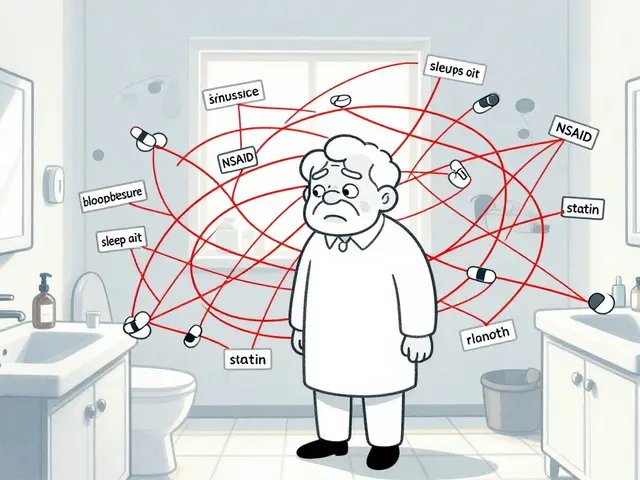
Every year, millions of people in the U.S. take vitamins, herbs, or other dietary supplements without telling their doctor. Many believe these products are harmless because they’re sold over the counter. But here’s the truth: supplement-drug interactions are quietly causing real harm - and most people have no idea.
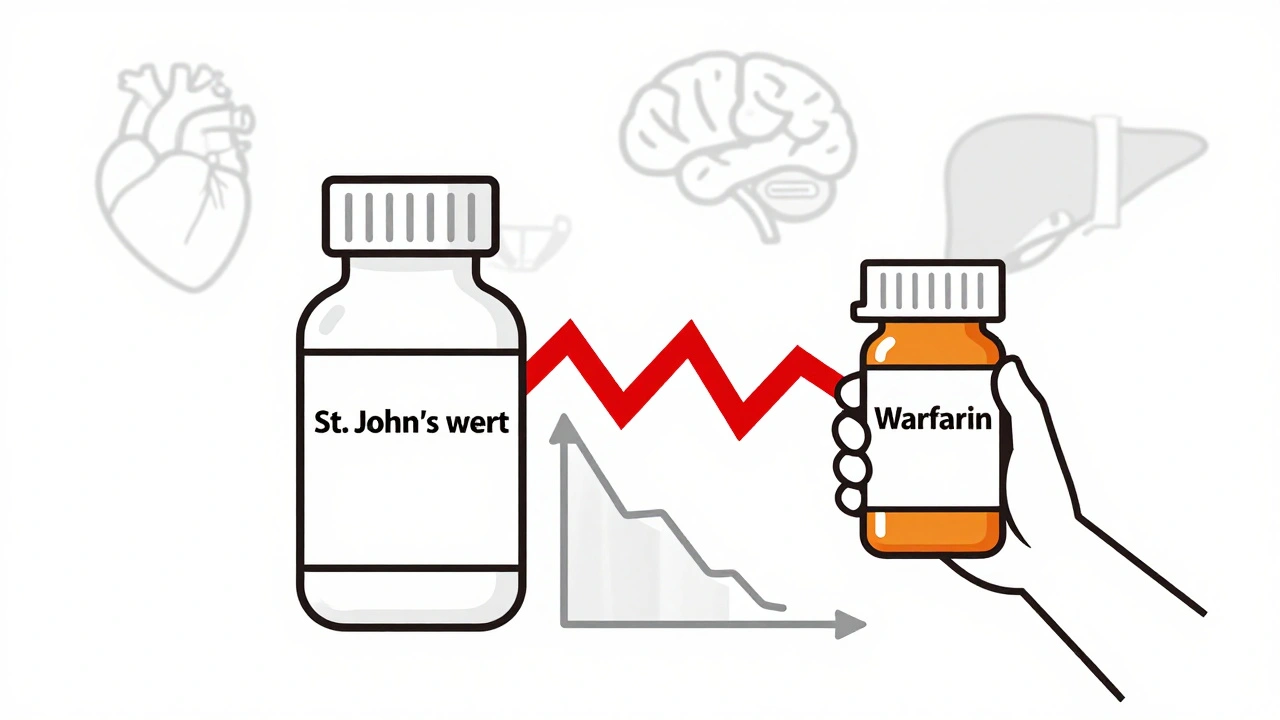
Take St. John’s wort, for example. It’s one of the most popular herbal supplements for mood support. But if you’re on a blood thinner like warfarin, an antidepressant like sertraline, or even a transplant drug like cyclosporine, this seemingly harmless herb can drop your medication levels by more than half. One patient on carbamazepine for seizures saw their drug levels crash after starting St. John’s wort - and ended up having breakthrough seizures. That’s not a rare case. It’s a documented medical emergency.
How Supplements and Drugs Really Interact
Supplements don’t just sit quietly in your body. They actively change how your body handles medications. There are two main ways this happens.
First, pharmacokinetic interactions mess with how your body absorbs, breaks down, or gets rid of a drug. For instance, magnesium in antacids can bind to antibiotics like ciprofloxacin and stop your body from absorbing them - reducing their effectiveness by up to 90%. That means your infection might not clear up, even if you’re taking the right dose.
Second, pharmacodynamic interactions change how the drug works in your body. Vitamin K, found in green tea supplements or leafy greens, directly opposes warfarin’s blood-thinning effect. If you suddenly start taking a vitamin K supplement while on warfarin, your INR (a measure of blood clotting) can drop dangerously low - increasing your risk of stroke or blood clots. On the flip side, ginkgo biloba can make warfarin too strong, pushing INR levels above 6.5 in some cases. That’s not just a lab number - it’s a bleeding risk that can land you in the ER.
The Biggest Culprits
Not all supplements are equal when it comes to risk. Some are harmless. Others? They’re ticking time bombs when mixed with common meds.
- St. John’s wort - Interacts with over 50 medications, including antidepressants, birth control pills, HIV drugs, and heart medications. It tricks your liver into breaking down drugs too fast.
- Ginkgo biloba - Doubles the risk of bleeding when taken with blood thinners like warfarin or aspirin. Case reports show INR spikes from 2.5 to 7.8 after just a few days of use.
- Cranberry - Often thought to be safe, but it can increase warfarin’s effect. One study found patients needed to cut their warfarin dose by nearly 30% after regularly drinking cranberry juice.
- Calcium supplements - If you take levothyroxine for hypothyroidism, calcium can block its absorption by up to 50%. That means you’re not getting the full dose - and your thyroid levels stay off.
- Red yeast rice - Marketed as a natural cholesterol reducer, but it contains lovastatin - the same active ingredient as the prescription drug Mevacor. Combine it with another cholesterol drug like gemfibrozil, and you risk rhabdomyolysis, a condition that destroys muscle tissue and can cause kidney failure.
Herbal supplements make up only 15% of supplement sales, yet they cause 65% of the serious interactions reported to the FDA. Why? Because they’re potent. Unlike synthetic drugs, they’re not standardized. One bottle of goldenseal might have 10 times the amount of berberine as another - and no label tells you which.

Why Doctors Don’t Know - And Why You Should Speak Up
Here’s the uncomfortable truth: most doctors don’t ask about supplements. And most patients don’t volunteer the info.
A 2018 study found that between 43% and 69% of patients don’t tell their doctor about supplement use. Why? Many think it’s not important. Others assume their doctor doesn’t know anything about them. One Reddit user wrote: “My doctor doesn’t know anything about supplements anyway.” That’s exactly the mindset that gets people hurt.
But when doctors do ask - and ask the right way - things change. A 2022 survey showed that 73% of physicians who specifically asked, “What vitamins, herbs, or other supplements do you take?” were able to prevent a dangerous interaction. That’s not luck. It’s practice.
Don’t say “I take some herbal stuff.” Say: “I take St. John’s wort, 300 mg twice a day, from Trader Joe’s.” Write it down. Bring the bottle. Names and doses matter.
The Regulatory Gap
The Dietary Supplement Health and Education Act (DSHEA) of 1994 is the law that lets supplements be sold without proving they’re safe or effective. The FDA can’t block a product unless it’s proven dangerous - and by then, thousands of people may have already taken it.
Compare that to prescription drugs, which go through years of testing before they hit the shelf. Supplements? They can be on the market in weeks. And 20% of them contain ingredients not listed on the label - including hidden prescription drugs, steroids, or stimulants.
Only 0.5% of supplements have published interaction studies. The Natural Medicines Database tracks over 1,500 interactions, but most labels don’t warn you. In fact, 78% of supplement bottles have no interaction warnings - even when the science says they should.
The FDA received over 1,800 reports of supplement-drug interactions between 2019 and 2022. Warfarin interactions made up 32% of those. Antidepressants? 24%. Immunosuppressants? 18%. And that’s just what got reported. Experts say less than 1% of actual adverse events are reported.
What You Can Do Right Now
You don’t need to stop taking supplements. But you do need to take control.
- Make a list - Write down every supplement you take, including brand, dose, and frequency. Don’t forget “natural” products like green tea extract or turmeric capsules.
- Bring it to your next appointment - Show your doctor or pharmacist the actual bottles. Ask: “Could any of these interact with my medications?”
- Check high-risk combinations - If you’re on warfarin, antidepressants, blood pressure meds, or immunosuppressants, assume any new supplement could be risky. Look up your exact combo on the NIH’s LiverTox or Natural Medicines Database.
- Don’t assume “natural” means safe - Just because something comes from a plant doesn’t mean it won’t hurt you. St. John’s wort is a plant. So is poison ivy.
- Report bad experiences - If you have a reaction, report it to the FDA’s MedWatch program. Your report helps others.
There’s no magic pill that makes supplements risk-free. But awareness? That’s powerful. And it’s free.
What’s Changing?
Pressure is building. The FDA is pushing for better labeling. In 2023, a bill called the Dietary Supplement Labeling Act was introduced to require interaction warnings on high-risk products. The National Center for Complementary and Integrative Health (NCCIH) has committed $15.7 million to research by 2025, focusing on older adults and heart patients - the groups most at risk.
But until laws change, the burden is on you. The supplement industry is worth over $52 billion. And it’s growing fast. But safety hasn’t kept up. You’re not just a consumer. You’re a patient. And your safety matters more than any marketing claim.
If you’re taking even one prescription drug - especially for heart disease, depression, seizures, or organ transplants - don’t assume your supplement is harmless. Ask. Check. Document. Speak up. Your life might depend on it.
Can I take vitamin D with my blood pressure medication?
Yes, vitamin D generally doesn’t interact with common blood pressure medications like lisinopril, metoprolol, or amlodipine. However, if you’re taking calcium supplements along with vitamin D, that combination can raise calcium levels too high - which may affect kidney function or interfere with certain heart medications. Always check with your provider if you’re on multiple supplements or have kidney issues.
Is it safe to take melatonin with antidepressants?
Melatonin can interact with certain antidepressants, especially SSRIs like fluoxetine or sertraline, and SNRIs like venlafaxine. It may increase drowsiness or, in rare cases, raise serotonin levels too high, leading to serotonin syndrome - a potentially dangerous condition. If you’re taking antidepressants, talk to your doctor before starting melatonin, even if it’s “natural.”
Why don’t supplement labels warn about drug interactions?
Under current U.S. law (DSHEA), supplement manufacturers aren’t required to prove safety or test for interactions before selling products. They also don’t have to include interaction warnings on labels - even when science shows clear risks. Only about 12% of major supplement companies conduct formal interaction studies. That means most labels are silent, even when danger exists.
Can I take fish oil with aspirin?
Fish oil has mild blood-thinning effects, and so does aspirin. Taking them together can increase your risk of bleeding, especially if you’re also on warfarin or have a bleeding disorder. It’s not always dangerous - but it needs monitoring. If you’re on daily aspirin for heart health and want to add fish oil, talk to your doctor first. They may check your INR or platelet function.
Do I need to stop supplements before surgery?
Yes. Many supplements - especially ginkgo, garlic, ginger, green tea, and St. John’s wort - can increase bleeding risk or interfere with anesthesia. Surgeons typically ask patients to stop all supplements at least 1-2 weeks before surgery. Don’t assume your surgeon knows what you’re taking. Bring your list and ask: “Which of these do I need to stop?”
Are there any supplements that are safe with almost all medications?
Some supplements have very low interaction risk, like vitamin C in standard doses (under 1,000 mg/day), B-complex vitamins (without high-dose B6), and magnesium oxide (if you’re not on antibiotics). But even these aren’t risk-free for everyone. For example, high-dose vitamin C can interfere with certain cancer drugs. Always check with your provider - especially if you’re on chemotherapy, immunosuppressants, or thyroid meds.
If you’re taking any prescription or over-the-counter medication, don’t treat supplements like candy. They’re powerful substances - and they can change how your drugs work. The safest choice isn’t to avoid them entirely. It’s to know exactly what you’re taking - and who to tell about it.


Comments
15 Comments
Annie Gardiner
Okay but have you ever actually met someone who died from a supplement? I mean, sure, St. John’s wort messed with someone’s seizure meds - but that’s like blaming a spoon for being too pointy when you stab yourself with it. People just don’t take responsibility anymore. It’s not the supplement’s fault. It’s the person who didn’t read the tiny print.
Rashmi Gupta
In India, we’ve been using turmeric and ashwagandha for 5000 years. Your ‘science’ is still catching up. Why do you assume Western medicine knows everything? We don’t need your FDA to tell us what’s safe. Our grandmothers knew better.
Kumar Shubhranshu
St John’s wort reduces drug levels by 50%? That’s not a interaction. That’s a betrayal. And you’re surprised?
Mayur Panchamia
This is why America is collapsing! You people take pills like candy and then blame the supplement industry! We in India don’t need your overregulated, over-labeled, over-medicated nonsense! We take neem, tulsi, and ginger - and we don’t need a 12-page warning label to know what’s good for us!
Kenny Pakade
I’ve been taking fish oil and aspirin for 8 years. Never bled. You’re just fearmongering. This article reads like a pharmaceutical ad. Who funded this?
Gwyneth Agnes
If you can’t be trusted to tell your doctor what you’re taking, you don’t deserve to live.
Ashish Vazirani
Let me tell you about my cousin’s uncle’s neighbor - he took red yeast rice because he heard it was ‘natural’ - and guess what? He ended up in the ICU with rhabdo. His kidneys failed. His wife cried for three days. The label didn’t say a word. Not one word. And now? He’s on dialysis. And the company? Still selling it. On Amazon. With 4.8 stars. People are dying because corporations don’t care. And you? You’re still scrolling.
Kay Jolie
It’s fascinating how the pharmacokinetic modulation of CYP3A4 isoforms by hyperforin - the primary alkaloid in St. John’s wort - creates a clinically significant induction cascade that downregulates P-glycoprotein transporters, thereby reducing serum concentrations of concomitant therapeutics. The regulatory lacuna under DSHEA is not merely a legal gap - it’s a systemic epistemic failure in risk communication. We’re not just talking about pills. We’re talking about the commodification of biological ignorance.
Max Manoles
I appreciate the depth of this post. I work as a clinical pharmacist and see this every week. One patient took calcium with levothyroxine - her TSH went from 2.1 to 14.8 in three weeks. She thought ‘it’s just a pill’ - and didn’t realize it was blocking absorption. We need more of these conversations. Not fear. Just clarity. Bring your bottles. Write down the names. Ask. It takes two minutes. It could save your life.
Arjun Deva
Did you know the FDA gets paid by supplement companies to ‘review’ safety? That’s why only 0.5% have studies. That’s why they don’t force labels. That’s why your ‘natural’ vitamin D has heavy metals in it. This isn’t negligence - it’s collusion. The whole system is rigged. The FDA, the manufacturers, even your doctor - they’re all in on it. They want you dependent. They want you buying more. Wake up.
Priya Ranjan
You’re all so naive. You think supplements are the problem? The real problem is that people think they can ‘self-diagnose’ with a Google search and then pop pills like candy. I’ve seen a woman take 10 different supplements for ‘anxiety’ while on SSRIs - and then wonder why she felt like a zombie. If you don’t have a degree in pharmacology, you shouldn’t be mixing anything. Period. Stop being a lab rat for the supplement industry.
Katie O'Connell
It is, without question, a matter of profound public health concern that the regulatory framework governing dietary supplements remains fundamentally incongruent with the pharmacological potency of many of their constituents. The absence of mandatory interaction labeling constitutes, in my estimation, a de facto abdication of the state’s duty to protect the citizenry from iatrogenic harm.
Clare Fox
idk man i just take my turmeric and my fish oil and my magnesium and i feel fine. maybe the real issue is that we’ve been taught to fear everything. what if the body knows what to do? maybe we’re just overthinking it. i mean, plants have been healing people for thousands of years. why do we need a lab to tell us what’s safe?
Akash Takyar
Thank you for sharing this. It’s so important to speak up. Many people feel embarrassed to talk about supplements - but your honesty helps others. If you’re taking anything, even a ‘simple’ vitamin - tell your doctor. Write it down. Bring the bottle. You’re not being a burden. You’re being smart. And that’s something to be proud of.
Nigel ntini
I’ve worked with older patients in the UK for 15 years. The biggest risk isn’t the supplement - it’s the silence. One woman took ginkgo with warfarin for 6 months. Never told anyone. Had a brain bleed. She survived. But she cried for weeks because she thought ‘it was just a herb.’ We need to normalize asking. Not judging. Just asking. ‘What else are you taking?’ It’s the simplest thing - and it saves lives.
Write a comment