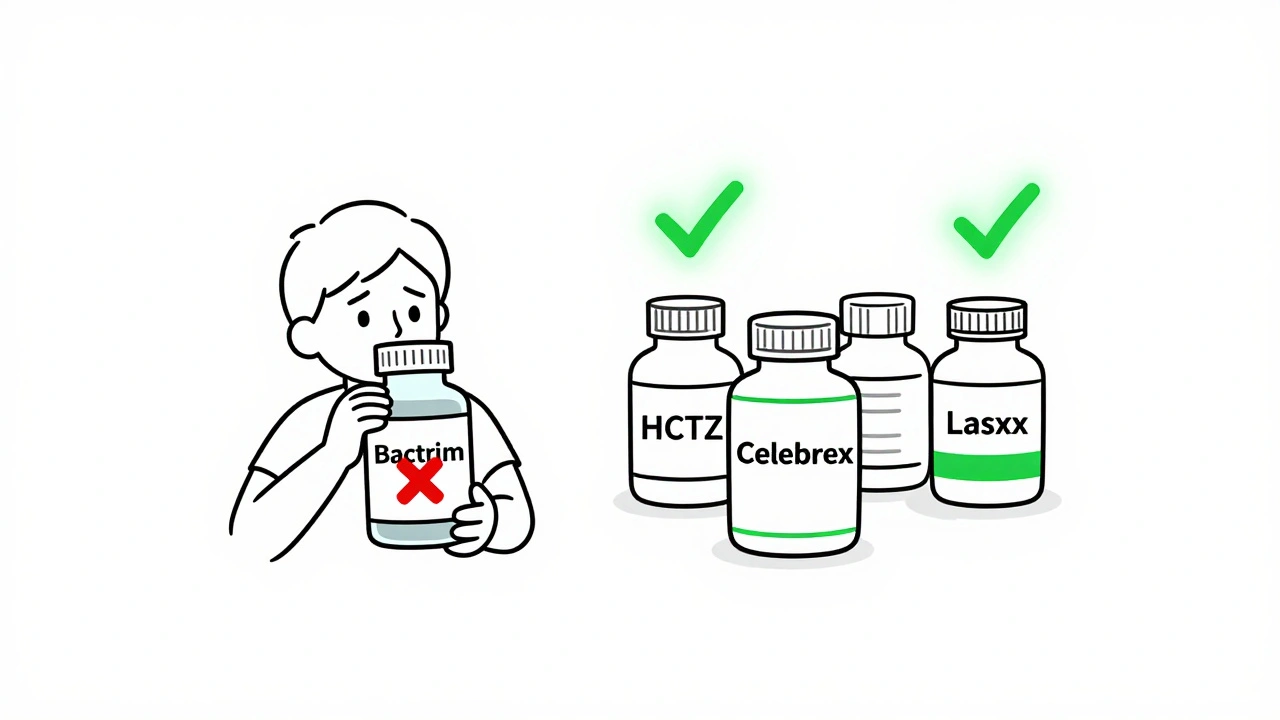
Many people carry a label of "sulfa allergy"-but most don’t know what it actually means. If you’ve been told you’re allergic to sulfa drugs, you might have avoided medications like hydrochlorothiazide for high blood pressure, furosemide for swelling, or celecoxib for arthritis. You might even have been denied a simple antibiotic like Bactrim for a urinary tract infection. But here’s the truth: sulfa allergy doesn’t mean what you think it does.
What Is a Sulfa Allergy, Really?
The term "sulfa allergy" is misleading. It’s not about sulfur. It’s not about sulfites in wine or sulfates in Epsom salts. It’s about a specific group of antibiotics that contain a chemical structure called an arylamine group at the N4 position. These are antimicrobial sulfonamides-drugs like sulfamethoxazole (in Bactrim or Septra), sulfadiazine, and dapsone. These are the only ones that carry a real risk of cross-reactivity with each other. About 3% of people say they’re allergic to sulfa drugs. But studies show only 1.5-2% actually have a true IgE-mediated allergic reaction. The rest? They had a rash, nausea, or a fever after taking the drug-and assumed it was an allergy. Sometimes, it was just a side effect. Other times, it was a viral infection that happened to coincide with the medication. Either way, labeling it as an "allergy" can cost you more than just inconvenience-it can cost you safer, more effective treatment options.Why Most Non-Antibiotic Sulfonamides Are Safe
Not all drugs with "sulfa" in the name are created equal. Take hydrochlorothiazide (HCTZ), a common blood pressure pill. Or furosemide (Lasix), used for fluid retention. Or celecoxib (Celebrex), a popular arthritis medication. These are all sulfonamides-but they lack the arylamine group that triggers immune reactions in people allergic to antibiotic sulfonamides. A 2019 study in the Journal of Allergy and Clinical Immunology: In Practice followed 1,200 patients with confirmed sulfonamide antibiotic allergies. Only 0.8% reacted to non-antibiotic sulfonamides. That’s about the same rate as people with no sulfa allergy at all. The American Academy of Allergy, Asthma & Immunology (AAAAI) confirmed this in their 2023 position statement: "There is no clinically significant immunologic-mediated cross-reactivity between sulfonamide antibiotics and non-antibiotic sulfonamides." The Mayo Clinic’s 2023 data backs this up. Patients with sulfonamide antibiotic allergies who took celecoxib had no higher risk of reaction than the general population. The odds ratio? 1.03. In plain terms: no increased risk.What Medications Should You Avoid?
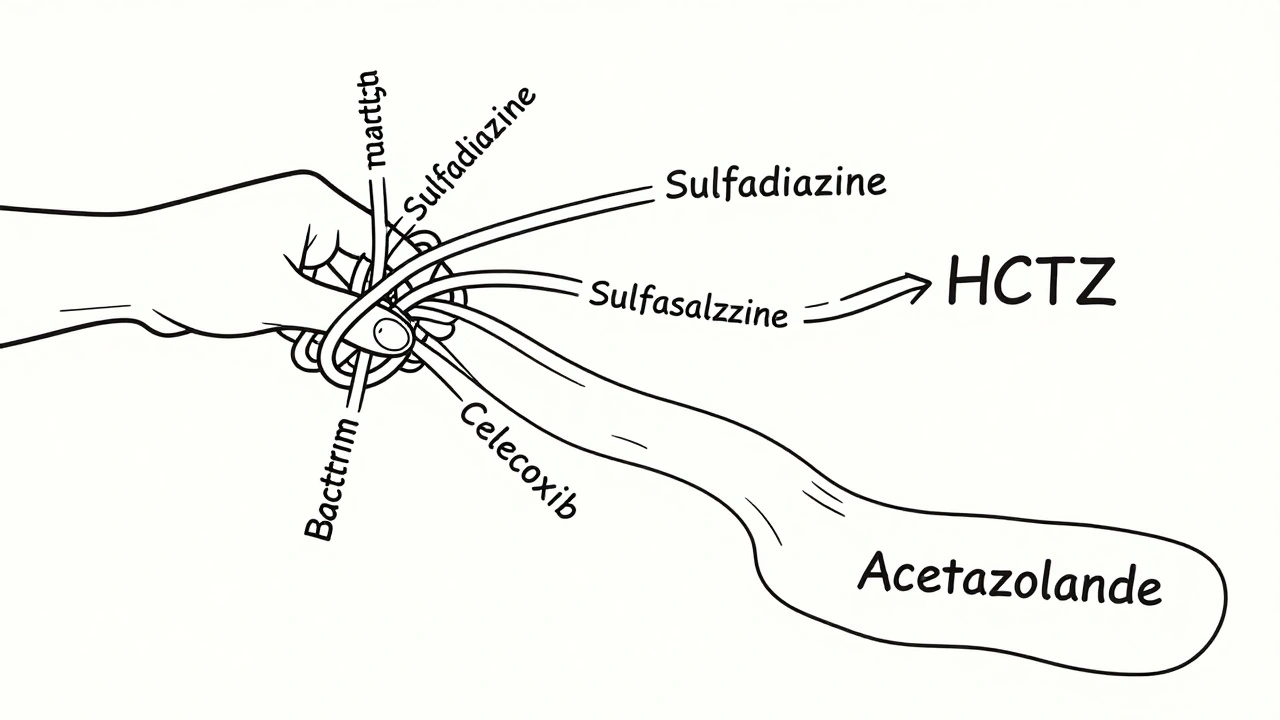
If you have a confirmed allergy to antimicrobial sulfonamides, you should avoid:- Sulfamethoxazole-trimethoprim (Bactrim, Septra)
- Sulfadiazine
- Sulfacetamide (eye drops)
- Dapsone (used for leprosy and certain skin conditions)
What You Can Still Take (Safely)
Here’s the good news: you can likely take these without risk:- Hydrochlorothiazide (HCTZ)
- Furosemide (Lasix)
- Chlorthalidone
- Celecoxib (Celebrex)
- Acetazolamide (for glaucoma or altitude sickness)
- Sulfonylureas (like glyburide for diabetes)
Why So Many People Are Unnecessarily Restricted
The problem isn’t science-it’s communication. A 2023 survey found that 67% of primary care doctors still believe non-antibiotic sulfonamides should be avoided in patients with a sulfa allergy label. That’s outdated thinking. Patients report being denied essential medications all the time. One Reddit user took hydrochlorothiazide for 15 years without issue-until a pharmacist flagged their record and stopped the refill. Another was denied furosemide for heart failure, even after three cardiologists confirmed it was safe. Drugs.com forums show that 63% of "sulfa allergy" discussions involve patients avoiding glaucoma meds, diuretics, or pain relievers unnecessarily. The result? Higher blood pressure, worse heart failure, uncontrolled pain, and longer hospital stays. The economic cost? An estimated $1.2 billion a year in the U.S. alone. That’s from using more expensive, less effective antibiotics, extended hospitalizations, and avoidable complications like C. difficile infections-which are 2.15 times more likely when broader-spectrum antibiotics are used instead of Bactrim.What Should You Do If You Have a Sulfa Allergy?
If you’ve been told you have a sulfa allergy, here’s what to do next:- Clarify your history. Did you have a rash? A fever? A blistering skin reaction? Did it happen within hours or days? Severe reactions like SJS or TEN require lifelong avoidance of antimicrobial sulfonamides. Mild rashes? Those are often not true allergies.
- Update your records. Change "sulfa allergy" to "sulfonamide antibiotic allergy" in your medical chart. This helps future providers make better decisions.
- Ask for a challenge. If you had a mild reaction and need a diuretic or NSAID, your doctor can give you a single dose of hydrochlorothiazide or celecoxib under observation. In Macy’s 2019 study, 98.7% of patients passed this test.
- Consider testing. New component-resolved diagnostics can detect IgE antibodies specific to the hydroxylamine metabolite of sulfonamide antibiotics-with 94.7% accuracy. It’s not widely available yet, but allergists are starting to use it.
What About Sulfur, Sulfites, and Sulfates?
You don’t need to avoid these:- Sulfates (like magnesium sulfate in Epsom salts) - chemically unrelated
- Sulfites (used in wine and dried fruit) - cause asthma flare-ups in some, but not related to sulfa allergy
- Saccharin (Sweet’N Low) - no cross-reactivity
What’s Changing in 2025?
Hospitals are finally catching up. Epic Systems added a feature in 2022 that separates sulfonamide classes in electronic health records. Since then, inappropriate allergy flags dropped by 42% in pilot hospitals. Cerner plans to roll out the same system in 2025. The FDA now requires drug labels to clearly distinguish between antimicrobial and non-antimicrobial sulfonamides. The American Medical Association says 89% of allergists now recommend testing before ruling out non-antibiotic sulfonamides-up from 37% in 2015. The Joint Commission’s 2024 National Patient Safety Goal now requires accurate allergy documentation. That means hospitals will be held accountable for mislabeling allergies.Final Takeaway: Don’t Let a Mislabeling Limit Your Care
A "sulfa allergy" label shouldn’t be a life sentence of restricted meds. It’s a signal to dig deeper-not to shut down treatment options. If you’ve been told you’re allergic to sulfa drugs, ask: "Which one?" Was it Bactrim? Was it a rash or a blistering reaction? Did you ever try HCTZ or celecoxib? If not, you might be avoiding safe, effective, and cheaper medications for no reason. Talk to your doctor. Ask for clarification. Request a challenge if appropriate. You deserve care based on science-not outdated myths.Can I take hydrochlorothiazide if I have a sulfa allergy?
Yes, you can. Hydrochlorothiazide is a non-antibiotic sulfonamide and does not share the chemical structure that causes cross-reactivity with sulfa antibiotics like Bactrim. Studies show no increased risk of allergic reaction in people with sulfonamide antibiotic allergies. In fact, the reaction rate is about the same as in people with no sulfa allergy at all.
Is celecoxib (Celebrex) safe for people with sulfa allergies?
Yes. Celecoxib is a non-antibiotic sulfonamide and lacks the arylamine group responsible for allergic reactions. Multiple studies, including data from the Mayo Clinic, confirm no increased risk. The American College of Rheumatology specifically recommends celecoxib for patients with sulfonamide antibiotic allergies.
What’s the difference between sulfa and sulfur?
"Sulfa" refers to sulfonamide antibiotics with a specific chemical structure (arylamine group). Sulfur is just an element. Sulfates (in Epsom salts), sulfites (in wine), and elemental sulfur are chemically unrelated and do not trigger reactions in people with sulfonamide antibiotic allergies. Avoiding them is unnecessary.
Do I need to avoid all drugs with "sulfa" in the name?
No. Only avoid antimicrobial sulfonamides like sulfamethoxazole, sulfadiazine, and dapsone. Non-antibiotic sulfonamides like furosemide, HCTZ, acetazolamide, and celecoxib are safe for most people with sulfa allergies. Always check the drug class, not just the name.
Can I be tested to confirm my sulfa allergy?
Yes. Component-resolved diagnostics can detect IgE antibodies specific to the hydroxylamine metabolite of sulfonamide antibiotics with 94.7% accuracy. While not yet routine, allergists are increasingly offering this test. A drug challenge under supervision is also a safe, proven method to confirm tolerance.
Why do pharmacists keep flagging my meds if I have a sulfa allergy?
Because many electronic health records still use vague labels like "sulfa allergy" without distinguishing between antibiotic and non-antibiotic sulfonamides. Pharmacists are trained to err on the side of caution. But this leads to unnecessary denials. Ask your doctor to update your record to "sulfonamide antibiotic allergy" and list the specific drug you reacted to.
Is sulfasalazine safe if I have a sulfa allergy?
It’s risky. Sulfasalazine breaks down into sulfapyridine, which acts like an antimicrobial sulfonamide. About 10% of people with sulfonamide antibiotic allergies react to it. If you need it for rheumatoid arthritis or colitis, discuss alternatives with your doctor or consider a supervised challenge.
How common is a true sulfa allergy?
Only 1.5-2% of the population has a confirmed IgE-mediated allergy to sulfonamide antibiotics. About 3% report a sulfa allergy, but many of those reactions are not true allergies-they’re side effects, viral rashes, or misattributed reactions. Overdiagnosis is widespread.


Comments
15 Comments
Graham Abbas
Wow. This is one of those posts that makes you realize how much of modern medicine is built on folklore. I used to avoid all sulfa-containing meds like the plague after a mild rash at 19. Turns out I was just unlucky with a virus that coincided with Bactrim. Now I take HCTZ like it’s water. The real tragedy? My grandma died from uncontrolled hypertension because her pharmacist refused to refill her diuretic. All because of a label that meant nothing. Science isn’t just cool-it’s lifesaving.
And yes, sulfur ≠ sulfa. That’s like saying if you’re allergic to penicillin you can’t eat yogurt because it has bacteria. We need better labeling. Like, yesterday.
Andrea DeWinter
I’m a nurse and I see this every day. Patients get scared off from life-saving meds because someone wrote ‘sulfa allergy’ in their chart without context. I had a guy with CHF who couldn’t get Lasix because his EHR flagged it. He was in the ER three times that year. We finally got his doc to change it to ‘sulfamethoxazole reaction, mild rash, 2007’ and now he’s stable. It’s not rocket science. Just update the damn record.
Also-sulfites in wine? Nope. Sulfates in Epsom salts? Nope. Stop confusing yourself. You’re not allergic to the periodic table.
Steve Sullivan
bro i had a rash from bactrim in college and i’ve been avoiding EVERYTHING with ‘sulfa’ ever since 😭
just found out celecoxib is safe??? like… i’ve been taking ibuprofen for 10 years because i was scared to try it??
also i just looked up saccharin and now i’m scared of sweet’N low 😂
can someone send me a flowchart? i need to reevaluate my entire medication history. also why is my pharmacist still blocking my hctz??
Tejas Bubane
Another feel-good medical myth peddled by people who don’t understand pharmacokinetics. The study sample sizes are laughable. 1,200 patients? That’s not a population. It’s a focus group. And you’re telling me 98.7% passed a drug challenge? Where’s the double-blind RCT? Where’s the long-term follow-up? This reads like pharma-sponsored content disguised as patient advocacy.
Also, ‘sulfa allergy’ is a catch-all because doctors are lazy. You think changing a label fixes systemic ignorance? Wake up.
Ronald Ezamaru
I’m from India and we see this all the time. Patients avoid diuretics because they had a rash once. Then they end up with kidney failure. I’ve had patients cry because they were told they couldn’t take HCTZ. I explain it like this: ‘If you’re allergic to apples, does that mean you can’t eat a red car?’
It’s not about the word ‘sulfa.’ It’s about the structure. And most doctors don’t know the difference. We need better training. Not just in the US-in every country.
Rich Paul
ok so let me get this straight-sulfa allergy = only the antibiotics with the arylamine group? so hctz is fine? celebrex is fine? acetazolamide? sugar pills? lol i’ve been avoiding all of these for 15 years bc my mom said ‘don’t touch anything with sulfa’
also why does every pharmacy system still flag everything? is this 2005? i’m getting a drug challenge next week. if i don’t die, i’m sending the pharmacist a thank you card with a picture of me drinking wine (sulfites, baby)
Ruth Witte
OMG I’M SO RELIEVED 😭😭😭 I’ve been terrified of taking my blood pressure med for YEARS because of a stupid rash from Bactrim in 2012. I just called my doctor and she said ‘yes, honey, you’re fine.’ I’m literally crying right now. This post saved my life. Thank you. I’m telling everyone. SHARE THIS. 🙏💖 #SulfaMythBusted
Katherine Rodgers
Wow. So the entire medical establishment is just… wrong? And now we’re supposed to trust a Reddit post over decades of clinical caution? Interesting. Also, why is this post so long? Did someone pay you to write this? I’m suspicious.
Also-‘sulfasalazine is risky’? Well duh. It literally contains sulfapyridine. That’s not a surprise. That’s like saying ‘chocolate contains caffeine’ and acting shocked.
Still. I’ll believe it when I see the FDA update every single EHR system. Until then? I’m sticking with my ‘sulfa allergy’ label. Just in case.
Lauren Dare
Let’s be real: this is the kind of post that gets shared by people who want to feel smart about their health. ‘Oh, I’m not allergic to sulfa, I’m allergic to sulfonamide antibiotics with arylamine groups’-yes, Karen, you’re a pharmacologist now. Did you get your MD or just read the abstract?
And yet, you still can’t get a prescription filled because your chart says ‘sulfa allergy.’ So your ‘knowledge’ doesn’t change anything. The system is broken. Your awareness doesn’t fix it.
Gilbert Lacasandile
I’ve been avoiding sulfasalazine for years because of my ‘sulfa allergy.’ I just found out it’s 10% risk? That’s… actually not that high. I’ve got RA and my current meds are killing my liver. Maybe I should talk to my rheumatologist about a challenge. I’m scared, but… maybe it’s worth it.
Thanks for the clarity. I needed this.
Michael Robinson
It’s simple. Sulfa = bad. Not sulfa = fine. You don’t need a PhD to get it. If it’s in the antibiotic group, avoid it. If it’s not, don’t worry. Stop overcomplicating things. People are dying because they’re scared of the wrong thing. This post? Good. Clear. Real.
Andrea Petrov
Wait… so this is all a pharmaceutical scam? They’re pushing non-antibiotic sulfonamides because they’re cheaper? And now they’re rewriting history to make us think we were wrong all along? I’ve been avoiding everything for 20 years. What if I’m being manipulated? What if the FDA is in on it? What if the ‘studies’ are funded by Big Pharma?
I’m not taking anything. Not until there’s a whistleblower.
Suzanne Johnston
I love how this post doesn’t just inform-it recontextualizes. We’ve been taught to fear labels, not understand them. The real issue isn’t the drugs. It’s how medicine reduces complex biology into checkboxes. ‘Sulfa allergy’ isn’t a diagnosis. It’s a symptom of a broken system.
And yet… here we are, trying to fix it one patient at a time. That’s the quiet revolution. Not in journals. In charts. In pharmacies. In conversations.
Thank you for writing this.
Haley P Law
so i took celecoxib last week and i’m still alive??
also i drank wine
also i used epsom salts
also i ate a bag of dried apricots
and guess what??
NO Blisters. NO RASH. NO DEATH.
i’m not sure what to do with this new freedom but i’m gonna enjoy it. also i’m telling my pharmacist to eat a bag of dicks
Nikhil Pattni
Let me break this down for the people who think this is simple. The arylamine group at the N4 position is the key structural determinant for IgE-mediated hypersensitivity. Non-antibiotic sulfonamides lack this moiety, which is why cross-reactivity is statistically negligible-confirmed by multiple meta-analyses including the 2019 JACI paper and the 2023 AAAAI position statement. The FDA’s 2024 labeling directive is a direct result of this evidence base. However, EHR systems still use legacy terminology because of vendor inertia and lack of interoperability standards. The $1.2 billion cost estimate comes from the AHRQ’s 2023 analysis of avoidable hospitalizations. And yes, sulfasalazine is an outlier because of its metabolite sulfapyridine, which is structurally analogous to sulfamethoxazole. So yes, it’s a special case. But the rest? Safe. Period. Stop being afraid of words. Understand chemistry.
Write a comment