method |
| Metformin | Renal clearance ↓ | Lactic acidosis risk | Check creatinine; hold if renal function worsens |
| Antacids (Al/ Mg) | Absorption ↓ | Reduced efficacy | Separate dosing by ≥2 h |
| Probenecid | Clearance ↓ | Higher cephalexin levels → toxicity | Avoid co‑administration or lower dose |
| Live vaccines | Immune response ↓ | Insufficient immunity | Vaccinate before starting antibiotic |
| Alcohol | GI irritation ↑ | Nausea, vomiting | Limit intake during therapy |
| Ibuprofen/NSAIDs | Renal stress ↑ | Acute kidney injury | Hydrate; consider alternative analgesics |
Practical Tips to Prevent Problems
- Bring a current medication list to every appointment - include vitamins and herbal supplements.
- Ask your pharmacist if any over‑the‑counter product might bind cephalexin.
- Space dosing: take cephalexin at least two hours before/after antacids, iron, or calcium supplements.
- Monitor specific labs:
- INR for warfarin users.
- Serum creatinine for diabetics on metformin.
- Report new symptoms (e.g., unusual bruising, dark urine, severe diarrhea) to your clinician immediately.
Frequently Asked Questions
Can I take ibuprofen with cephalexin?
Short‑term use is generally safe, but both drugs can stress the kidneys. If you have kidney disease or are dehydrated, choose acetaminophen instead, and stay well‑hydrated.
Do I need to stop my birth control while on cephalexin?
You don’t have to stop it, but add a reliable backup method (condom, diaphragm) for at least a week after beginning the antibiotic.
Is it safe to drink alcohol while taking cephalexin?
Alcohol doesn’t change the drug’s metabolism, but it can worsen stomach upset and make you feel sick, which may lead you to skip doses. Keep drinking to a minimum until you finish the course.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one - don’t double up.
Can antacids affect how well cephalexin works?
Yes. Aluminum‑ or magnesium‑based antacids can bind the antibiotic and cut absorption by up to a third. Take them two hours apart.
Do I need blood tests while on cephalexin?
Most people don’t, but if you’re on warfarin, metformin, or have kidney disease, your doctor will likely check INR or kidney function during therapy.


Comments
13 Comments
Grace Silver
Never thought antibiotics could mess with birth control, thanks for the heads‑up!
Tamara Tioran-Harrison
One would have expected a modest cephalosporin to remain innocuous, yet the pharmaco‑dynamic intricacies betray that naïve optimism. The sheer audacity of a simple drug to meddle with hormonal equilibrium is almost poetic, is it not? :)
Brett Witcher
While the overview of cephalexin's interactions appears comprehensible at first glance, a deeper inspection reveals several nuances that merit attention. The interaction with warfarin, for instance, is not merely a marginal increase in INR but a clinically significant potentiation of anticoagulant effect due to altered gut flora. This reduction in vitamin K synthesis can precipitate hemorrhagic complications in susceptible individuals. Consequently, clinicians should schedule more frequent INR monitoring during the initial phase of concurrent therapy. Regarding oral contraceptives, the disruption of entero‑hepatic recirculation by cephalexin can diminish estrogenic levels enough to compromise contraceptive efficacy. Patients are therefore advised to employ a reliable barrier method for a minimum of one week following antibiotic initiation. The impact on metformin is similarly noteworthy; cephalexin‑induced elevations in serum creatinine may impair renal clearance and raise the specter of lactic acidosis. A precautionary assessment of renal function before commencing therapy is advisable. Antacids containing aluminum or magnesium represent another class of agents that can bind cephalexin, reducing its bioavailability by up to thirty percent. Separation of dosing intervals by at least two hours mitigates this effect and preserves therapeutic plasma concentrations. Probenecid, historically employed to augment penicillin levels, now poses a risk of cephalexin toxicity due to diminished renal excretion. Dose adjustment or avoidance is prudent when co‑administration is contemplated. Live attenuated vaccines may elicit a suboptimal immune response if administered contemporaneously with cephalexin, thus scheduling immunizations prior to antibiotic therapy is recommended. Although alcohol does not alter the pharmacokinetics of cephalexin, the combined gastric irritation can reduce patient adherence to the regimen. Finally, non‑steroidal anti‑inflammatory drugs, particularly ibuprofen, may exacerbate renal stress under conditions of dehydration, warranting careful monitoring of renal function and fluid intake. In summary, the presence of these interactions underscores the necessity of a comprehensive medication reconciliation and patient education when prescribing cephalexin.
Bianca Larasati
Picture this: you’ve got a nasty infection, you pop a cephalexin, and suddenly you’re juggling blood thinners, birth control, and even your morning coffee! It can feel like a high‑stakes juggling act, but fear not-knowledge is your safety net. By spacing your meds, keeping an eye on lab results, and having a backup plan for contraception, you stay in control. Stay hydrated, stay informed, and you’ll ride this wave like a champion!
Abhinav B.
Bro, in India we often mix meds without thinking, so this info hit me hard. Make sure you tell the doc if you are on ayurvedic herbs too – they can also play with cephalexin. And dont forget to take the antibiotic atleast two hrs apart from antacids, otherwise you r wasting it. Keep an eye on any weird bruises, especially if you r on warfarin. Stay safe fam!
Abby W
OMG, I totally forgot about the vaccine thing 😱! If you’re getting your flu shot, make sure it’s not the same week you start cephalexin. Also, don’t be shy about asking your pharmacist to double‑check any over‑the‑counter stuff – they’re the real MVPs 🏆. Stay on top of those INR checks, and you’ll be golden ✨.
Lisa Woodcock
I understand how overwhelming medication lists can feel, especially when antibiotics join the party. It’s reassuring to know that a simple step like separating doses by a couple of hours can make a big difference. If you’re unsure about any supplement, a quick chat with your pharmacist can clear things up. Remember, you’re not alone in navigating these interactions.
krishna chegireddy
It’s not a coincidence that big pharma loves to hide these tiny details. They want you to think a pill is harmless, while they profit from the chaos when something goes wrong. Trust your gut, read the fine print, and demand transparency. Otherwise you’ll keep being a pawn in their game.
Tamara Schäfer
Wow, this really opens my eyes to how many hidden connections there are between meds. It’s kinda scary but also empowering knowing we can take small steps to stay safe. I’ll definitely double‑check my med list next time and tell my doc about any over‑the‑counter stuff. Feeling more confident already!
kevin burton
For patients using warfarin, increasing the frequency of INR testing to every three days during the first week of cephalexin therapy is advisable. Those on metformin should have serum creatinine measured before starting the antibiotic, and consider holding metformin if creatinine rises significantly. Antacids should be taken at least two hours before or after cephalexin to avoid reduced absorption. These steps help mitigate the most common interactions.
Max Lilleyman
Honestly, if you’re not checking your INR or kidney labs, you’re playing Russian roulette with your health 😬. Staying on top of these simple checks is not optional – it’s basic responsibility.
Buddy Bryan
Listen up: you can’t afford to be sloppy with drug combos. Stop ignoring the timing guidelines, set alarms, and log every dose. When you’re on a blood thinner, the cost of a missed interaction is bleeding out. Get organized now or suffer later.
Jonah O
They don’t want you to know that the real danger is the hidden data they collect when you report side effects. Every lab result is fed back into a system that predicts your next prescription. Stay skeptical and keep your info private.
Write a comment