Specialty medications and injectables are saving lives-but they’re also breaking budgets. These drugs treat serious conditions like cancer, rheumatoid arthritis, and MS, but they often cost more than $1,000 a month. Even if you have insurance, your out-of-pocket bills can still be crushing. The truth? You’re not alone. Employers, insurers, and patients across the U.S. are scrambling to find ways to bring these costs down without sacrificing care. The good news? There are proven, practical strategies that work-right now.
Use Formulary Management to Avoid Unnecessary Spending
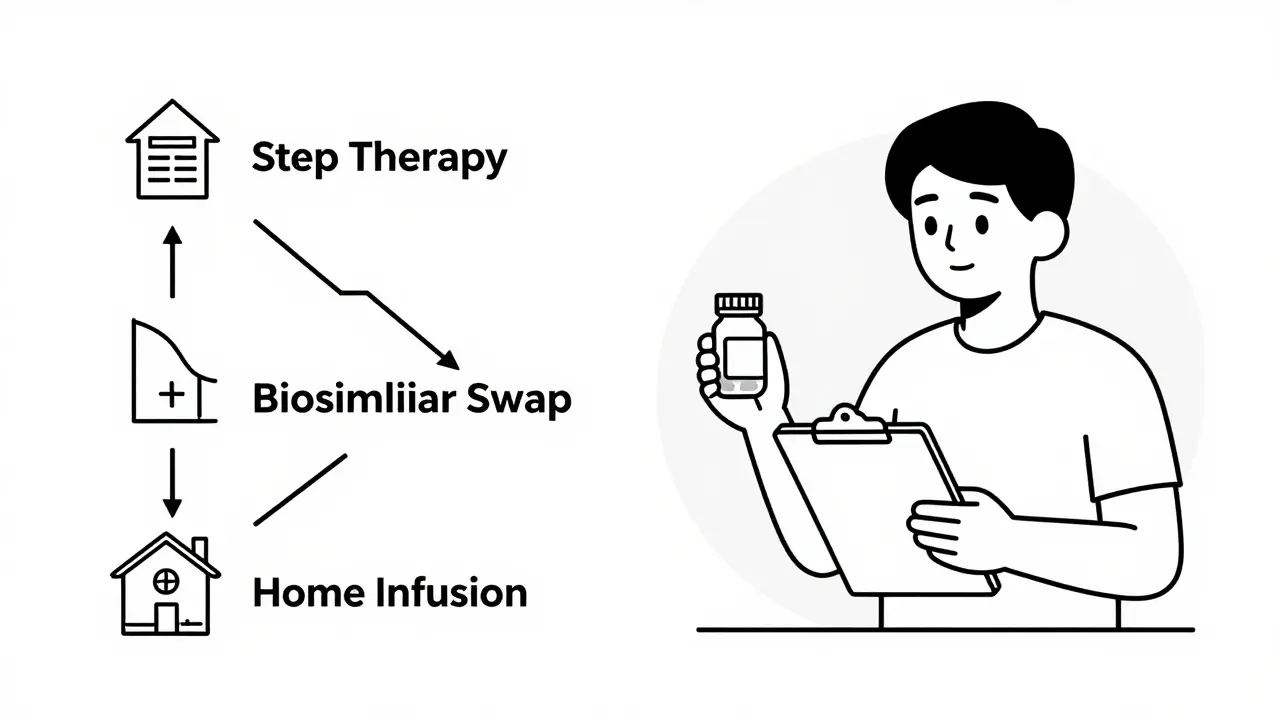
Most insurance plans have a list of preferred drugs called a formulary. But not all formularies are created equal. Some let you get any drug you ask for, no questions asked. Others use step therapy and prior authorization to make sure you’re on the most cost-effective option that still works. For example, if you’re prescribed a new GLP-1 weight loss drug that costs $1,200 a month, your plan might first require you to try a cheaper, equally effective alternative. If that doesn’t work, then they approve the expensive one. This isn’t about denying care-it’s about preventing waste. A study by Excellus BlueCross BlueShield found this approach saved $13.64 per member per month on just one class of drugs. That adds up fast across thousands of people. The key? Make sure your plan’s formulary is actively managed by pharmacists, not just automated systems. Look for plans that have a Pharmacy and Therapeutics (P&T) committee reviewing drugs quarterly. These committees check clinical data, cost, and real-world outcomes before adding or removing a drug. If your employer or insurer doesn’t have one, ask why.Switch to a Narrow Pharmacy Network
Not all pharmacies are the same when it comes to specialty drugs. Some pharmacies specialize in handling complex injectables-like those requiring refrigeration, special training, or patient coaching. These specialty pharmacies often have contracts with drug makers that give them lower prices. By limiting your plan to just a few of these top-tier specialty pharmacies, insurers can negotiate better rates. CarelonRx found that narrowing networks cuts costs by 10-15%. That means the same drug, same dose, same delivery-but you pay less. The catch? You might have to switch pharmacies. If your current pharmacy isn’t in the network, you’ll get a letter explaining the change. Don’t panic. These networks are chosen because they offer better support: free delivery, 24/7 nurse hotlines, refill reminders, and even help with insurance paperwork. One patient told us she saved $400 a month and got a nurse calling her every week to check on side effects. That kind of service isn’t available at your corner drugstore.Ask About Biosimilars-They’re Not Just Cheaper, They’re Just as Good
Biosimilars are the equivalent of generic drugs-but for biologics. Biologics are complex, made from living cells, and used in treatments like rheumatoid arthritis or Crohn’s disease. They’re expensive because they’re hard to copy. But biosimilars? They’re scientifically proven to work the same way, with the same safety profile. The FDA approves them after rigorous testing. And they cost about half as much. Quantum Health reports biosimilars can save $180 billion over five years across the entire U.S. healthcare system. Yet only 30% of eligible patients are using them. Why? Fear. Misinformation. Some doctors still think they’re “inferior.” But that’s outdated. Hospitals that switched to biosimilars saw 20-30% cost reductions-with no drop in patient outcomes. If your doctor prescribes a brand-name biologic, ask: “Is there a biosimilar available?” If they say no, ask for a second opinion. Many patients who switched reported no difference in how they felt-just a lower bill.
Move Infusions Out of the Hospital
Many injectables aren’t just taken at home-they’re given in a hospital infusion center. That’s expensive. A single infusion in a hospital can cost $1,500. The same treatment in a doctor’s office? Around $800. At home, with a trained nurse? As low as $400. Quantum Health studied 220 specialty drugs and found that 91% of patients who could safely receive treatment outside a hospital saved 48% on costs. That’s not a guess-it’s real data from 1.8 million patients. Ask your provider: “Can this be given in my doctor’s office or at home?” Most conditions that require infusions-like IV antibiotics, immune therapies, or iron infusions-can be safely managed outside the hospital. Home infusion services now include everything: equipment delivery, nurse visits, monitoring, and 24/7 support. It’s safer, more comfortable, and far cheaper.Use Financial Assistance Programs-The Right Way
Drug makers often offer copay cards to help patients pay for expensive meds. Sounds great, right? But here’s the catch: many insurance plans don’t count those payments toward your deductible or out-of-pocket maximum. That means you’re still paying the full cost of your plan, even if your copay card says “$0.” That’s where copay maximizer programs come in. These programs let your copay assistance go toward your deductible instead of just covering the copay. So if your drug costs $1,200 and your copay card covers $1,000, that $1,000 counts toward your deductible. Next month, when you need another dose, you’re closer to hitting your out-of-pocket max-and your insurance kicks in sooner. CarelonRx found that when these programs are properly structured, patients end up with $0 out-of-pocket costs-and employers pay less too. It’s a win-win. But you have to ask for it. Don’t assume your plan offers it. Call your insurer and say: “Do you have a copay maximizer program for specialty drugs?”Push for Value-Based Contracts
What if you only paid for a drug if it worked? That’s the idea behind value-based contracts. Instead of paying the full price upfront, the drug maker agrees to refund part of the cost if the drug doesn’t help you. Prime Therapeutics reports a 45% jump in these types of agreements over the past year. They’re still rare-but growing fast. If your employer or insurer is negotiating a contract for a new high-cost drug, ask if they’re including a performance clause. For example: “If the drug doesn’t reduce your inflammation markers after 6 months, we get a 50% rebate.” It’s not magic. It’s accountability. And it’s starting to show up in cancer treatments, MS drugs, and even rare disease therapies. If your plan doesn’t offer this yet, it’s not because it’s impossible-it’s because no one asked.
Combine Strategies for Maximum Savings
No single trick cuts costs enough on its own. But when you stack them? That’s when the real savings happen. For example: Use a narrow pharmacy network to get lower prices. Switch to a biosimilar. Get your infusion at home. Use a copay maximizer. And push for value-based pricing. Together, these steps can cut your total drug spending by 40-60%. Employers who use four or more of these strategies are seeing specialty drug cost growth drop from 10-12% per year to just 5-7%. That’s a $45-60 billion industry-wide savings by 2027. It’s not about cutting corners. It’s about cutting waste. And you have more power than you think.What You Can Do Right Now
- Call your insurer and ask: “Do you use a specialty pharmacy network? Which ones?”
- Ask your doctor: “Is there a biosimilar for this drug?”
- Request: “Can this injection be done at home or in an outpatient clinic?”
- Ask: “Do you have a copay maximizer program?”
- If you’re an employer: Push for value-based contracts and P&T committees.
Are biosimilars safe to use instead of brand-name biologics?
Yes. Biosimilars are approved by the FDA after rigorous testing to prove they work the same way as the original drug-with no meaningful differences in safety, purity, or potency. Hospitals and clinics that have switched to biosimilars report the same patient outcomes, with 20-30% lower costs. Over 42 biosimilars are now approved in the U.S., and their use is growing fast.
Why does my copay card say $0 but my bill is still high?
Many copay cards only cover your copay amount, but don’t count toward your deductible or out-of-pocket maximum. That means you’re still paying the full cost of your insurance plan. A copay maximizer program fixes this by letting the card payment count toward your deductible, so you reach your out-of-pocket limit faster. Ask your insurer if they offer this.
Can I get my injectable medication delivered to my home?
Yes, for many injectables. Home infusion services are now common for drugs like IV antibiotics, immune therapies, and iron infusions. These services include delivery of equipment, trained nurses to administer the drug, and 24/7 support. Costs are typically 40-50% lower than hospital infusions. Ask your doctor or pharmacist if your drug qualifies.
Do prior authorizations delay my treatment?
Sometimes, but not always. When done right, prior authorizations prevent you from getting a drug that won’t work or is unnecessarily expensive. Plans with active Pharmacy and Therapeutics committees can approve most requests within 24-48 hours. One study found 98% of specialty drug requests were approved even with prior authorization in place-and patient adherence actually improved because of better clinical support.
Is it worth switching pharmacies just to save money?
If your current pharmacy isn’t part of a specialty network, yes. Specialty pharmacies offer more than just lower prices-they provide free delivery, nurse support, refill reminders, and help with insurance paperwork. Patients using these networks report higher satisfaction and better adherence. The transition takes a few weeks, but the long-term savings and support make it worth it.



Comments
10 Comments
Art Van Gelder
Okay so let me get this straight-you’re telling me if I just switch pharmacies and ask my doctor if there’s a biosimilar, I could save like half my monthly drug bill? And they send a nurse to my house to give me the shot? That’s wild. I’ve been paying $1,400 a month for my RA med and never even thought to ask. I feel like I’ve been walking around with a blindfold on. Why isn’t this on every insurance website? Why isn’t this on TV? Why do we make healthcare so damn complicated when the fixes are this simple?
Johnnie R. Bailey
There’s a quiet revolution happening in specialty drug access, and it’s not being led by CEOs or lobbyists-it’s being led by patients who asked one question: ‘Is there another way?’ The real innovation isn’t in the science-it’s in the system design. Formularies that listen. Networks that care. Contracts that tie payment to outcomes. We’ve been conditioned to think cost = quality, but that’s a myth. The data shows otherwise. The challenge isn’t finding cheaper drugs-it’s finding the courage to demand better structure.
Nader Bsyouni
Biosimilars are just corporate lies to make pharma look good while they keep raking in cash the same way they always did lol
Julie Chavassieux
I switched to a biosimilar... and my insurance STILL didn't cover it... and then my nurse called me at 2am because I had a reaction... and I cried... and then I got a bill for $800... I'm done.
Ajay Brahmandam
Just talked to my pharmacist yesterday-she showed me how my copay card wasn’t counting toward my deductible. I had no idea. We called my insurer, they fixed it in 10 minutes. Now I’m $1,200 closer to hitting my out-of-pocket max. Small move. Huge difference. Don’t assume anything. Always ask.
jenny guachamboza
I think this is all a ploy by Big Pharma to get us to take cheaper drugs so they can raise prices later 😳💸 they already know we’ll take anything if it’s labeled ‘FDA approved’... also my cat thinks I’m being watched by the insurance company 👀
Jim Brown
The fundamental tension in healthcare economics lies not in the cost of molecules, but in the alignment of incentives. When reimbursement structures reward volume over value, innovation becomes distorted. The strategies outlined herein-narrow networks, value-based contracting, biosimilar adoption-represent not merely cost-containment measures, but a reorientation toward patient-centered stewardship. This is not radical. It is restorative.
Jamison Kissh
What’s interesting is how much of this depends on patient advocacy. The system doesn’t change unless someone speaks up. I didn’t know about copay maximizers until my mom asked during her MS infusion appointment. She was 72. She didn’t even know how to use Zoom, but she called the insurer and demanded answers. That’s the real power here-not the tech, not the contracts-it’s the person who refuses to stay silent.
Vikrant Sura
All this talk about savings but no one mentions how long it takes to get prior auth approved. My sister waited 3 weeks for her chemo drug. She almost died waiting. So yeah, save money but what about the people who can't wait?
Cara Hritz
I used a copay maximizer and it worked but my doctor said the biosimilar was ‘not as good’ even though the FDA says it is so idk what to believe anymore
Write a comment