It’s easy to think of herbal teas as harmless, even healthy. A warm cup of chamomile before bed, ginger for digestion, or hibiscus for a tart boost - these feel like gentle, natural choices. But what if that cup of tea is quietly changing how your blood pressure medicine, blood thinner, or antidepressant works in your body? The truth is, herbal teas aren’t just flavorings. They’re bioactive substances that can interfere with prescription drugs in ways that are serious, sometimes life-threatening - and most people have no idea.
Why Herbal Teas Aren’t Just ‘Herbal Water’
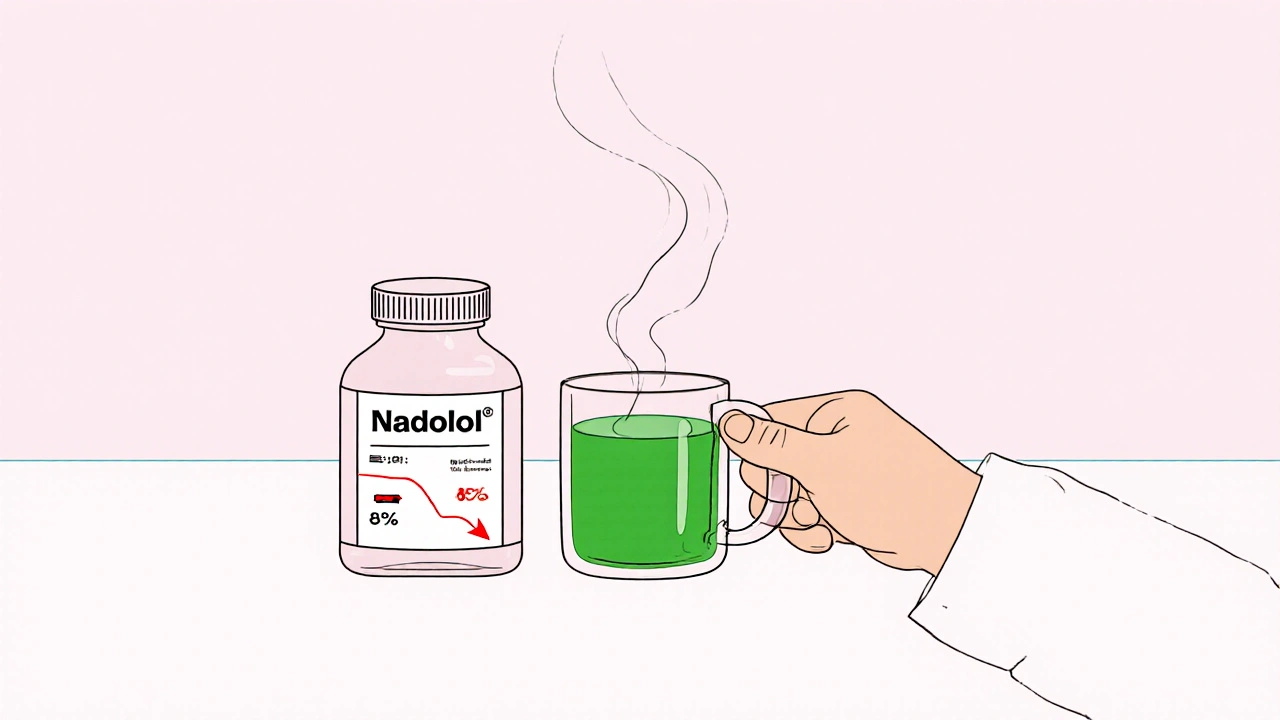
Unlike regular tea made from the Camellia sinensis plant, herbal teas come from roots, flowers, seeds, or leaves of other plants. That means they contain complex chemical compounds - things like flavonoids, alkaloids, and polyphenols - that your body treats like medicine, not just tea. These compounds don’t just float through your system. They interact with enzymes, transporters, and receptors that handle your prescription drugs. For example, green tea contains epigallocatechin gallate (EGCG), a powerful antioxidant. In test tubes, EGCG blocks the same protein transporters that move drugs like atorvastatin (Lipitor) and nadolol (a beta-blocker) into your bloodstream. A 2023 clinical study found that drinking three strong cups of green tea daily cut nadolol levels in the blood by 85%. That’s not a small drop. It means the drug isn’t working - and your heart rate or blood pressure could spike without warning.The Top 5 Herbal Teas That Can Clash With Medications
Not all herbal teas carry the same risk. But these five are backed by real clinical evidence and have caused documented problems:- St. John’s wort tea: This one is dangerous with antidepressants, birth control pills, and even some heart medications. It activates liver enzymes that break down drugs too fast. If you’re on sertraline, fluoxetine, or cyclosporine, this tea can make your meds useless. People have ended up in the hospital because they thought ‘natural’ meant safe.
- Green tea: Beyond the nadolol and statin issues, green tea can interfere with blood thinners, chemotherapy drugs, and even some antibiotics. The problem isn’t just caffeine - it’s the EGCG. Even one cup a day can matter if you’re on a narrow-therapeutic-index drug.
- Hibiscus tea: Popular for its tart flavor and supposed blood pressure-lowering effects, hibiscus acts like an ACE inhibitor. When combined with lisinopril, enalapril, or other blood pressure pills, it can push your systolic pressure below 90 mmHg. That’s not a bonus - it’s dizziness, fainting, and risk of falls.
- Ginkgo biloba tea: Often taken for memory, ginkgo thins the blood. When mixed with warfarin (Coumadin), aspirin, or clopidogrel, it increases bleeding risk. There are documented cases of brain bleeds and eye hemorrhages in people who drank ginkgo tea daily while on anticoagulants.
- Chamomile tea: It’s soothing, yes - but chamomile contains apigenin, which can mess with how your body metabolizes birth control pills and some anti-anxiety meds. One small study suggested it might reduce the effectiveness of oral contraceptives, leading to unintended pregnancies.
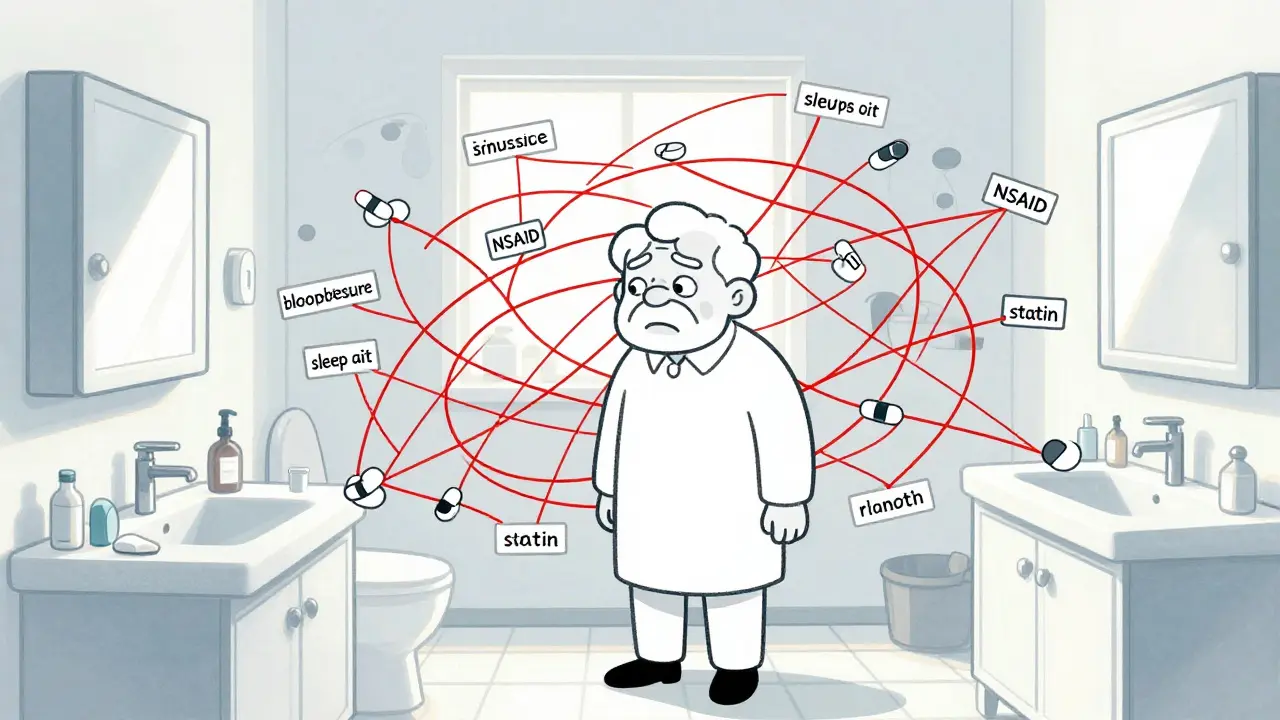
Who’s at the Highest Risk?
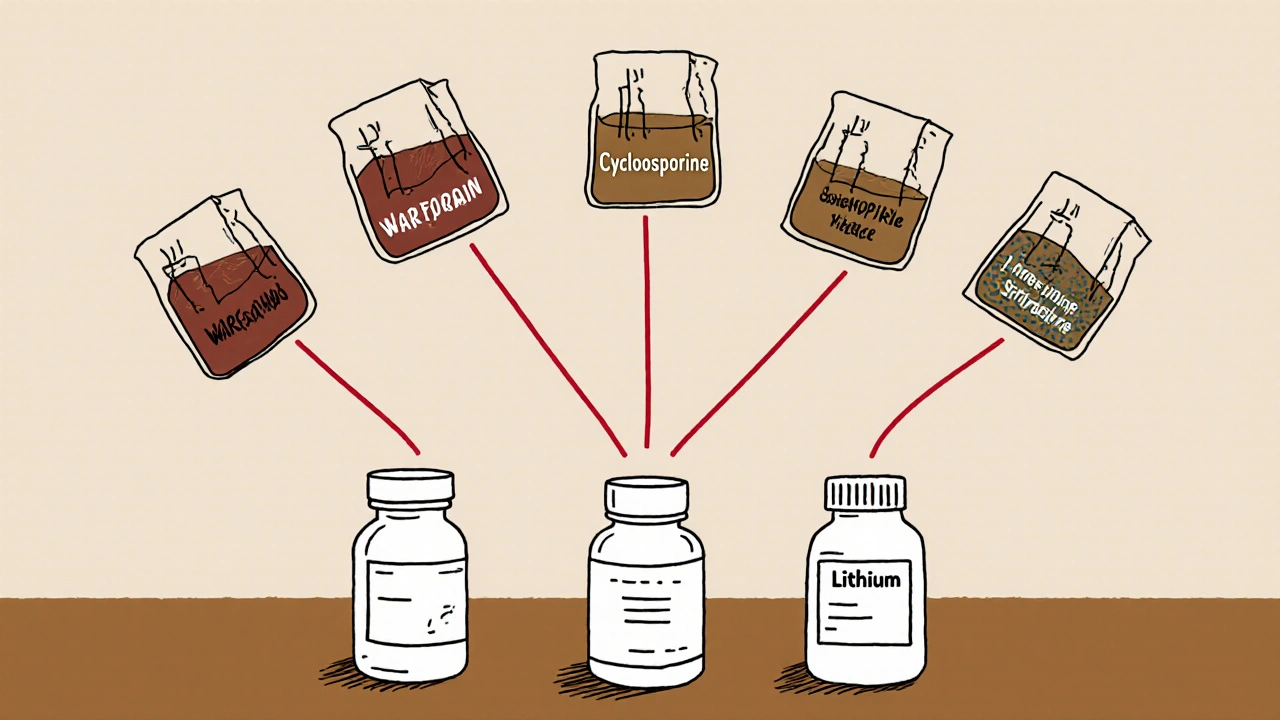
This isn’t just about older people taking a few pills. Anyone on certain types of medications should treat herbal teas like a drug - not a snack. People on these drugs need to be especially careful:- Warfarin (blood thinner): Ginkgo, ginger, garlic, and chamomile all increase bleeding risk.
- Digoxin (heart medication): Licorice root tea can lower potassium, which makes digoxin toxic.
- Cyclosporine (transplant drug): St. John’s wort and green tea can slash its levels, risking organ rejection.
- Theophylline (asthma): Green tea can raise theophylline levels dangerously, causing seizures or heart rhythm problems.
- Lithium (mood stabilizer): Diuretic herbs like dandelion or hibiscus can cause lithium to build up to toxic levels.
What About ‘Functional’ Tea Blends?
The market is flooded with teas labeled “immune support,” “stress relief,” or “detox.” These often contain 5, 7, or even 12 different herbs. One blend might have hibiscus, ginger, licorice, and chamomile - all in one cup. That’s a cocktail of potential interactions. There’s no regulation requiring these blends to be tested for safety with medications. A 2023 FDA report noted that over 70 warning letters were sent to supplement makers in just two years for making illegal drug claims. If a tea says it “lowers blood pressure,” it’s already acting like a drug - and you shouldn’t drink it while on BP meds.
What Should You Do?
You don’t need to give up herbal tea. But you need to be smart. Here’s what to do right now:- Make a list. Write down every herbal tea you drink, how often, and how strong (e.g., “2 cups of chamomile at night,” “1 cup hibiscus in the morning”).
- Bring it to your next appointment. Don’t wait for your doctor to ask. Say: “I drink these teas - do any of them interfere with my meds?”
- Know your high-risk drugs. If you’re on warfarin, digoxin, cyclosporine, theophylline, or lithium, avoid St. John’s wort, green tea, hibiscus, and ginkgo unless your doctor says it’s safe.
- Don’t assume ‘organic’ or ‘natural’ is safe. The FDA doesn’t test supplements before they’re sold. A product labeled “pure” could still contain contaminants or interact with your meds.
- When in doubt, pause. If you’re starting a new medication, hold off on new herbal teas for a week or two. Watch for changes - dizziness, unusual bruising, heart palpitations, or feeling like your meds aren’t working.
The Bottom Line
Herbal teas aren’t the enemy. But treating them like harmless background noise is dangerous. They’re active substances - and they can change how your medications work. The science is clear on several key herbs. The risk isn’t theoretical. People have had strokes, organ rejections, and uncontrolled bleeding because they didn’t realize their tea was interfering with their pills. If you’re taking any prescription medication, especially for heart, brain, or immune conditions, your herbal tea isn’t just a comfort - it’s a variable in your treatment plan. Talk to your doctor. Bring your tea bag. Ask the question. It could save your life.Can I still drink herbal tea if I’m on blood thinners?
You can, but you need to avoid certain types. Ginkgo biloba, chamomile, ginger, and garlic teas can increase bleeding risk when combined with warfarin or aspirin. Hibiscus tea may also interfere. Stick to plain peppermint, rooibos, or caffeine-free fruit teas unless your doctor approves otherwise. Always monitor for unusual bruising or bleeding.
Does green tea interfere with cholesterol meds?
Yes. Green tea, especially in strong or concentrated forms, can reduce the absorption of statins like atorvastatin and simvastatin by up to 39%. If you’re on a statin, drinking more than one cup of strong green tea daily could make your medication less effective. Switch to rooibos or chamomile in the morning if you take your statin at night.
Is it safe to drink herbal tea while taking antidepressants?
Not if it contains St. John’s wort. This herb speeds up how your liver breaks down many antidepressants, including SSRIs like sertraline and fluoxetine, making them ineffective. It can also cause serotonin syndrome - a dangerous condition with high fever, confusion, and rapid heart rate. Avoid St. John’s wort tea completely if you’re on any antidepressant.
Can herbal tea affect my birth control?
Yes. Chamomile tea has been shown in early studies to interfere with the enzymes that process estrogen in birth control pills. While more research is needed, the risk is real enough that experts advise caution. If you rely on hormonal birth control, avoid daily chamomile tea or switch to a non-herbal alternative.
Why don’t pharmacists warn me about herbal teas?
Because most people don’t tell them they’re drinking herbal tea. Pharmacists only see what’s on your prescription list - not your tea cabinet. Herbal teas aren’t classified as drugs, so they’re not flagged in pharmacy systems. It’s up to you to disclose them. Always say: “I drink this tea every day.”
Are there any herbal teas that are generally safe with medications?
Rooibos, fruit teas (like apple or berry), and plain peppermint are generally low-risk for interactions. They don’t contain the potent compounds found in St. John’s wort, ginkgo, or green tea. But even these can be risky if you’re on multiple medications or have kidney or liver disease. When in doubt, ask your doctor.


Comments
13 Comments
Bailey Sheppard
This is one of those posts that makes you pause and rethink everything you thought was harmless. I used to drink three cups of green tea a day thinking I was being healthy. Turns out I was probably sabotaging my blood pressure meds without even knowing it. Scary stuff.
Thanks for laying it out so clearly. I’m going to print this out and bring it to my next appointment.
Girish Pai
India has been using herbal infusions for millennia - Ayurveda doesn’t operate on FDA-approved clinical trials. You Westerners treat plants like chemical cocktails, but we know their energetic signatures. This fear-mongering is colonial science disguised as caution.
My grandmother drank hibiscus with her antihypertensives for 40 years. She’s 92 and still walks 5k daily. Your pharmacokinetic models are reductive.
Kristi Joy
Thank you for writing this. I know so many people who think ‘natural’ = ‘no side effects.’ It’s not just about safety - it’s about respect. Your body is doing complex work, and herbs are powerful tools, not snacks.
If you’re on meds, treat your tea like a prescription. Write it down. Talk to your provider. No shame in asking. We’re all learning together.
Hal Nicholas
Of course this is true. The FDA doesn’t regulate herbs because Big Pharma doesn’t want you to know you can replace their $500 pills with something from your backyard.
St. John’s wort is cheaper than Zoloft. Ginkgo beats Plavix. They’re hiding this from you. The system doesn’t want you healthy - it wants you dependent.
And now they’re calling it ‘dangerous’ to scare you away from real medicine. Wake up.
Louie Amour
Look, I’ve read the literature. The interactions aren’t just theoretical - they’re documented in peer-reviewed journals. If you’re drinking hibiscus tea while on lisinopril and you’re not monitoring your BP, you’re playing Russian roulette with your cerebellum.
And yes, I’m calling you out if you’re one of those people who says ‘I’ve been doing it for years.’ That’s not a safety record - that’s luck. And luck runs out.
Kristina Williams
Did you know the government puts fluoride in the water to make you forget how dangerous herbs are? They don’t want you connecting the dots. Chamomile tea? That’s a mind-control agent disguised as relaxation. They’ve been suppressing this for decades.
And why do you think they call it ‘herbal tea’ instead of ‘herbal drug’? To confuse you. It’s all a setup. I saw a video on YouTube where a guy in a lab coat admitted it.
Christine Eslinger
There’s a difference between traditional use and pharmacological interaction - and this post nails it. Just because something’s been used for centuries doesn’t mean it’s safe with modern pharmaceuticals.
St. John’s wort induces CYP3A4 and P-glycoprotein, which is why it tanks cyclosporine levels in transplant patients. That’s not folklore - it’s biochemistry.
But the real issue isn’t the herbs. It’s the lack of patient education. Doctors don’t ask. Pharmacists don’t probe. Patients don’t volunteer. And that’s the systemic failure.
Bring your tea bag. Write it down. Say it out loud. Your life might depend on it.
Shaun Barratt
It is worth noting that the bioavailability of EGCG in green tea is highly variable depending on brewing temperature, steeping time, and leaf quality. A single cup of loose-leaf, 85°C, 5-minute brew may deliver 150–200 mg EGCG, whereas a tea bag steeped for 2 minutes at 70°C may yield less than 50 mg.
Therefore, the 85% reduction in nadolol levels cited in the 2023 study likely applies to concentrated, high-dose intake - not casual consumption.
Context matters. Overgeneralization risks unnecessary alarm.
Iska Ede
So let me get this straight - drinking tea is now a felony if you take meds? Cool. Next they’ll ban sunlight because it interferes with antidepressants.
Also, why is everyone suddenly so scared of plants? Did we forget that humans evolved eating them? I’m going to drink chamomile tea while on birth control and let the universe sort it out. Namaste, y’all.
Gabriella Jayne Bosticco
I’ve been on warfarin for 7 years. I drink rooibos every morning. I avoid ginkgo, chamomile, and ginger. I check my INR monthly. Simple.
It’s not about fear. It’s about awareness. You don’t need to give up tea - just know what’s in it. And if you’re unsure? Ask. Your pharmacist will appreciate you for it.
Gabe Solack
Just want to say thank you for this. I’m on lithium and was drinking dandelion tea every day thinking it was a ‘detox’ thing. Turns out it was probably raising my lithium levels. I stopped it yesterday.
Also, I’m now showing my mom this post. She’s 71, on 5 meds, and drinks 3 herbal teas a day. She thinks it’s ‘just tea.’ 😅
Small changes save lives.
Yash Nair
India has 5000 years of herbal wisdom and you think some American study tells you what’s safe? You people drink bottled water and call it healthy. We drink neem tea to cure diabetes. You drink chamomile and call it self-care.
Stop pretending your science is better than our tradition. Your pills are poison. Our herbs are truth.
Shilpi Tiwari
Let’s talk about CYP450 polymorphisms. The risk isn’t uniform. Someone with CYP2D6 ultrarapid metabolizer status will clear SSRIs faster - so St. John’s wort’s effect is amplified. But someone with poor metabolizer status? Might not even notice.
Also, ginkgo’s antiplatelet effect is dose-dependent. One cup of weak tea? Negligible. Two cups of concentrated extract? High risk.
It’s not black and white. It’s pharmacogenomics. We need personalized guidance, not blanket warnings.
Write a comment