When your lower left belly suddenly feels like it’s been stabbed with a hot knife, and you can’t stand up straight, it’s not just gas. It could be diverticulitis-inflamed pouches in your colon that turn from harmless bumps into painful infections. This isn’t rare. By age 60, more than half of people in the U.S. have these pouches. Most never know they’re there. But when they get infected, it hits hard.
What Exactly Are Diverticula?
Diverticula are small, balloon-like sacs that push out through weak spots in the colon wall. Think of them like tiny bulges in an old tire. They form over years, often because of low-fiber diets that force the colon to work harder. The pressure builds, and the wall gives way. These pouches are usually 5 to 10 millimeters wide-small enough to slip past notice.Over 95% of them show up in the sigmoid colon, the last curve before the rectum. That’s why pain is almost always in the lower left side. But in Asian populations, it’s more common on the right. Why? Because colon anatomy differs slightly across ethnic groups. The pouches themselves aren’t the problem. It’s when they get blocked by stool or bacteria that things go wrong.
How Do You Know It’s Diverticulitis and Not Something Else?
Many people mistake diverticulitis for IBS, appendicitis, or even ovarian cysts. But there are clear signs that set it apart.- Sharp, constant pain in the lower left abdomen-not crampy, not coming and going
- Fever above 38°C (100.4°F)-present in 70-80% of cases
- White blood cell count over 11,000
- Pain that gets worse when you move or cough
IBS feels more like bloating and irregular bowel habits without fever. Appendicitis starts near the navel and moves to the lower right. Ovarian cysts can mimic the pain, especially in women, but they don’t cause fever or elevated white blood cells. A CT scan is the gold standard for diagnosis-it shows the inflamed pouches and whether there’s an abscess or perforation.
But here’s the catch: 25% of cases get misdiagnosed the first time. People go to the ER, get told it’s just constipation, and come back days later worse off. On average, it takes 3.2 days to get the right diagnosis. That delay increases risk.
How Severe Is It? The Hinchey Stages
Not all diverticulitis is the same. Doctors use the Hinchey system to classify severity:- Stage Ia: Tiny abscess near the colon, less than 3cm
- Stage Ib: Larger abscess, 3-5cm
- Stage II: Abscess in the pelvis
- Stage III: Pus leaking into the belly cavity
- Stage IV: Fecal matter leaks out-this is life-threatening
Most people (80%) fall into Stage I. These are the cases where you might not even need to go to the hospital. But if you’re in Stage III or IV, you’re in emergency territory. Surgery becomes urgent.

Antibiotics: Still Necessary?
Ten years ago, every case got antibiotics. Now? Not so much.The old rule was simple: infection = antibiotics. But a major 2021 study called the DIVERT trial changed everything. It compared patients treated with antibiotics to those treated with fluids, rest, and pain relief. The results? No difference in recovery time. Both groups healed in about 7 days.
So now, doctors follow a smarter approach:
- If you have mild symptoms, no fever, normal bloodwork-skip antibiotics. Just rest, drink fluids, eat clear liquids for a couple days.
- If you have fever above 38.5°C, high white blood cells, or are over 65-antibiotics are still recommended.
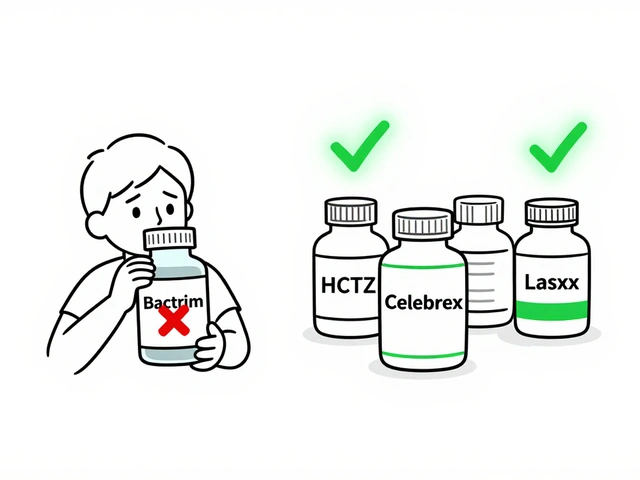
Common antibiotics include amoxicillin-clavulanate (Augmentin) for mild cases. For hospital stays, piperacillin-tazobactam (Zosyn) is used intravenously. The shift away from routine antibiotics isn’t just about saving pills-it’s about stopping antibiotic resistance before it gets worse.
What to Eat When You’re Sick-and After
For the first 48 to 72 hours during a flare-up, stick to clear liquids: water, broth, apple juice, gelatin. No solids. Your colon needs to rest.After that, slowly add low-fiber foods: white rice, eggs, skinless chicken, mashed potatoes. No whole grains, nuts, seeds, or raw veggies yet. That’s not because they cause diverticulitis-they don’t. It’s because they’re harder to digest when your colon is inflamed.
Here’s the big myth busted: nuts, seeds, and popcorn don’t cause diverticulitis. A 18-year study of 47,000 women found no link at all. In fact, those who ate more nuts had fewer attacks. The old warning came from a time when doctors didn’t understand how the colon worked.
After recovery, the real fix is fiber. Aim for 30-35 grams daily. That’s:
- 1 cup cooked lentils (15g)
- 1 medium pear (6g)
- 1 cup oats (4g)
- 1 cup broccoli (5g)
- 1 slice whole wheat bread (2g)
People who hit that target cut their risk of a second attack by nearly half. One man on a health forum went from 3 attacks in 2 years to none for 27 months after switching to 35g of fiber a day.
When Surgery Might Be Needed
Most people never need surgery. But if you’ve had two or more attacks that landed you in the hospital, your doctor might suggest removing the affected part of the colon. That’s a big change from 5 years ago, when doctors waited for three attacks.Why the shift? Because between attacks, many people live with constant discomfort-bloating, cramps, fear of the next flare-up. One study found 40% of patients with multiple episodes had major activity limits. Quality of life matters as much as survival.
For complicated cases (Stage III), surgeons now often do laparoscopic lavage-cleaning out the belly instead of removing the colon. It works 82% of the time in contained infections. Resection (removing the colon) is still used for Stage IV or if there’s a hole.

What You Can Do to Prevent Another Attack
Prevention isn’t about avoiding seeds or being scared of fiber. It’s about three things:- Get enough fiber-30-35 grams daily. If you can’t get it from food, try psyllium husk (Metamucil) or methylcellulose (Citrucel).
- Stay active-people who exercise less than 2 hours a week have 38% higher risk. Walking 30 minutes a day helps.
- Don’t smoke-smokers are 2.7 times more likely to get diverticulitis.
Obesity also doubles your risk. Losing even 10 pounds can make a difference.
And yes, you still need a colonoscopy 6 to 8 weeks after your first attack-especially if you’re over 50. About 1.3% of cases turn out to be colon cancer hiding behind diverticulitis symptoms. Better safe than sorry.
New Hope: Drugs and AI
There’s new science on the horizon. In 2023, the FDA approved mesalazine (Pentasa) for long-term use to reduce recurrence. In trials, it cut attacks by 31% over a year compared to placebo.Mayo Clinic is using AI to predict who’s likely to have another flare-up. The algorithm looks at your CT scan, blood tests, age, and BMI-and predicts risk with 83% accuracy. That means doctors can now target high-risk patients with preventive meds before they get sick again.
Researchers are also studying gut bacteria. People with diverticulitis often have low levels of Faecalibacterium prausnitzii-a good bug that calms inflammation. Future treatments might involve probiotics or even fecal transplants.
Real Stories, Real Impact
On Reddit, one user wrote: “I missed three weeks of work during my first attack. Bloodwork was normal. No one believed me.” Another said: “The pain felt like hot knives stabbing me over and over.”These aren’t exaggerations. Diverticulitis is brutal when it hits. But it’s also manageable. Most people recover fully. Many never have another attack. The key is not panic-it’s knowledge.
Don’t wait for the next flare-up to learn what works. Start eating more fiber now. Move more. Quit smoking if you can. And if you’re ever in doubt about abdominal pain-get it checked. Early diagnosis saves you from emergency surgery and months of pain.
Can diverticulitis go away without antibiotics?
Yes, in mild, uncomplicated cases, diverticulitis can resolve on its own with rest, hydration, and a clear liquid diet. Studies like the 2021 DIVERT trial show no difference in recovery time between patients treated with antibiotics and those treated without. Antibiotics are now reserved for cases with fever above 38.5°C, high white blood cell counts, or in older adults.
Is it safe to eat nuts and seeds with diverticulitis?
Yes. The old advice to avoid nuts, seeds, and popcorn is outdated and incorrect. A major 18-year study of 47,000 women found no link between eating these foods and increased diverticulitis risk. In fact, those who ate more nuts had fewer flare-ups. During an active flare-up, you may need to avoid them temporarily for easier digestion, but they don’t cause the condition.
How long does a diverticulitis attack last?
Mild cases usually improve within 48 to 72 hours with rest and fluids. Full recovery, including returning to a normal diet, typically takes 7 to 10 days. More severe cases requiring hospitalization may take 10 to 14 days or longer, especially if surgery or drainage is needed. Recovery time depends on severity, age, and overall health.
When should I see a doctor for abdominal pain?
See a doctor immediately if you have sudden, severe lower left abdominal pain, fever above 38°C, vomiting, inability to pass gas or stool, or if the pain worsens with movement. These are signs of diverticulitis or possible complications like abscess or perforation. Delaying care increases the risk of serious complications requiring emergency surgery.
Can diverticulitis come back after treatment?
Yes, 15% to 30% of people have a second attack within a few years. Risk is higher if you’re overweight, smoke, have low fiber intake, or have had multiple hospitalizations. After two severe attacks, your doctor may recommend surgery to remove the affected colon section. Long-term fiber intake and lifestyle changes can reduce recurrence by up to 50%.
Do I need a colonoscopy after diverticulitis?
Yes, doctors recommend a colonoscopy 6 to 8 weeks after an attack, especially if you’re over 50. This is to rule out colon cancer, which can mimic diverticulitis symptoms. Studies show about 1.3% of patients over 50 have cancer found during this follow-up exam. Even if symptoms clear, the scan is important for safety.



Comments
8 Comments
Joe Lam
Look, if you're still prescribing antibiotics for uncomplicated diverticulitis like it's 2012, you're not just outdated-you're contributing to the global antibiotic apocalypse. The DIVERT trial wasn't some blog post, it was a randomized controlled study with 1,200 patients. We've known for years that inflammation doesn't equal infection. Yet here we are, watching primary care docs still reach for amoxicillin like it's a magic bullet. Stop treating the colon like a dirty sink you need to flush with drugs.
jagdish kumar
Everything burns. Even fiber. Even silence. We are all just temporary sacks of bacteria trying not to rupture.
zac grant
Big win for evidence-based medicine here. The shift away from routine antibiotics is one of the most underappreciated changes in GI care over the last decade. For mild Hinchey Ia/Ib cases, watchful waiting + hydration + low-residue diet is not just non-inferior-it's superior in terms of microbiome preservation. And yes, nuts are safe. The 2016 JAMA study with 47K women remains the definitive evidence. Also, psyllium > methylcellulose for long-term compliance-better stool consistency, less bloating. Pro tip: aim for 35g fiber via whole foods first, supplements only as a bridge. And for God’s sake, get that colonoscopy. Missed CRC masquerading as diverticulitis is a real thing.
Pavan Kankala
They don't want you to know this, but diverticulitis was invented by Big Pharma to sell antibiotics and colonoscopies. The real cause? Glyphosate in your bread, 5G radiation weakening your colon walls, and the government's secret agenda to keep people docile with chronic pain. You think they want you healthy? They want you on Metamucil forever so you keep buying it. That 'AI prediction model'? It's just a front to collect your biometric data. And the fiber advice? Total distraction. Your body doesn't need '35g'-it needs detox. Juice cleanses, infrared saunas, and raw garlic are what actually heal. The system doesn't want you to know that.
Jessica Baydowicz
YESSSSS to the fiber push!! 🙌 I used to get flare-ups every 6 months like clockwork-then I started snacking on almonds, chia seeds, and lentil soup like it was my job. Two years zero attacks. Also, walking after dinner? Non-negotiable. I used to sit on the couch like a potato after work-now I’m pacing while scrolling TikTok and my colon is thriving. It’s not magic, it’s just… basic human maintenance. You don’t need to be a saint, just consistent. And yes, nuts are your friends. Eat them like they’re going out of style. 💪
John Filby
Just had my first attack last month-no antibiotics, just broth and rest for 3 days. Felt like a zombie, but I recovered fine. I’m now eating oatmeal every morning and taking Metamucil like it’s my religion 😅. Anyone else notice how much better you feel when you’re not constipated? Like… your whole body sighs? Also, is it just me or does everyone ignore the exercise part? I started walking 20 min after dinner and my bloating dropped off a cliff. Small changes, big wins.
Rachel Bonaparte
Let’s be real-this whole ‘fiber fixes everything’ narrative is a corporate wellness fantasy designed to sell psyllium husk and whole grain bread. The real issue? Chronic low-grade inflammation from processed foods, glyphosate residues, and the fact that modern humans haven’t evolved to digest modern diets. The fact that 80% of cases are Stage I doesn’t mean it’s benign-it means we’re ignoring the root cause. And don’t get me started on the colonoscopy push. How many times do we need to be reminded that cancer can hide behind diverticulitis? Because I’ve read the studies-they’re funded by GI device manufacturers. The real solution? Fasting. Intermittent fasting resets the microbiome. No one wants to talk about that because it doesn’t come in a pill bottle. And yes, I know I sound dramatic. But I’ve seen people get misdiagnosed, overmedicated, and then told to ‘eat more broccoli.’ It’s not helpful. It’s negligent.
Scott van Haastrecht
So let me get this straight-we’ve got a system where doctors are told to withhold antibiotics, but if you show up with fever and a WBC of 15k and they don’t give you cipro, you’re the one who gets sued? Meanwhile, the same docs who say ‘rest and fluids’ are the ones who send you home with a prescription for Tylenol and a pat on the back. This isn’t patient-centered care, it’s cost-cutting dressed up as science. And now they’re using AI to predict who’ll flare next? Brilliant. Let’s just label people as ‘high risk’ and charge them $300/month for supplements while ignoring their sleep, stress, and insulin resistance. This isn’t medicine. It’s a business model. And you’re all just cheerleaders for it.
Write a comment